The plantar surface of the foot has the thickest keratin layer, a high concentration of eccrine sweat glands, as well as sensory nerves, including Pacinian corpuscles, and other mechanoreceptors. The combination of abundant keratin and sweat creates an ideal environment for fungal infections. Friction and contact with footwear also make the feet susceptible to contact dermatitis. In addition, the feet are disproportionally affected by vascular disorders, due to their gravity-dependent anatomical location, and by peripheral small fiber sensory neuropathies. Since the feet are a site of frequent injury, vascular disorders and sensory neuropathies predispose this area to recurrent and difficult-to-manage wounds.
The most common causes of skin diseases on the feet are dermatophyte infections and inflammatory dermatoses (see Table 36-1). Clinically these two categories of disease are often indistinguishable from one another. The presence of fissures and/or scale in the toe web space and nail dystrophy is more suggestive of a dermatophyte infection, but nail dystrophy can also occur in psoriasis.
| Disease | Epidemiology | History | Physical Examination |
|---|---|---|---|
| Inflammatory | |||
| Allergic contact dermatitis | Common F > M Age: any age | Pruritus and painful fissures Onset: hours to days after contact with allergen | Acute: Papules and vesicles on an erythematous base (Figures 8-4 and 8-5) Chronic: xerosis, fissuring, hyperpigmentation, and lichenification (Figures 8-1, 8-2, 8-3) |
| Atopic dermatitis | Common M ≥ F Age: usually begins in childhood but may persist | Pruritic and painful Chronic waxing and waning course Family history of atopy | Presents with swelling, xerosis, fissuring, erythema, and lichenification on the dorsal feet and soles (Figure 2-10) |
| Dyshidrotic dermatitis | Common F ≥ M Age: usually young adults | Severely pruritic or painful. Chronic and recurrent with episodes lasting 2-3 weeks | Multiple grouped vesicles and erosions on a noninflammatory base located on the soles (Figure 8-12) |
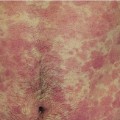
| Psoriasis vulgaris | Common M = F Age of onset: any age, but peaks in 20s and 50s | Pruritic and painful Chronic, indolent course. Associated with arthritis and nail pitting/dystrophy Family history of psoriasis | Well-demarcated plaques with adherent, thick scale on an erythematous base. Less commonly present with pustules over pressure-bearing regions of the soles (Figure 9-1) |
| Palmoplantar pustulosis | Uncommon F > M Age: 50-60 years of age | Pruritus, burning or pain Chronic waxing and waning course | Scattered creamy-yellow pustules and dusky-red macules on soles, with a tendency to affect the heel and instep of the foot; may be bilateral or unilateral |
| Infectious | |||
| Tinea pedis | Common M > F Age: post-puberty | Asymptomatic or pruritic Lasts months to years Associated with onychomycosis | Interdigital type: dry scaling and/or maceration, peeling, and fissuring in toe webs (Figure 10-9) Moccasin type: well-demarcated erythematous patch with fine, white uniform scale on soles and sides of feet (Figure 10-10) Inflammatory/bullous type: vesicles or bullae containing clear fluid, erosions on the soles (Figure 10-11) |
| Cellulitis | Common M = F Age: any age, but occurs more commonly on the feet in adults | Pain swelling, fever, malaise, and chills Increased risk in diabetic patients and patients with fissures on their feet | Localized erythema, warmth, swelling, and tenderness with ill-defined borders (Figure 12-3) |
| Warts | Common M > F Age: more common in children and young adults | Asymptomatic or painful. May persist for years | Discrete or confluent hyperkeratotic papules or plaques on soles. May have black or brown dots within the lesions created by thrombosed capillaries (Figure 11-7) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree