CHAPTER 39 Secondary rhinoplasty
Patient evaluation
• Determine the patient’s top three concerns (airway and aesthetic).
• Obtain thorough, but targeted history.
• External exam: Assess skin envelope, asymmetries, support of all three vaults and shape of the radix, dorsum, sidewalls, tip, base and alar regions.
• Internal exam: Assess septum, internal valve, bone spurs and turbinates.
• Septal support: Use a Q-tip to push on septum; apply Afrin spray to rule out perforations and synechiae.
• Include an ear, scalp and chest wall exam for potential graft material.
Anatomy
The tip
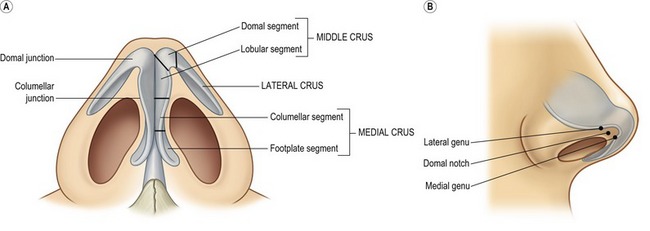
The usual concerns in the tip are volume, definition, width, rotation and projection. In secondary cases, distortion, deformity and deficiency must also be considered. The tip is composed of the paired lower lateral (alar) cartilages, each of which is composed of three crura; medial, middle and lateral (Fig. 39.1). The medial crus is comprised of the lower footplate segment and the superior columellar segment. The columellar–lobular junction marks the transition from the nasal base to the tip lobule and usually corresponds to the nostril apex (1–2 mm). The middle crus extends from the columellar–lobular junction to the lateral crus. The middle crus consists of the medial lobular segment and the more lateral domal segment. It is the domal segment that normally contains both the medial genu (the transition with the infralobular segment) and the lateral genu (the transition to the lateral crus). It is these two genu that bracket, and therefore create the anatomy of the “domal notch”. The lateral crura are made up of the lateral crus and accessory cartilages. The lateral crus is the main component of the nasal lobule. Medially, the lateral crus–domal junction line determines tip definition. Cephalically, the lateral crus has a scroll formation adjacent to the upper lateral cartilages. Caudally, the inferior border of the lateral crus diverges away from the nostril rim. Laterally, the crus passes away from the nostril rim and tapers in size. Configuration, axis of orientation and axis of curvature of the lateral crus all affect its aesthetic fabric.
The nasal base
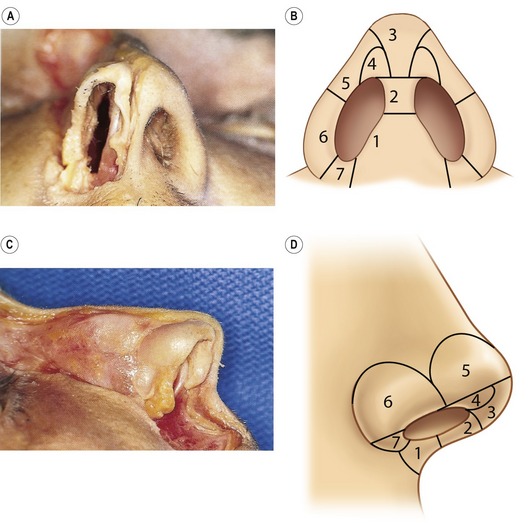
The nasal base is not a distinct anatomical entity; its aesthetic is frequently impacted by adjacent tip structures. The nasal base is subdivided into eight separate components (Fig. 39.2). The columella base consists of soft tissue, depressor septi nasalis muscle centrally, the nasalis muscles laterally and the medial crural footplates. The transverse width of the columella base is related to the separation of the footplates and the quantity of intervening soft tissue. The central columellar pillar is created by medial crura apposition; its length determined by the medial crura termination at the columellar lobular junction. The infralobular triangle and soft triangle are the capstone of the basilar pyramid and are determined by the configuration of the middle crura. The soft triangle is a reflection of the width of the domal notch and is comprised of a web of opposed skin and vestibular mucosa, which is devoid of cartilage. The lateral wall reflects the support and proximity of the lateral crura to the alar rim. The alar base is composed of subcutaneous tissue and muscle and serves as an external baffle for the nose, which determines the amount of alar flare and width. The nostril sill varies widely on its vestibular and cutaneous surfaces, and is intimately affected by the configuration of the adjacent alar base. The nostril is the central void that is determined only by its surrounding structures and is highly variable between individuals.
Technical steps
Assessing the septum and turbinates
Following Betadine preparation and subperichondrial injection with 1% Xylocaine with epinephrine, a right vestibular hemi-transfixion incision is performed and the caudal septum is identified. Sharp dissection with a Converse–Daniel scissor is performed down to the perichondrium. In order to facilitate the dissection and guarantee that you are in fact in the subperichondrial plane, cross-hatches are made on the caudal septum and then a Cottle elevator is used to elevate the mucoperichondrium and reveal the Robin’s-egg blue color beneath. The elevator is inserted dorsally parallel to the septum and a vertical sweep is done back and over the perpendicular plate of the ethmoid, and then down onto the vomer (Fig. 39.3). The inferior portion is then dissected from back to front coming from the posterior vomer forward, allowing easier separation of the fused perichondrial/periosteal fibers. If the septum has been previously harvested, this dissection is done only over the dorsal aspect of the L-strut. One must be careful separating the mucosa–mucosa adherence if the septal body has been previously harvested. If still present, cartilage harvest is accomplished with a #15 blade, septal scissors and a Cottle elevator taking great care to preserve at least a 10 mm wide L-shaped strut. If a dynamic septal collapse is present, then septal replacement grafts must be considered.
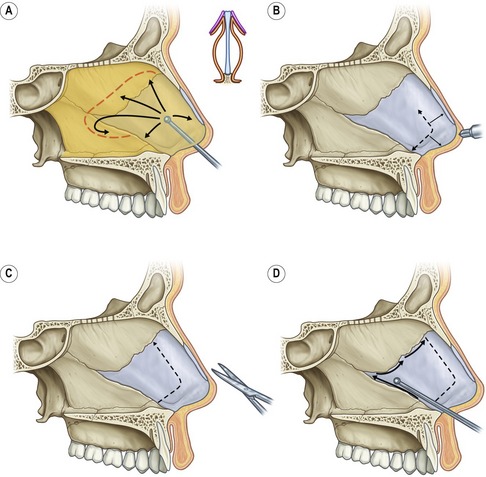
Fig. 39.3 A–D, Assessment of the septum.
With kind permission from Springer Science & Business Media: Daniel R. Rhinoplasty: An atlas of Surgical Techniques. 2002.
Opening and assessing the skin envelope
1. Closed: It is indeed the small minority of secondary cases that will be able to be performed using a closed approach. In these rare cases, either a retrograde/intercartilaginous incision, intracartilaginous/transcartilaginous incision, or an infracartilaginous incision can be utilized. The infracartilaginous incision can be used with an intercartilaginous incision for a “delivery” approach, or with a transcolumellar incision for an open approach.
2. Open: The transcolumellar incision used most commonly consists of an inverted “V” with wings, unless a different transcolumellar scar is already in place (Fig. 39.4). The apex of this 3 mm equilateral V
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree