Skin and Soft Tissue
L. Scott Levin
Martin I. Boyer
David J. Bozentka
Stephan G. Pill
Kodi K. Azari
Nelson Castillo
Amit Gupta
I. Nail
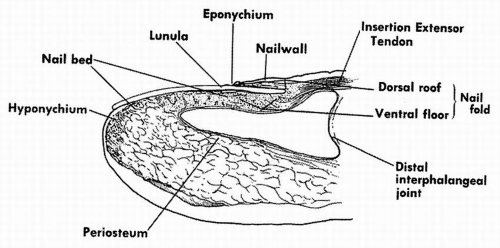
Anatomy (Fig. 20.1)
The perionychium consists of the nail bed, nail fold, eponychium, paronychium, and hyponychium.
The nail bed is the soft tissue beneath the nail and consists of the germinal matrix proximally and the sterile matrix distally. The nail bed is supplied by two terminal branches of the volar digital artery and innervated by the dorsal branch of the digital nerve.
The germinal matrix extends from the nail fold to the lunula, which is a white arc distal to the eponychium. The germinal matrix is responsible for generating 90% of the nail plate.
The sterile matrix extends from the lunula to the hyponychium. It provides adherence and adds a squamous epithelial layer to the nail plate.
The proximal nail fold is the most proximal extent of the perionychium and consists of a dorsal roof and a ventral floor.
The eponychium is the skin covering the nail fold. It extends from the skin on the dorsum of the nail, which is termed the nail wall, to the dorsal aspect of the nail plate.
The cuticle, the nail vest, is the thin membrane that extends from the eponychium to the nail plate.
The paronychium is the skin on each side of the nail.
The hyponychium is the junction of the nail bed and the skin at the most distal aspect of the finger. It is a barrier to infection and has the greatest density of lymphatics of any dermal area in the body.
Nail injuries
Many nail bed injuries are simple lacerations, although stellate lacerations, crush, and avulsion injuries are also possible.
Injury to the sterile matrix causes nail deformity, and injury to the germinal matrix can cause nail absence.
Nail bed exploration may necessitate nail plate removal, and lacerations can be repaired with fine absorbable suture, such as 7-0 Chromic. If the laceration involves the nail fold, roof/floor, the nail plate should be cleansed and replaced. Alternatively, foil or gauze can be introduced into the nail fold. An x-ray should be obtained to rule out an underlying fracture.
A subungual hematoma can occur if there is disruption of the nail bed within an intact nail plate. Bleeding into this poorly compliant space can cause severe pain, and evacuation via nail trephination or removal may be needed
to relieve symptoms. In general, drainage alone is sufficient for smaller hematomas whereas areas greater than 50% of the nail bed are often best treated with removal of the nail plate and repair of the underlying nail bed injury. The removed nail should be cleansed and replaced in the nail fold.
Nail deformity
Nonadherence is the most common posttraumatic deformity. Since the sterile matrix produces nail cells that adhere to the undersurface of the nail, transverse or diagonal scars of the sterile matrix can cause the nail to loosen distal to the scar. Proximal nonadherence often results in an unstable, painful nail. Distal nonadherence is not a problem unless dirt buildup underneath the nail causes an infection. The scar must be resected for correction of the deformity. The defect can either be closed primarily or a sterile matrix graft can be applied from an adjacent area of the nail bed or toenail bed.
Ridges can be caused by scar tissue under the nail bed or from an uneven dorsal cortex. Ridging can cause distal nonadherence. Scar excision and smoothing of the irregularity to create a flat nail bed are required to correct the deformity.
A split nail can result from a ridge or longitudinal scar in the germinal or sterile matrix. The scar is usually too wide for excision and primary repair of the defect. Sterile matrix scars should be removed and covered with a split-thickness nail bed graft. Germinal matrix scars require full-thickness grafts for nail production.
Cornified nail bed deformities occur when the germinal matrix is removed but the sterile matrix continues to produce keratinized material. Treatment consists of sterile matrix excision and covering the defect with a split-thickness skin graft (STSG).
Nail cysts and spikes can follow incomplete removal of the germinal matrix after amputation of a fingertip. Cysts are formed when the germinal matrix continues to produce nail under a closed defect. Patients present with a painful, enlarging mass. (Spikes result when the germinal matrix remains, leading to distal nail production.) These are commonly seen after resection
of an ingrown toenail. Treatment consists of removal of the cyst or spike and complete excision of the germinal matrix.
Hook nail deformity is a nail with a pronounced volar curvature and occurs when there is a loss of bony support under the nail. It is most commonly seen after primary closure of fingertip amputation, when the nail bed is pulled down over the distal phalanx. Acute treatment involves trimming the nail bed back to the distal extent of the distal phalanx. Although providing sufficient initial supports, bone grafts tend to resorb. Once a hook nail is present, the soft tissue of the fingertip must be restored and the nail bed transferred back to the level of the bone. This may be accomplished by a V-Y advancement flap, cross-finger flap, or full-thickness skin graft (FTSG). Free vascularized toe transfers have been described to preserve nail length, although they are associated with significant donor site morbidity.
Pincer nail deformity is an abnormal curvature of the nail in a radioulnar direction. It often gives semicircular appearance to the nail when viewed from the distal aspect. On occasion, it will be painful along the radial or ulnar aspects and have the appearance of an ingrown nail. Treatment can be unpredictable, but when attempted, involves elevation of the nail matrix off the bone and placement of a dermal graft. When successful, this will restore the normal contour to the nail.
Pterygium refers to scarring of the nail fold and eponychium to the nail bed. The nail is unable to grow at the site of scarring leading either to nail absence or splitting. Treatment consists of freeing the dorsal roof of the nail fold from the nail bed and either inserting a silicone sheet in this space or placing a split thickness sterile matrix graft on the undersurface of the eponychium to prevent rescarring. Alternatively, the eponychium can be reconstructed with a composite graft. Pterygia can also occur within the hyponychium leading to a painful fingertip. Treatment consists of removing the distal nail and hyponychium and placing a STSG in its place to cause an iatrogenic nonadherence.
II. Introduction to Soft Tissue Coverage
Partial-thickness wounds can heal by re-epithelialization, since the basement membrane remains intact and is capable of regenerating more superficial skin layers.
Fibroblasts at the margins of full-thickness wounds differentiate into myofibroblasts, which contract to pull the skin edges together and reduce the area for wound healing.
Healing of full-thickness wounds can be facilitated by reconstructive options, including primary closure, secondary intention, skin grafting, and flap coverage. The most appropriate option depends on both wound and patient characteristics.
The reconstructive ladder is a method to approach wound reconstruction, which proceeds from simple to complex (bottom of the ladder to the top):
Free tissue transfer
Distant axial pattern flaps
Distant Random pattern flaps
Local Island pattern flaps
Local axial pattern flaps
Local random flaps
FTSGs
STSGs
Secondary intention
Primary closure
The goals of soft tissue coverage are to provide an adequate barrier to contamination, to restore sensibility, and to improve appearance.
Secondary intention
1. Allowing a wound to heal by secondary intention allows contraction and gradual re-epithelialization to provide healing when primary closure is not possible.
2. It can be used for small clean defects without exposed bone or substantial deep tissue loss.
3. The classic description is for a defect less than 1 cm in diameter, but this can be used for larger areas without exposed bone, tendon, or nerve.
3. It allows early joint mobilization, which can prevent contracture.
4. Since the defect heals by scar, adequate padding may not be restored and tenderness, cold intolerance, and poor cosmesis may result.
Skin grafts
Skin grafting: The use of skin grafts includes use of split-thickness or full-thickness grafts. Split grafts may be either meshed or unmeshed, and will successfully cover many wounds in the extremities. Indications are for wounds that cannot or should not be treated by primary or delayed primary closure. The wound bed must have good vascularity. Skin grafts will adhere to muscle, paratenon, and intact periosteum. Fat can be used as a bed, but is less predictable than the previously mentioned structures. The wound beds must be freshened prior to grafting, which includes the removal of collinized granulation tissue, to avoid infection and subsequent loss of the graft. Immobilization is critical for successful graft healing.
STSG
The epidermis and a variable amount of dermis are harvested by an adjustable dermatome.
Graft thickness can be thin (0.005 to 0.012 in), intermediate (0.012 to 0.018 in), or thick (0.018 to 0.030 in), although the most common graft thickness is 0.012 to 0.015 in.
The ideal recipient site is located where wound contraction will not lead to decreased joint mobility.
STSGs are particularly useful for defects on the dorsum of the hand and fingers.
Although any part of the body can be used for skinn graft harvesting, the anterolateral thigh is most commonly used donor site. The posterolateral trunk and thigh can be used for thicker grafts.
Meshing the graft allows expansion for coverage of a large area and allows drainage of postoperative hematoma, which enhances graft viability.
STSGs have a better take than full-thickness grafts.
Disadvantages include an inability to restore sensibility, and the greater tendency to contract, leading to a less attractive appearance.
FTSGs
FTSGs consist of the epidermis and the entire layer of dermis.
The subcutaneous fat is manually removed from the graft prior to placing it in the defect.
The recipient site must be a clean vascularized bed.
They are particularly useful for defects on the palmar side of the hand and fingers.
Common donor sites include the groin and lower abdomen for large defects and the ipsilateral extremity for small defects (i.e. hypothenor skin).
The donor site should be larger than the defect to allow for primary contracture following harvest of the graft.
The donor site is typically closed primarily, thus, limiting FTSG to smaller defects, but the donor site can be covered with a STSG.
Advantages include improved wound bed protection, better reinnervation potential, less wound contracture, and faster maturation.
Disadvantages include a higher infection rate and an overall lower survival, in comparison to STSG.
Local or distant flaps
More complex wounds with exposed neurovascular or tendinous structures, bone devoid of periosteum, insufficient vascularity or poor soft tissue beds require the transfer of well-vascularized tissue to achieve wound closure. Rotation flaps, as isolated tissue or combination of muscle, fascia, or cutaneous tissue, can provide vascularized tissue for an obliteration of dead space and wound closure without tension. However, these options may be limited because of the wound location or regional donor site deficiencies. These include random-pattern, axial-pattern, or island flaps.
III. Flaps
A flap is a tissue transferred from a donor site to a recipient site while maintaining its own blood supply and is used when a defect cannot be closed primarily, should not be allowed to heal secondarily, and cannot support a skin graft. Their donor site can be closed primarily or covered with a STSG.
Skin flaps can be described by their vascular supply as random pattern or axial pattern.
Random-pattern flaps receive their blood supply by small, unnamed vessels from the subcutaneous or subdermal plexus. The flap is created by raising three sides and using the forth side as a pedicle. The flap length: width ratio should not exceed 2:1 to avoid vascular compromise. The flaps may be described by their geometric shape such as mitten (bilobed) flap, Limberg (rhomboid) flap, semicircular rotation, bipeninsular, or simple unipeninsular advancement.
In contrast, axial-pattern flaps are supplied by a single, constant vessel, which must be preserved as a vascular pedicle along the long axis of the flap. The area of skin supplied by the axial pedicle is called the vascular
territory. In general, axial-pattern flaps have a more substantial blood supply than random-pattern flaps, making them more resistent to infection. In addition, the better blood supply enables the length: width ratio to be greater than 2:1. Since the vascular pedicle must be carefully preserved, care must be taken when thinning the flap. The flaps may be described according to their contents, such as fasciocutaneous, muscle, musculocutaneous, osseous, osteocutaneous, or a composite (combination of tissue types) flap.
Skin flaps can also be described by location as local, regional, or distant. (Table 20.1)
Local flaps are taken from tissue adjacent to the defect. As such, they have similar characteristics to the lost skin. Local flaps can be advancement flaps, rotational flaps, transposition flaps, or island flaps. Ischemia at the tip of the flap is a concern with local flaps.
Advancement flaps have a pedicle on the side opposite to the primary defect.
Rotational flaps are random-pattern flaps that are moved laterally and stretched to cover both the donor and recipient sites. Therefore, by definition, rotational flaps are always bigger than the defect.
Transposition flaps are also moved laterally, but the donor site is closed primarily or with another graft.
Island flap implies an area of skin that is detached from all of its host attachments except for its vascular pedicle.
Regional flaps are taken from the ipsilateral limb when local tissue is of insufficient amount or quality.
TABLE 20-1 Regional flap options for upper extremity defects
Local Flaps
Regional Flaps
Distant Flaps
Z-plasty
Cross-finger flap
Groin flap
Axial flag flap
Reversed cross-finger flap
Latissimus dorsi flap
Dorsal metacarpal artery flap
Innervated cross-finger flap
Digital artery island flap
Cross-thumb flap
V-Y advancement flap
Thenar flap
Lateral V-Y advancement flap
Neurovascular island flap
Moberg flap
Radial artery forearm flap Ulnar artery forearm flap Reversed posterior interosseous artery flap
Fillet flap Scapular flap Lateral arm flap
Distant flaps are taken from a site outside the ipsilateral limb. They are either harvested as a free flap or divided at a second operative procedure.
Local flaps
Z-plasty
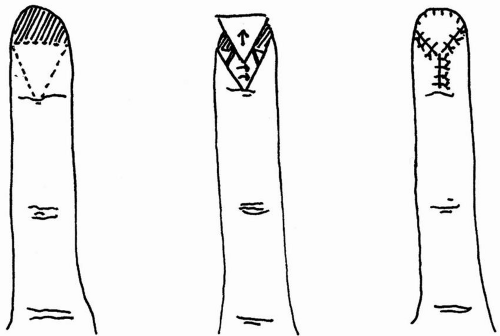
Z-plasty is a random, transpositional flap used to lengthen contractions or scars (Fig. 20.2).
All limbs must be of equal length.
It can increase scar length by 25% with 30-degree angles, 50% with 45-degree angles, and 75% with 60-degree angles.
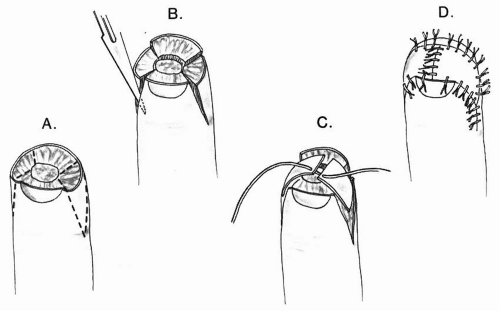
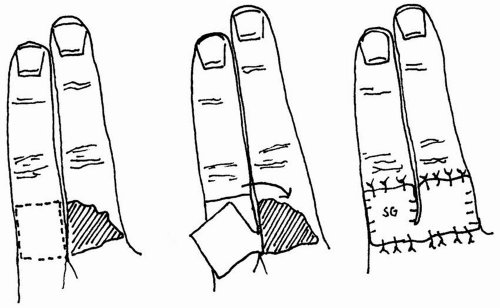
Atasoy volar V-Y advancement
This flap is often used for transverse fingertip amputations or amputations with more dorsal tissue loss (Fig. 20.3).
The skin is cut leaving the subcutaneous tissue intact for vascular supply. The V-cut points toward the distal interphalangeal joint (DIP) flexion crease and the distal flat edge is mobilized and pulled up over the top.
The proximal V-segment of skin is closed primarily.
It is useful when sensation is vital, such as in musicians (Table 20.2).
A different flap is typically needed when the predominant tissue loss is palmar.
Kutler paired lateral V-Y advancement flap
Similar to the Atasoy although the V-Y advancement is performed on both sides of the digit, and the flat distal portions are sutured together in the midline of the fingertip (Fig. 20.4).
Cleland ligaments must be freed dorsally, and the anterior neurovascular supply must be protected.
This flap is best for transverse fingertip amputations.
The scar at the tip of the finger can be problematic.
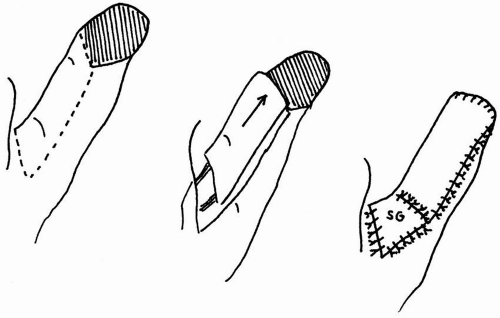
Moberg volar advancement flap
This volar rectangular skin flap is based on the neurovascular bundles and typically used for thumb pulp defects.
The flap is best for thumb defects, since the dorsal arterial supply is independent of the volar supply in the thumb, making dorsal skin necrosis less likely. Also, flexion of the interphalangeal (IP) joint is often needed for sufficient flap advancement, and IP contracture is better tolerated in the thumb.
Two midlateral incisions are made dorsal to the neurovascular bundles, and the flap is dissected off the flexor tendon sheath and can be advanced approximately 2.0 cm (Fig. 20.5).
The secondary site is closed primarily or covered with a skin graft.
The flap includes all the volar skin, subcutaneous tissue, and both neurovascular bundles from the tip injury to the metacarpophalangeal joint.
If the flap remains under tension, a proximal V-Y advancement or transverse incision can be used to slightly increase advancement. This area can be allowed to heal secondarily or covered with a FTSG on the secondary defect.
The IP joint is immobilized for 10 days post-op.
The disadvantages of this flap are limited advancement, flexion contracture, and possible injury to the dorsal vascular branches.
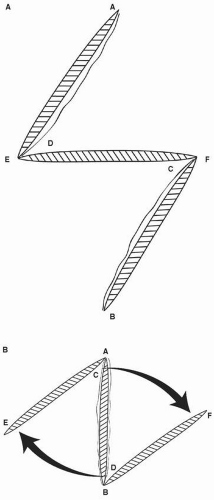
Figure 20.2 Z-plasty. Note that all sides must be equal in length. A. Flap design and B. Orientation after rotation of flap
Dorsal metacarpal artery island flap
The neurovascular island flap is raised from the dorsum of the index proximal phalanx and is most useful for defects on the thumb, first web space, and proximal long and ring fingers.
The pedicle contains the first or second metacarpal artery, veins, and branches of the radial nerve, which are dissected distal to proximal.
The interosseous fascia is included in the flap, since the vessel runs deep to this plane.
Doppler ultrasound can be used to identify the vessel course.
The flap can be raised with a proximal antegrade or reverse-flow pedicle, based on a perforator from the common digital vessels.
TABLE 20-2 Examples of local finger flaps, non-innervated and innervated
Non-innervated Flaps
Innervated Flaps
Thenar flap
V-Y advancement
Cross-finger flap
Moberg volar advancement Neurovascular island Innervated cross-finger Axial flag
The reversed-flow flap can extend as far ulnar as the fifth metacarpal head and is used for digital defects proximal to the PIP joints.
Axial flag flap
This flap is based on the dorsal digital artery or the proper digital artery at the web space of the donor finger (Fig. 20.6).
The flap is raised over the dorsum of the proximal phalanx, near the interdigital crease.
The index and long fingers are the most common donor fingers.
The flap is very mobile and can cover palmar defects in the proximal aspect of an adjacent digit.
The flap is particularly useful for coverage of defects with exposed tendon.
Regional flaps
Posterior interosseous artery flap
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree