■ This serves as a rough guide to when different lymphatic basins should be addressed; ultimately, the clinician should dissect all lymphatic basins that could potentially be harboring clinical disease based on an understanding of lymphatic drainage patterns.
■ The removal of the superficial lobe of the parotid gland is performed for any primary cutaneous tumor anterior to the external auditory canal and above the angle of the mandible.
■ Levels 1 to 4 are dissected with any lesion involving the scalp anterior to the plane of the external auditory canal, facial skin, or anterior neck skin.
■ Levels 2 to 5 are dissected with any lesion involving the scalp posterior to the plane of the external auditory canal or posterior neck skin.
■ If the primary lesion is in the scalp and located very close to the plane of the external auditory canal, dissection should include levels 1 to 5.
Positioning
■ Patients are placed supine with the top of the head at the edge of the surgical bed.
■ A bump is placed underneath the shoulder blades to allow for extension of the neck, being careful to maintain support of the head on the operating room (OR) table.
TECHNIQUES
SELECTIVE NECK DISSECTION LEVELS 1 TO 4
■ A curvilinear incision is made midway between the angle of the mandible and the clavicle; the incision travels within a neck crease, extending a few centimeters from the mastoid tip toward the approximate midpoint of the thyroid cartilage (FIG 2).

■ Skin is incised down through the subcutaneous tissue and platysma.
■ Subplatysmal skin flaps are elevated to expose the deeper contents overlying levels 1 to 4 of the neck; this will extend to the mentum, along the strap musculature in the midline, to the posterior border of the sternocleidomastoid muscle (SCM), and down to the level of the clavicle (FIG 3).

■ The marginal mandibular nerve is identified in the superficial layer of the cervical fascia near the angle of the mandible and is identified using nerve stimulation. The nerve is dissected free and elevated over the plane of the mandible (FIG 4).
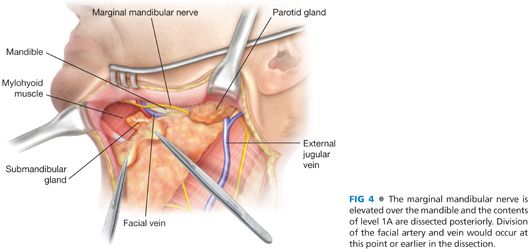
■ The facial artery and vein are identified and ligated as they cross over the plane of the mandible.
■ The tissue over the mandible is then incised from the mentum to the angle of the mandible, taking care not to injure the previously dissected marginal mandibular nerve. This tissue is pulled inferiorly, taking care to remove the perifacial lymph nodes located near the facial vessels. During this dissection, the retromandibular vein may be identified and ligated as it travels through the tail of the parotid gland.
■ Incise soft tissue over contralateral anterior belly of the digastric muscle from mentum down to hyoid bone.
■ Begin elevating contents of level 1A by pulling tissue laterally off the mylohyoid muscle toward the ipsilateral anterior belly of the digastric muscle; this will require division of tissue along the hyoid bone inferiorly.
■ Bring packet of tissue over ipsilateral digastric and back onto mylohyoid until the edge of the mylohyoid is reached see FIG 4.
■ Retract the mylohyoid muscle medially to allow for exposure of the contents deep to the submandibular gland. This may require some blunt dissection in this area. Identify the hypoglossal nerve, lingual nerve, and submandibular duct (FIG 5).
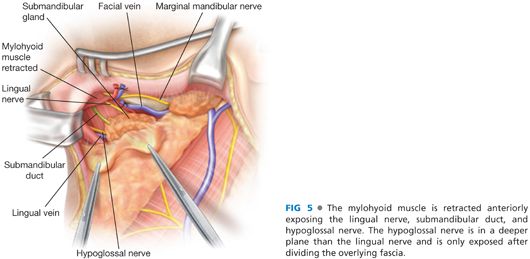
■ Divide the submandibular duct, taking care not to cause excessive bleeding from the nearby veins (FIG 6).

■ Divide the submandibular ganglion and allow the lingual nerve to retract superiorly.
■ Pull the submandibular gland and packet of tissue laterally, carefully dividing the tissue over the posterior belly of the digastric (FIG 7).
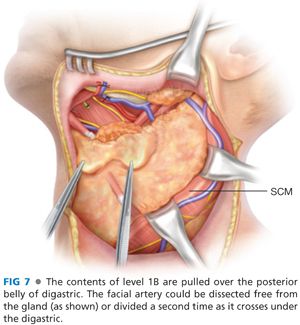
■ Approximately halfway up the posterior belly, the facial artery is again seen travelling under the digastric and into the submandibular gland; divide the artery a second time.
■ Trace the posterior belly superiorly, dividing the overlying tissue until the SCM is reached. If it has not already been divided, the retromandibular vein is usually encountered as it exits the parotid gland near the angle of the mandible—carefully divide the vein.
■ The SCM is then “unwrapped.” At the posterior edge of the SCM, incise the fascia over the muscle. This will require division of the cutaneous nerves that course over the muscle; the great auricular branch to the ear as well as the external jugular can sometimes be traced out and saved.
■ Pull the fascia medially to unwrap the SCM; be careful to take all tissue over the muscle because lymph nodes associated with the external jugular vein must be removed.
■ After the anterior surface of the SCM is wrapped, carefully roll the muscle outward to start unwrapping the deep surface; at the junction of the upper one-third and lower two-thirds, the cranial nerve (CN) XI (the spinal accessory nerve) will be encountered as it enters the muscle.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








