Hands have structures with many unique structural and functional features. As such, they are prone to developing specific dermatologic diseases. Structurally, the palms have a thick keratin layer, a high concentration of sweat glands, Meissner’s corpuscles, and other mechanoreceptors. Functionally, we use our hand to interact with the world. Therefore, hands are subject to physical injury. Hands are often the first body part to come into contact with objects and substances in our environment. As a result, they are frequently the site of exposure to allergens, irritants, and infectious agents. This concept is central to the transmission of pathogens and development of certain dermatologic conditions such as contact dermatitis. Given their distal location, the neurovascular supply of hands (particularly the digits) can also predispose the hands to neuropathies, ischemic insults, and vasculitides. Hands tend to get more sun exposure than centrally located anatomical structures thereby subjecting them to photodermatoses and actinic damage. Hands may also manifest cutaneous signs of internal disease.
Skin diseases primarily involving the hands can be broadly categorized into inflammatory dermatoses, infections, connective tissue disorders, and photodermatoses (see Table 33-1). Widespread actinic keratoses on the hands are also included in this chapter because they are sometimes misdiagnosed as a “rash.” The inflammatory dermatoses are most common and typically present with pruritic papules or plaques. The morphology of tinea manuum depends on its distribution, with annular plaques being more common on the dorsal hand and diffuse fine scale on the palm. Sunlight-induced dermatoses and connective tissue disorders present on the dorsal hands with pink papules and plaques.
| Disease | Epidemiology | History | Physical Examination |
|---|---|---|---|
| Inflammatory | |||
| Irritant contact dermatitis | Common F > M Any age Atopics are at increased risk | Pruritic, burning, or painful Variable onset depends on frequency of exposure and strength of irritant | Well-demarcated with a “glazed” appearance Erythema, fissures, blistering, and scaling usually in finger web spaces or dorsum of hands (Figures 8-1, 8-2, 8-3) |
| Allergic contact dermatitis | Common F > M Any age | Pruritic with onset hours to days after contact with allergen | Acute: papules and vesicles on an erythematous base (Figures 8-4 and 8-5) Chronic: xerosis, fissuring, hyperpigmentation, and lichenification usually on the dorsum of hand and distal fingers (Figures 8-1, 8-2, 8-3) |
| Atopic dermatitis | Common F > M Age: any May be only manifestation of disease in adults | Pruritic and sometimes painful Chronic course with exacerbations Triggers: frequent hand washing or wet work Usually worse in winter Family history of atopy | Presents with swelling, xerosis, fissuring, erythema, and lichenification on dorsum and palms (Figure 2-10) |
| Dyshidrotic dermatitis | Common F ≥ M Age: young adults and atopics overrepresented | Very pruritic Chronic and recurrent, episodes last 2-3 weeks. Exacerbated by sweat and stress | Multiple grouped vesicles and erosions on noninflammatory base on lateral surface and palms (Figure 8-12) |
| Psoriasis vulgaris | Common M = F Age of onset: peaks in 20s and 50s. May be only manifestation of disease | Painful fissures or pruritic Chronic indolent course May have arthritis and family history of psoriasis | Presents with well-demarcated erythematous plaques with loosely adherent, silvery scale (Figure 9-1), or less commonly with pustules on central palms (Figure 9-6) |
| Palmoplantar pustulosis | Uncommon F > M Onset: 50-60 years of age | Pruritus, burning, pain Lasts years Waxing and waning course | Scattered creamy yellow pustules and dusky red macules on palms |
| Lichen planus | Uncommon F > M Age: 30-60 years | Asymptomatic or pruritic Lasts months to years May be drug-induced or associated with hepatitis C infection | Classically, flat-topped, well-defined, polygonal, violaceous, shiny papules on volar wrist and dorsum (Figure 9-10) |
| Infectious | |||
| Warts | Common M > F More common in children and young adults | Asymptomatic or painful. May persist for years | Discrete or confluent hyperkeratotic papules or plaques. May have black or brown dots within the lesions created by thrombosed capillaries (Figure 11-6) |
| Tinea manuum | Uncommon M > F | Asymptomatic or pruritic. Last months to years Contact with infected person or animal or autoinoculation (eg, from foot or groin) Usually associated with tinea pedis | On palms presents with diffuse fine scaling (Figure 10-6). Unilateral in 50%. On dorsum presents with annular red patch/plaque with peripheral scale at leading edge. Nails may be affected |
| Herpetic whitlow | Uncommon At risk: Healthcare workers, or contact with HSV | Painful | Grouped and confluent vesicles on red edematous base on a distal digit |
| Neoplastic | |||
| Actinic keratoses | Common M > F Age: >40 years | Asymptomatic or tender Duration: months to years Risk factors: advancing age, cumulative sun exposure, outdoor occupation, and fair skin type | Skin-colored, yellow-brown, pink ill-defined gritty papules with adherent hyperkeratotic scale (Figure 17-1) |
| Systemic disease | |||
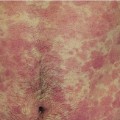
| Acute cutaneous lupus erythematosus (generalized) | Uncommon F > M Age: any age, but most commonly 30-40 years of age High morbidity | Pruritus or burning Duration: weeks to months Maybe related to sun exposure. Associated with fevers, fatigue, oral ulcers, and other systemic findings consistent with SLE | Red clustered papules, urticarial plaques, and patchy erythema with variable scale on dorsal hands, classically sparing the skin overlying the joints |
| Dermatomyositis | Uncommon F > M Age: bimodal; peaks at ages 5 to 10 and 50 years | Asymptomatic or mildly pruritic. Chronic course Associated with photosensitivity, scalp pruritus/burning, and symmetric proximal muscle weakness | Flat-topped violaceous papules overlying knuckles and interphalangeal joints (Gottron’s papules) Periungual erythema (Figure 24-6) |
| Porphyria cutanea tarda | Uncommon M = F Age: adults 30-50. Hereditary or acquired (eg, medications) | Pain from erosions Gradual onset easily traumatized fragile skin Implicated drugs: ethanol, estrogen, iron, among others Other predisposing factors: diabetes mellitus and hepatitis C virus | Tense vesicles/bullae and erosions with normal appearing surrounding skin Atrophic white-pink scars and milia on dorsal hands (Figure 24-13) |
| Photodermatoses: see Chapter 31 (Skin Diseases of the Face) | |||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree