Skin Resurfacing
Fritz E. Barton
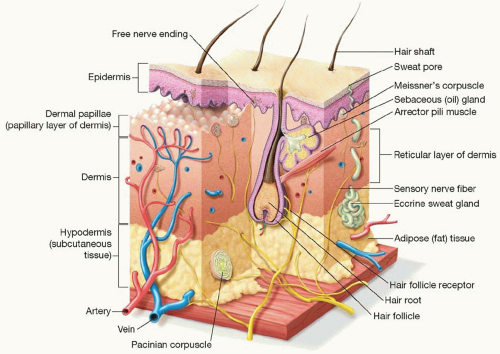
LAYERS OF THE SKIN
In basic terms, the skin is divided into two layers: the epidermis and the dermis (Figure 41.1). The epidermis provides a water exchange barrier (via its lipid intercellular mortar) and sun protection (via pigment). A vertical series of oxytalan elastic fibers attach the epidermis to the underlying dermis (Chapter 13).
The dermis is the structural layer of the skin. The more superficial papillary dermis provides flexibility and elastic recoil. The deeper reticular dermis provides a thick, sturdy foundation.
Natural aging is a process of atrophy of all skin elements—epidermis, dermis, and appendages. Actinic damage, to the contrary, is a process of thickening—particularly of the epidermis. The face, neck, chest, and hands are the most sun exposed and the most frequent sites of skin resurfacing.
THE MALADIES
Common benign maladies of the skin surface include dyschromias (solar lentigines), keratoses (actinic and seborrheic), and wrinkles.
With age, asynchrony of keratinocyte proliferation can produce seborrheic keratoses. These lesions are usually individually curetted, since they involve only the superficial epidermis. Actinic keratoses commonly occur with chronic sun exposure. If few, they may be individually treated with cryotherapy or trichloroacetic acid (TCA). If diffuse, overall skin resurfacing may be required.
Skin pigmentation occurs from melanocytes that are principally distributed along the basement membrane. Each melanocyte normally controls the production and distribution of melanin to approximately 15 to 18 keratinocytes.
With age and irradiation-induced DNA damage, asynchrony of melanin production and/or distribution occurs. Thus, collections of excess pigment (lentigines) occur. Solar lentigines are common on the face, chest, and dorsal hands. Histologically, both increased number of basal melanocytes and increased deposition of melanin in keratinocytes are present. Cryotherapy is a common treatment for isolated lesions, since melanocytes are particularly susceptible to cold injury.1,2 Broader fields of lentigines are more conveniently treated with TCA peels or intense pulsed light treatments.3,4 Eradication requires destruction to the basal layer of the epidermis.
On rare occasions, abnormal pigment may be distributed into the dermis—a condition known as melasma. Melasma occurs most commonly in young females and is felt to be hormonally induced. Treatment is unpredictable. Topical Retin A and hydroquinone 2% to 4% to block melanin production is useful and is critical for avoiding recurrence. Dermal chemical peels, intense pulse light, and non-ablative laser treatments may also be useful.
The exact cause of fine lines and wrinkles remains undetermined. Changes in the epidermis, loss of oxytalan fibers at the dermal-epidermal (DE) junction, and “elastotic” thickening in the superficial dermis all seem to play a role. What empirically seems clear, however, is that correction of skin wrinkles requires some type of ablative therapy through the DE junction into the papillary dermis at least.5,6,7
RESURFACING MECHANISMS
The concept of resurfacing is to destroy the layers of the skin down past the level of the abnormality, followed by healing of the skin to replace the removed layers with fresh, healthy tissue.
If the level of destruction is confined to the epidermis, the re-epithelialization occurs from the basal layer of the epidermis. If the level of destruction removes the epidermis, re-epithelialization occurs from lateral migration of adjacent keratinocytes and vertical migration of epithelial cells from the underlying dermal appendages (sweat glands and hair follicles). Destruction into the dermis stimulates a healing response characterized by new collagen production. The type of collagen response varies with the injury mechanism.
For practical purposes, there are three methods of resurfacing: mechanical sanding (dermabrasion), chemical burn (chemical peels), and photodynamic treatments (laser ablation or coagulation).
There are several side effects of skin resurfacing that influence the choice of method and application: rate of healing, loss of skin texture, depigmentation, and potential for visible scarring.
Any injury that removes all epithelium and enters the dermis can cause scarring. The exact limits of dermal depth and injury type which exceeds the normal healing capacity and produces visible scarring are not known. However, it is apparent that the deeper the dermal injury, the greater the likelihood of scarring. In addition, certain topographic areas are more prone to scar—such as the mandibular border and neck where the dermis is thinner and there are fewer underlying skin appendages for re-epithelialization.
The vast majority of melanocytes occur along the basal epithelial layer, although some also reside in the hair follicles. Complete removal of the basal melanocytes by destruction or selective melanocyte injury (such as heat from coagulative lasers or phenol peel) can result in unwanted hypopigmentation.
The opposite can also occur. Freshly re-populating melanocytes are particularly sensitive to sunlight stimulation and “post-inflammatory hyperpigmentation” can occur for the first several months of healing.
EPIDERMAL CORRECTIONS
Epidermal treatments usually focus on actinic keratoses, dyschromias, and dull skin from excess accumulation of old keratinocytes in the stratum corneum.
The skin abnormalities may be diffuse or patchy, but since the depth of treatment is superficial to the basement membrane,
repair is rapid from migration of surface epithelium. Therefore, a complete coverage treatment is safe and effective.
repair is rapid from migration of surface epithelium. Therefore, a complete coverage treatment is safe and effective.
The most common superficial treatments are chemical peels (Chapter 13).
α-Hydroxy acids are naturally occurring acids derived from fruits and milk products.8 They are shown in Table 41.1.
Glycolic acid has received the most wide use in topical products, primarily due to the fact that its smaller molecular size (two carbon chain) makes it penetrate the epidermis most readily. Both the concentration and the pH influence its penetration. As a topical peel, the FDA has suggested limits of 30% concentration and pH 3.0 or greater. It has been used “off label” in concentrations of 50% and lower pH’s. From a practical standpoint, patchy or uneven penetration is a problem that limits its use as an epidermal peeling agent. For this reason, glycolic acid peels are often administered in a gel base rather than in aqueous solution.
Lactic acid is a three carbon chain. As such, it penetrates more slowly and perhaps more evenly than glycolic acid. It can be applied in concentrations up to 70%.
The “frosting” end point of effect in α-hydroxy acid peels is often indistinct. As a result, they are usually applied on a time of application basis, followed by dilution with water rinsing.
β-Hydroxy acids are a chemical variant with two carbons between hydroxyl groups, versus one carbon separating hydroxyl groups in α-hydroxy acids. The most commonly used β-hydroxy acid is salicylic acid. Salicylic acid in concentrations up to 30% can be used for peeling. Salicylic acid produces a visible white frost (even more visible under fluorescent light), which makes the end point easier to assess. It is particularly effective in acne skin patients. Historically, salicylic acid lost favor because of the side effect of tinnitus with higher concentrations.
TABLE 41.1 α-HYDROXY ACID NATURALLY OCCURRING SOURCE | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
The most commonly used superficial peeling agent is Jessner’s solution (formerly Coombes formula).9 It is a combination of α- and β-hydroxy acids, providing benefits of both, but each in low enough concentration to limit side effects. The formula is usually mixed as follows:
Resorcinol | 14 g |
Salicylic acid | 14 g |
Lactic acid | 14 mL |
OS ethanol | 100 mL |
Premixed Jessner’s solution is commercially available. The mixture has several advantages. First, a light frost end point can be visualized. Second, it rapidly volatizes, so it does not need neutralization. Depth is controlled by the number of layers applied. Jessner’s peels are not only used alone as an epidermal peeling agent, but they are also commonly used for initial dekeratinization to facilitate the penetration of other chemical peels such as TCA.
TCA has been used as a variable depth skin peel since at least 1962.10 It is used in strengths of 15% to 20% for epidermal peels. Coagulation of keratinocyte protein produces a light white frost, which is easy to read as an end point. Epidermal TCA peels desquamate in approximately 5 days and are effective for correction of superficial actinic changes and dyschromias.
DERMAL CORRECTION
Wrinkles and fine lines involve at least the DE junction, if not the dermis itself. Correction requires a treatment that penetrates to the dermis and causes secondary fibroblastic production of
collagen. While elastin replacement has been theorized, there is yet no predictable way to stimulate normal elastin replacement.
collagen. While elastin replacement has been theorized, there is yet no predictable way to stimulate normal elastin replacement.
The more aggressive resurfacing methods—deeper peels, dermabrasion, and lasers—are most commonly employed for dermal problems. Scarring risk, however, increases significantly as the dermis is injured. The key to each of the dermal treatments is determining the depth of treatment—the clinical end point. Each technique has different visual signs and all the signs are relatively subtle. Experience is required to learn to accurately “read” those end points.
CHEMICAL PEELS
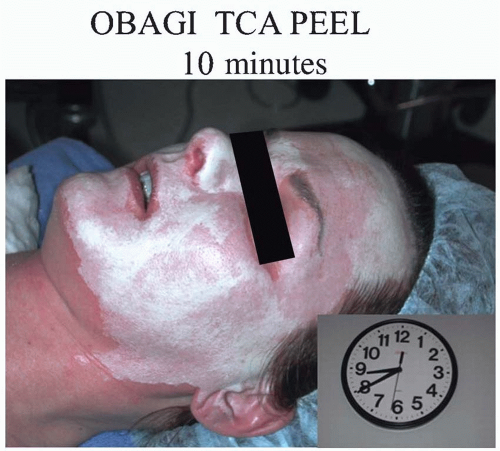
The two most common dermal depth peels are TCA and phenol/croton oil. Both create a definite white “frost” by coagulation of epidermal proteins (Figure 41.2).
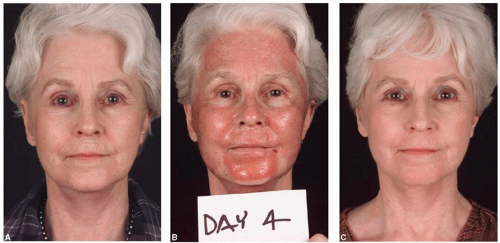 FIGURE 41.3. Patient with severe sun-damaged skin. A. Before treatment; B. Four days after 42.5% TCA to face and dermabrasion of upper lip; and C. 6 weeks post peel. |
TABLE 41.2 READING THE TRICHLOROACETIC ACID FROST | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
When used in a concentration of 35% to 42.5%,11 TCA is an excellent peeling agent for the face. One of the advantages of TCA is the ability to read the depth by clinical end points (Table 41.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree