The legs are predisposed to dermatoses that are gravity dependent, including stasis dermatitis and vascular conditions such as leukocytoclastic vasculitis, the pigmented purpuric dermatoses, and livedo reticularis. Legs are also the site of frequent trauma and thus are susceptible to conditions that may be induced by trauma including superficial thrombophlebitis, pyoderma gangrenosum, necrobiosis lipoidica, chronic ulcers, and cellulitis. In patients with preexisting vascular conditions affecting the lower extremities, including diabetes mellitus, venous insufficiency, and peripheral vascular disease, traumatic wounds may take longer to heal and may have an increased risk of infection.
Skin diseases primarily involving the legs can be broadly categorized into inflammatory conditions, infectious diseases, superficial vascular disorders, neoplastic lesions, and underlying systemic diseases (see Table 35-1). Differentiating between these conditions can usually be done based on an appropriate history and physical examination. Occasionally, dermatitis on the lower extremities may be difficult to distinguish from a cellulitis. Cellulitis of the lower extremities tends be unilaterally, as compared to dermatitis, which usually is bilateral.
| Disease | Epidemiology | History | Physical Examination |
|---|---|---|---|
| Inflammatory | |||
| Asteatotic dermatitis | Common M > F Age: typically >60 years | Pruritus and dry skin Waxing and waning course Worse in winter | Dry, fissured, cracking, mildly scaly and inflamed plaques on bilateral anterior lower legs (Figure 8-3) |
| Stasis dermatitis | Common F > M Age: middle-aged and elderly adults | Asymptomatic or pruritic Associated with leg swelling | Erythematous, scaly plaques, may be hyperpigmented, lichenified, or sclerotic on bilateral anterior lower legs, especially medial ankles (Figure 29-1) |
| Nummular eczema | Common M > F Age: Adults | Pruritus Chronic, waxing, and waning course Worse in fall and winter | Round, light pink, scaly, thin, 1-3 cm plaques on legs (Figure 8-11) |
| Psoriasis vulgaris | Common M = F. Onset at any age but peaks in 20s and 50s | Asymptomatic to mildly pruritic. Chronic course. May be associated with arthritis Family history of psoriasis | Red papules and plaques with silvery, thick, adherent scale, commonly on knees (Figure 9-1) |
| Erythema nodosum | Uncommon F > M Age: 20-40 years | Tender lesions Variable course May be associated with fevers and arthralgias | Indurated, tender, red, deep, poorly defined nodules, usually on bilateral shins (Figure 24-14) |
| Pyoderma gangrenosum | Rare F ≥ M Age: all ages, but typically 30-40 years | Painful. May last months to years Spontaneous healing may occur | Initially, a hemorrhagic pustule with surrounding erythema. Later, ulceration with granulation tissue, eschar and purulent material at the base, and a dusky red/purple border (Figure 2-13) |
| Infectious | |||
| Cellulitis | Common M = F Age: more common in older adults | Pain, swelling, fever, chills, and malaise Increased risk in diabetics | Localized warm, red, tender plaque with ill-defined borders, usually on lower leg (Figure 12-3) |
| Tinea corporis | Common M > F Age: any age | Mild pruritus History of concomitant tinea pedis | Solitary or grouped, well-demarcated red annular plaques with a raised border and peripheral scale (Figure 10-4). Sometimes peripheral vesicles or pustules |
| Neoplastic | |||
| Stucco keratoses | Common M > F Age: older adults | Asymptomatic and usually unnoticed | Keratotic, stuck on appearing, whitish-grey papules bilaterally on extensor surface (Figure 16-3) |
| Systemic | |||
| Diabetic dermopathy | Uncommon M:F unknown Age: usually >50 years | Asymptomatic Appears in crops. Slowly resolves with scarring | Well-circumscribed, round, atrophic, and hyperpigmented plaques that heal with scarring on bilateral shins |
| Necrobiosis lipoidica | Uncommon F > M Age: young adults | Usually asymptomatic, but may ulcerate and become painful. Gradual onset, may last years. One-third have history of diabetes or minor trauma | Well-demarcated, shiny plaque with a mildly elevated erythematous border and an atrophic, yellowish, waxy center on bilateral shins (Figure 24-8) |
| Thrombocytopenic purpura (TTP) | Uncommon M = F Age: any age, depending on etiology | Asymptomatic Onset: hours Associated with low platelets due to HIV, TTP, ITP, DIC, drugs, infections, and bone marrow dyscrasias | Petechiae: pinpoint, nonblanching, nonpalpable red macules (Figure 25-1) Ecchymosis: larger red macules and black-and-blue patches |
| Vascular | |||
| Superficial thrombophlebitis | Uncommon M:F unknown Age: young to middle aged adults | Asymptomatic or tender Idiopathic or due to trauma, infection, IV extravasation, or migratory thrombophlebitis | Red and tender subcutaneous cord with swelling along the course of a vein Can occur on the trunk or extremities, but most commonly occurs on the legs |
| Leukocytoclastic vasculitis. | Uncommon M = F Age: all ages | Asymptomatic, pruritic, or tender. Duration: days to years depending on etiology. Idiopathic or due to drugs, underlying CVD, infections, or malignancy | Classic presentation is palpable purpura/petechiae with bright red well-defined macules and scattered red papules on lower legs and ankles (Figure 25-4) |
| Pigmented purpuric dermatosis (Schamberg’s disease) | Common M > F Age: typically 30-60 years | Asymptomatic or mildly pruritic. Slowly evolving over months. Chronic course, lasting years | Characteristic purpuric, speckled, “cayenne pepper-like” macules or less commonly annular plaques and lichenoid papules on lower legs |
| Physiologic livedo (cutis marmorata) | Common M:F unknown Age: more apparent in neonates, infants, and children | Asymptomatic A physiologic phenomenon that occurs in the cold | Purple discoloration of the skin in a netlike distribution on the lower extremities that resolves with warming |
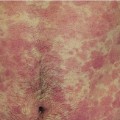
| Primary and secondary pathologic livedo reticularis (LR) | Uncommon M < F Age: 20-30 years of age | Asymptomatic. Secondary LR is associated with conditions that cause vasospasm, increased blood viscosity, vasculitis, or intravascular obstruction | Purple discoloration of the skin in a netlike distribution on the lower extremities that persists after rewarming (Figure 2-28) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree