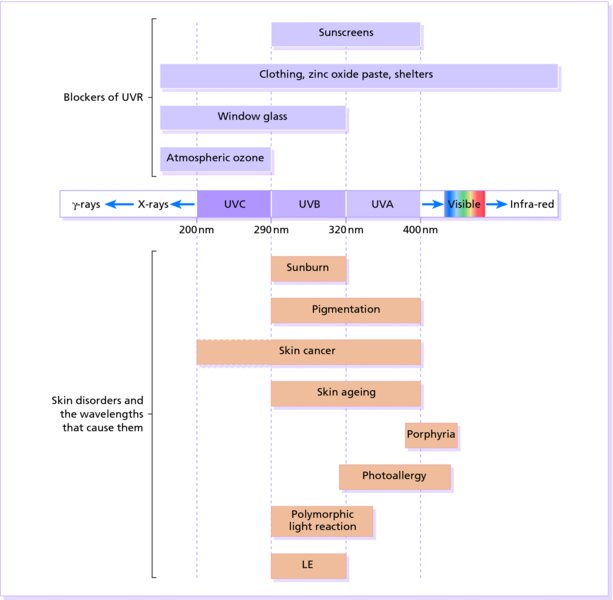
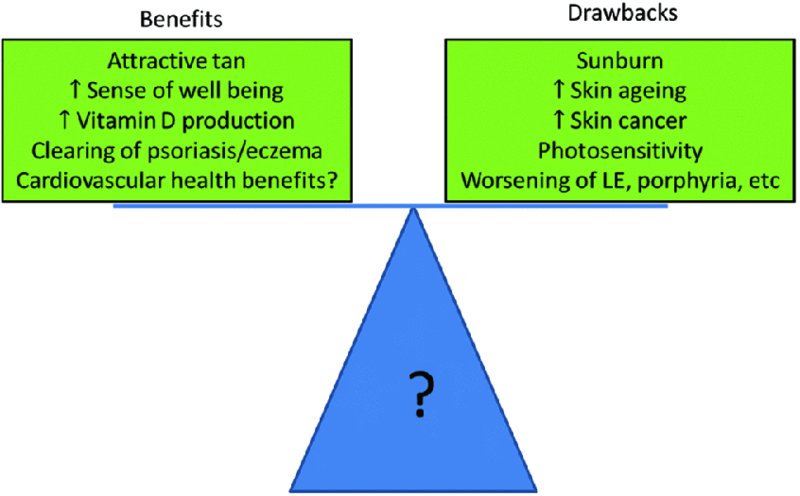
18 Ultraviolet radiation (UVR) has a mixture of beneficial and harmful effects. Our species, Homo sapiens, arose in Africa probably around 200 000 years ago. In contrast to our primate cousins, we have lost our covering of fur. In combination with the high volumes of sweat we can produce, this enables us to lose heat effectively, and originally we found our ecological niche as a long distance hunter, able to track our prey until heat and exhaustion fatally weakened it. With this loss of fur, however, has come the need to cope with the effects of the sun directly striking our epidermis. In the last 80 000 years we have scattered from our ancestral African homeland to populate the globe. The range of environments in which we have settled, from the tropics to the polar regions, and Himalayan heights to below sea level, has further altered our exposure to sunlight and imposed powerful evolutionary pressures on our skin. The most obvious effect of this has been in the range of pigmentation we show. This has been caused by two opposing evolutionary pressures. On the one hand we need pale enough skin to synthesise vitamin D, and, on the other, our skin needs enough eumelanin to protect from carcinogenesis and neural tube defect-inducing folate destruction. Recent large-scale population movements have led to high rates of skin cancer in white Australians, and high rates of rickets in immigrants from the Indian subcontinent to Scotland. The UVR spectrum is divided into three parts (Figure 18.1), each having different effects on the skin, although UVC does not penetrate the ozone layer of the atmosphere and is therefore currently irrelevant to skin disease. Virtually all of the UVB is absorbed in the epidermis, whereas some 30% of UVA reaches the dermis. The B wavelengths (UVB: 290–320 nm) cause sunburn and are effectively screened out by window glass. The A spectrum (UVA) is longwave ultraviolet light, from 320 nm to the most violet colour perceptible to the eye (about 400 nm). It ages and tans the skin. The differences between the wavelengths can be recorded conveniently in the form of action spectra, which show how effective each is at producing different biological effects, such as clearing psoriasis or causing erythema. UVR is non-ionizing, but changes the skin by reacting with endogenous light-absorbing chemicals (chromophores), which include DNA, RNA, urocanic acid and melanin. Figure 18.1 Skin disorders and the wavelengths that cause them. The variation in consitutive skin pigmentation and response to UVR is conventionally divided into six types (Table 18.1). These skin types require different degrees of protection against the sun. Table 18.1 Skin types classified by their reactions to ultraviolet radiation (UVR). A considerable body of epidemiological data suggest beneficial health effects of sunlight but the interpretation of these data can be contentious. Rickets is a disease of poor diet or inadequate sun exposure resulting in low vitamin D levels and correction of either of these factors is therapeutic. The case for the benefits of vitamin D in other conditions is less clear-cut. Observational studies show that subjects with high levels of circulating vitamin D are less likely to have cardiovascular disease, hypertension, type 2 diabetes or multiple sclerosis than those with low levels. Correlation should not be confused with causation, however, and the results of intervention studies in which vitamin D supplementation has been given have been disappointing. Ill health may lead to reduced sun exposure and thus low vitamin D levels (reverse causation), or vitamin D levels might be acting as a marker for sunlight exposure, which is beneficial via a different mechanism (confounding). A newly identified alternative mechanism is mediated by the vasodilator nitric oxide. The skin contains large stores of nitrate and nitrite, which are converted by sunlight to the nitric oxide from where it enters the circulation and lowers blood pressure. Other mechanisms may also exist. Clinically, UVR is helpful in the treatment of diseases such as psoriasis and eczema, but at the same time use of tanning lamps, particularly by young people, increases the risk of developing melanoma and non-melanoma skin cancers. Excess UV exposure also leads to photoageing, and may cause or worsen several skin disorders (Figure 18.2). Figure 18.2 The balance between the benefits and drawbacks of sun exposure. UVB penetrates the epidermis and superficial dermis, stimulating the production and release of prostaglandins, leukotrienes, histamine, interleukin 1 (IL-1) and tumour necrosis factor α (TNF-α). These cause pain and stimulate the production of the inducible nitric oxide synthase (iNOS) enzyme. This generates very high local concentrations of nitric oxide which causes the characteristic dermal vasodilatation and redness. Skin exposed to too much UVB smarts and becomes red several hours later. Severe sunburn is painful and may blister. The redness is maximal after 1 day, contemporaneously with peak levels of the iNOS enzyme, and then settles over the next 2–3 days, leaving sheet-like desquamation (Figure 18.3), diffuse pigmentation (a ‘tan’) and, sometimes, discrete lentigines. Figure 18.3 Peeling after acute sunburn. This doctor’s son should have known better. Phototoxic reactions caused by drugs are like an exaggerated sunburn. None are required. The treatment is symptomatic. Baths may be cooling and oily shake lotions (e.g. oily calamine lotion) or creams are comforting. Potent topical corticosteroids (Formulary 1, p. 401) help if used early and briefly. Oral aspirin (a prostaglandin synthesis inhibitor) relieves the pain. Basic photochemical laws require a drug to absorb UVR to cause such a reaction. Most drugs listed in Table 18.2 absorb UVA as well as UVB, and so window glass, protective against sunburn, does not protect against most phototoxic drug reactions. Table 18.2 Drugs commonly causing photosensitivity. Tenderness and redness occur only in areas exposed both to sufficient drug and to sufficient UVR (Figure 18.4). The signs and symptoms are those of sunburn. The skin may later develop a deep tan. Figure 18.4 Extreme photosensitivity of a patient taking griseofulvin. Note sparing of the area covered by the watch strap and ring. These reactions are not immunological. Everyone exposed to enough of the drug, and to enough UVR, will develop the reaction. Some drugs that can cause phototoxic reactions are listed in Table 18.2. In addition, contact with psoralens in plants (Figure 18.5) can cause a localized phototoxic dermatitis (phytophotodermatitis; Figure 18.6). These areas burn and may blister, leaving pigmentation in linear streaks and bizarre patterns. Figure 18.5 Cow parsley contains psoralens and is a common cause of photodermatitis.
Skin Reactions to Light
Type
Definition
Description
I
Always burns but never tans
Pale skin, red hair, freckles
II
Usually burns, sometimes tans
Fair skin
III
May burn, usually tans
Darker skin
IV
Rarely burns, always tans
Mediterranean
V
Moderate constitutional pigmentation
Latin American, Middle Eastern
VI
Marked constitutional pigmentation
Black
Beneficial effects of sunlight
Sunburn
Cause
Presentation and course

Differential diagnosis
Investigations
Treatment
Phototoxicity
Amiodarone
Chlorpromazine
Doxycycline
Nalidixic acid
Naproxen
Piroxicam
Phenothiazines
Psoralens
Sulfonamides
Tetracyclines
Thiazides
Topical NSAIDs
Etofenamate
Ketoprofen
Topical UV absorbers
Octocrylene
Benzophenone-3
Voriconazole
Presentation and course

Cause

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








