12 Secondary deformities and the secondary facelift
Synopsis
 Although many aspects of planning and performing secondary facelift surgery are similar to those of the primary procedure, one must identify and treat not only new problems that are the product of age, but those that have resulted from any prior procedure as well. Often it is these secondary deformities that present the biggest challenge in terms of creativity, planning, preparation, and technique.
Although many aspects of planning and performing secondary facelift surgery are similar to those of the primary procedure, one must identify and treat not only new problems that are the product of age, but those that have resulted from any prior procedure as well. Often it is these secondary deformities that present the biggest challenge in terms of creativity, planning, preparation, and technique.
 Recognizing the problems in the secondary facelift patient and appreciating their underlying anatomical abnormalities is fundamental to planning and performance of any repair. Although not all problems can always be completely corrected, any surgeon able to recognize their anatomic basis can, through the application of logic and careful planning, select techniques that are safe, effective, and rational.
Recognizing the problems in the secondary facelift patient and appreciating their underlying anatomical abnormalities is fundamental to planning and performance of any repair. Although not all problems can always be completely corrected, any surgeon able to recognize their anatomic basis can, through the application of logic and careful planning, select techniques that are safe, effective, and rational.
 Secondary deformities are worth every surgeon’s consideration, even if he or she performs only the occasional secondary procedure, as they exist as compelling reminders of mistakes to avoid in the planning and performance of any primary procedure.
Secondary deformities are worth every surgeon’s consideration, even if he or she performs only the occasional secondary procedure, as they exist as compelling reminders of mistakes to avoid in the planning and performance of any primary procedure.
 Hairline displacement and disruption remain predictable outcomes of many currently used facelift plans and are a source of disappointment and frustration for patients and surgeons alike. These problems are the result of poor analysis and planning and failure to use an incision along the hairline when indicated.
Hairline displacement and disruption remain predictable outcomes of many currently used facelift plans and are a source of disappointment and frustration for patients and surgeons alike. These problems are the result of poor analysis and planning and failure to use an incision along the hairline when indicated.
 The placement of an incision and thus of the resultant scar along a hairline at secondary surgery represents a choice between two imperfect alternatives but the best overall artistic and aesthetic compromise in many patients.
The placement of an incision and thus of the resultant scar along a hairline at secondary surgery represents a choice between two imperfect alternatives but the best overall artistic and aesthetic compromise in many patients.
 Using the SMAS to lift sagging facial tissues and restore facial contour circumvents the problems associated with skin-only facelifts, as it is an inelastic structural layer capable of providing meaningful and sustained support. Although skin must be excised in SMAS procedures, only redundant tissue is sacrificed and closure can be made under normal skin tension.
Using the SMAS to lift sagging facial tissues and restore facial contour circumvents the problems associated with skin-only facelifts, as it is an inelastic structural layer capable of providing meaningful and sustained support. Although skin must be excised in SMAS procedures, only redundant tissue is sacrificed and closure can be made under normal skin tension.
 “Lamellar” dissections, in which the skin and SMAS are dissected as two separate layers, offer the important advantage that skin and SMAS can be advanced different amounts, along separate vectors, and suspended under differential tension. This allows each layer to be addressed individually as indicated and, in turn, results in a more comprehensive and natural appearing improvement.
“Lamellar” dissections, in which the skin and SMAS are dissected as two separate layers, offer the important advantage that skin and SMAS can be advanced different amounts, along separate vectors, and suspended under differential tension. This allows each layer to be addressed individually as indicated and, in turn, results in a more comprehensive and natural appearing improvement.
 It is not enough in most secondary facelift procedures to limit treatment of the neck to pre-platysmal lipectomy and post-auricular skin excision in secondary facelift patients. For many patients, subplatysmal fat accumulation, submandibular salivary gland “ptosis”, and digastric muscle hypertrophy will contribute significantly to their neck deformity and necessitate additional treatment.
It is not enough in most secondary facelift procedures to limit treatment of the neck to pre-platysmal lipectomy and post-auricular skin excision in secondary facelift patients. For many patients, subplatysmal fat accumulation, submandibular salivary gland “ptosis”, and digastric muscle hypertrophy will contribute significantly to their neck deformity and necessitate additional treatment.
 As experience is gained in evaluation of patients presenting for secondary surgery, prominent submandibular glands will increasingly be recognized as a frequent part of the secondary neck deformity and the underlying cause of objectionable residual bulges in the lateral triangle of the lateral submental region. In most instances, the secondary facelift will provide an opportunity for proper diagnosis and appropriate treatment, when present.
As experience is gained in evaluation of patients presenting for secondary surgery, prominent submandibular glands will increasingly be recognized as a frequent part of the secondary neck deformity and the underlying cause of objectionable residual bulges in the lateral triangle of the lateral submental region. In most instances, the secondary facelift will provide an opportunity for proper diagnosis and appropriate treatment, when present.
 The secondary facelift will generally require a comparatively small resection of skin and an increased focus on correcting deep layer problems and secondary deformities, depending upon the skill of the surgeon performing the primary procedure and the type of technique used.
The secondary facelift will generally require a comparatively small resection of skin and an increased focus on correcting deep layer problems and secondary deformities, depending upon the skill of the surgeon performing the primary procedure and the type of technique used.
 Secondary facelifts are often time consuming and technically demanding when compared to primary procedures and are likely to test the patience and composure of most surgeons.
Secondary facelifts are often time consuming and technically demanding when compared to primary procedures and are likely to test the patience and composure of most surgeons.
 Many patients requesting secondary facelifts are chronologically elderly, but deceptively young in appearance. A careful medical history must be taken because they often have medical problems consistent for their age group.
Many patients requesting secondary facelifts are chronologically elderly, but deceptively young in appearance. A careful medical history must be taken because they often have medical problems consistent for their age group.
 The opportunity to perform a facelift is a unique artistic privilege granted to us by our patients that carries a significant responsibility. It deserves nothing less than our best effort, and a few extra hours of our time in the operating room benefits them for the rest of their lives.
The opportunity to perform a facelift is a unique artistic privilege granted to us by our patients that carries a significant responsibility. It deserves nothing less than our best effort, and a few extra hours of our time in the operating room benefits them for the rest of their lives.
 Performing a secondary facelift if frequently a considerable undertaking and its difficulty should not be underestimated. The procedure must be carefully planned, meticulously carried out, and the patient’s safety and wellbeing unfailingly insured.
Performing a secondary facelift if frequently a considerable undertaking and its difficulty should not be underestimated. The procedure must be carefully planned, meticulously carried out, and the patient’s safety and wellbeing unfailingly insured.
 Performance of the procedure itself only fulfills part of our obligation to the patient and the care they receive perioperatively is arguably as important as the surgery itself. Diligent perioperative care will ensure the best result and reduce the likelihood that problems and complications will occur.
Performance of the procedure itself only fulfills part of our obligation to the patient and the care they receive perioperatively is arguably as important as the surgery itself. Diligent perioperative care will ensure the best result and reduce the likelihood that problems and complications will occur.
Identification and analysis of secondary aging deformity
Surgery does not halt the aging process and patients requesting secondary or tertiary facelifts usually present with many of the same problems seen when they presented for their primary procedures. This is particularly true if the primary facelift was limited and consisted of skin excision and skin tightening only. In such instances, a tight or pulled appearance will typically be present, but problems of deep layer origin will still be evident and will likely have worsened over time. These include nasolabial folds, labiomental folds, cheek ptosis, infraorbital hollowing, malar flattening, jowl laxity, subplatysmal fat accumulation, submandibular gland hypertrophy, and cervical band formation (Fig. 12.1).
Identification and analysis of secondary surgical deformities
Hairline displacement and disruption
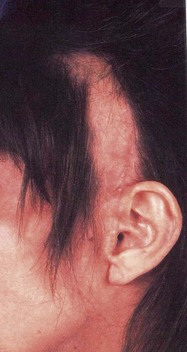
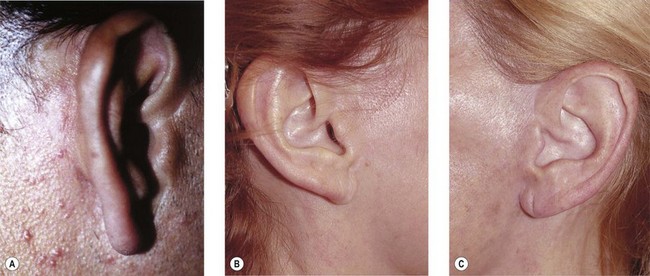
The placement of an incision and thus of resultant scar along a hairline at secondary surgery represents a choice between two imperfect alternatives but the best overall artistic and aesthetic compromise in many patients. Although incisions upon the scalp produce concealed scars within the hair, they will result in tell-tale and objectionable hairline displacement in many patients that is usually readily apparent upon casual glance and at some distance. These deformities are often not subtle and frequently result in an unnatural or even grotesque appearance (Fig. 12.2). In addition, they are uniformly difficult for the patient to disguise and a challenge for the surgeon to correct.
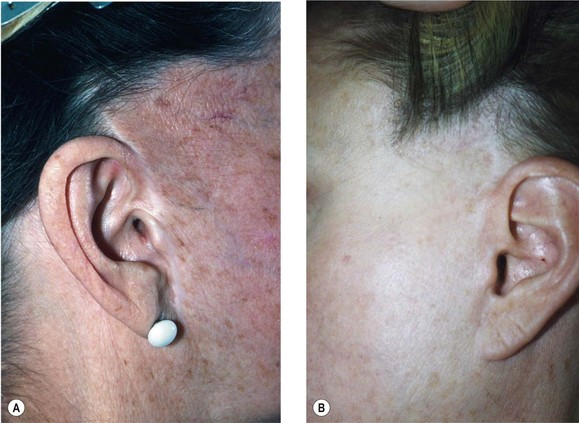
Placing the incision along a hairline, however, usually results in a fine scar only visible on close inspection when correctly planned and proper technique is used. And unlike displaced hair, a scar along the hairline can usually be easily concealed with make-up or tattooed if necessary, but generally go unnoticed in most social situations and casual encounters. Often, they are difficult to detect even on close inspection (see Fig. 12.5). Attempts to disguise displaced hair by combing adjacent hair over these areas is no more effective than the “comb-over” hairstyles worn by many balding men. Although this is perhaps preferable to the patient to having bald spots and missing hair showing, it is immediately evident that the problem is still present in most cases.
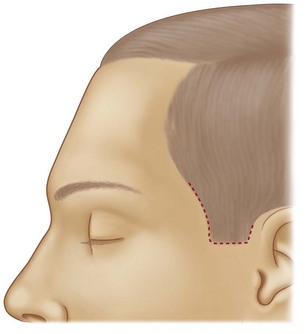
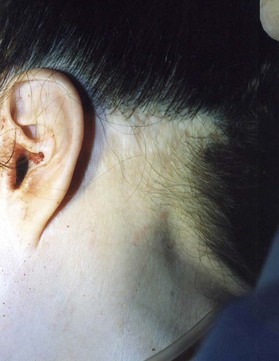
The temporal portion of the facelift incision traditionally placed within the temporal scalp will frequently result in a tell-tale and unnatural-appearing superior elevation and posterior displacement of the temporal hairline. Secondary or tertiary facelifts using the same incision plan will compound this problem and often result in a bizarre appearing and objectionable absence of temple hair (Fig. 12.3).
This can best be minimized or avoided at secondary facelift by the use of an incision along the hairline (Fig. 12.4).
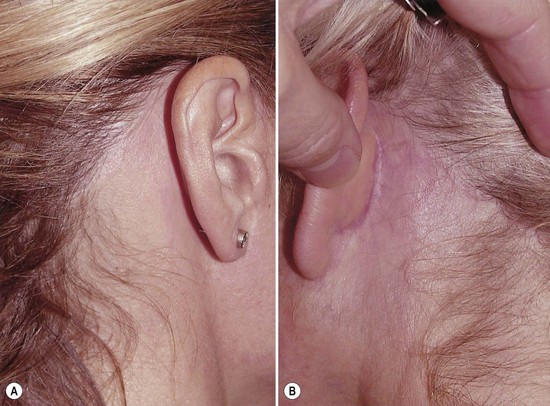
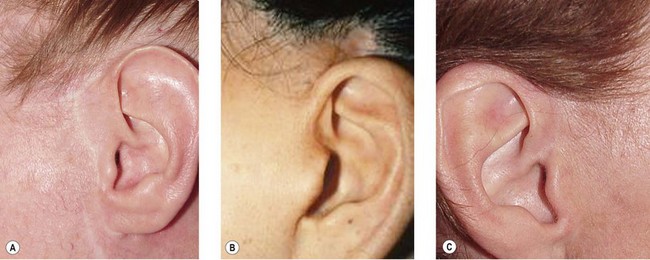
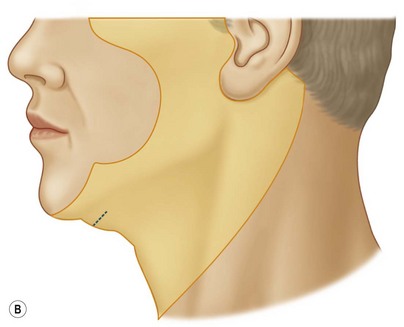
If it is appropriately planned and carefully executed, an acceptable scar will result that is artistically and aesthetically superior to additional hairline displacement (Fig. 12.5).

Fig. 12.5 (A,B) Healed incisions along the temporal hairline. The use of an incision along the hairline, when indicated, can prevent hairline and sideburn displacement without compromising the end result. Although a fine scar is present in these patients, it is not evident upon casual inspection. Note the preservation of lush temple hair and a full, youthful appearing sideburn (compare with Figs 12.2 and 12.3).
(Procedures performed by Timothy J Marten, MD, FACS.)
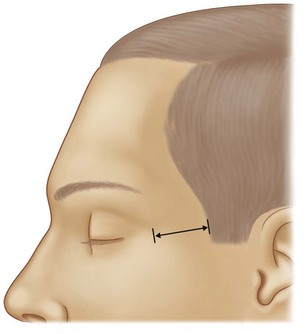
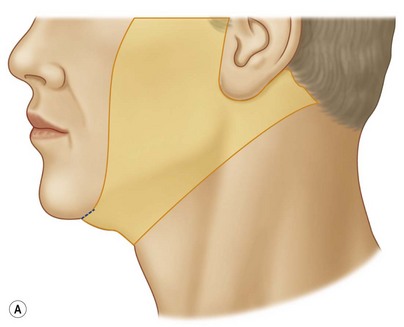
In choosing the location of the temporal portion of the facelift incision, it is important to note the degree of existing temple “skin show” (Fig. 12.6) and consider it in conjunction with skin redundancy present over the cheek (Fig. 12.7).
The occipital portion of the facelift incision is traditionally placed high upon the occipital scalp, in a well intended, but almost always counter-productive effort to hide the resulting scar. Unfortunately, any such a plan embodies an inherent defect in design that will preclude optimal improvement in the neck and frequently result in a tell-tale and unnatural appearing displacement of the occipital hairline (Fig. 12.8).
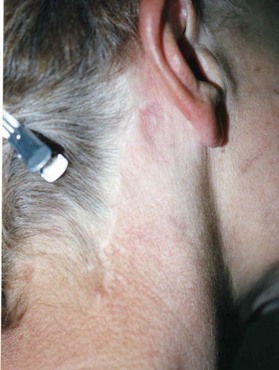
Although occipital hairline displacement may sometimes be acceptable to patients after their primary procedure, secondary or tertiary facelifts using the same incision will compound this problem and usually result in an unnatural and intolerable absence of occipital hair and notching of the occipital hairline (Fig. 12.9).
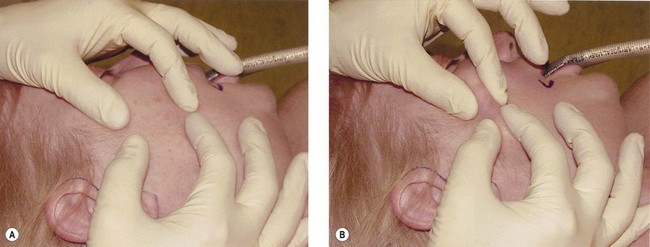
If an attempt is made to reconstitute the hairline by superior shifting of the post- auricular flap, a wide scar will usually result as the tissue discarded in any such maneuver is necessary for side-to-side head tilt and shoulder drop when the patient is in an upright position. These problems can best be minimized at the time of secondary facelift by the use of an incision along the occipital hairline (Fig. 12.10).
If the incision is appropriately planned and carefully executed, an acceptable scar will result that is artistically and aesthetically superior to additional hairline displacement. In addition, this plan will sometimes allow scalp displaced at the primary procedure to be partially advanced back towards its proper position (Fig. 12.11).
When and incision is used along the occipital hairline it should be planned in such a way that the inferior portion of the incision and thus the resulting scar is turned back into the scalp and at the junction of thick and fine hair on the nape of the neck (see Figs 12.10, 12.11). It should not be carried more inferiorly because it will be incompletely concealed and is likely to be visible to others (Fig. 12.12).
Although incisions placed along the frontal, temporal, and occipital hairlines will prevent additional hairline displacement at a secondary procedure, they do not provide for correction of large and severe problems sometime seen (see Figs 12.2, 12.3, 12.8, 12.9). In these situations, consideration must be given to the use of hair flaps, hair transplantation, and scalp expansion.
Hair loss
Hair loss is an all too common and avoidable stigmata of facelift surgery seen in many patients presenting for secondary procedures. Hair loss is generally the result of technical errors, including improperly made incisions that damage hair follicles, placement of overly tight sutures, or the closure of inadequately mobilized scalp flaps under too much tension. It may occur, however, in smokers, certain individuals with scalp disease (alopecia areata), eating disorders, or patients with a variety of systemic illness in the absence of any wrong doing on the part of the surgeon. Consideration should be given to an origin of this sort before hair loss experienced by the patient at the primary procedure is attributed to technical error. Hair loss is also frequently the result of the ill-conceived shifting of scalp flaps along the wrong vector. This is commonly seen on the temporal scalp after erroneous attempts to smooth the forehead and glabella by applying lateral traction on the forehead flap (Fig. 12.13).
Small areas of hair loss resulting from tight suture placement or attempts at spot suspension of the scalp can often be corrected at the time of secondary facelift by direct excision after adequate mobilization of surrounding tissue or by incorporation of the hairless area into a more comprehensive incision plan (Fig. 12.14).
Larger areas of hair loss resulting from excessive flap tension, an overly tight closure or ill-conceived scalp flap shifting are usually much more difficult to correct, especially if scalp excision was aggressive at the primary procedure and little residual redundancy is present (Fig. 12.15). In such instances, the patient and surgeon must accept that complete correction may not be possible at the time of secondary facelift and that hair transplantation, scalp flaps and even scalp expansion may be necessary at a later date. The goal at any secondary procedures in these patients is to select a surgical plan that does not further compound the problem.
Poorly situated scars
Poorly situated scars are typically seen in the pre-auricular, peri-lobular, and post-auricular areas. They can also be found in the submental region in many patients. Proper placement of incisions is important, particularly in the pre-auricular area, because even a thin, well-healed scar will ultimately be visible and noticed by others in most cases as a result of the gradient of skin color and texture typically present on each side of it. Although differences in skin color can sometimes be concealed with make-up, differences in texture usually cannot. Scars placed along natural anatomic interfaces tend to be overlooked by the eye however, where a gradient of color and texture is expected to be seen and where the scar appears to be a natural crease on the face. Make-up becomes less necessary as the scar is lost in shadow, appears to be a natural part of the face, or is mistaken to be a reflected highlight (Fig. 12.16).
The pre-auricular region is a common point of reference for those seeking to identify the facelift patient, and, as such, it is of concern to patients and worthy of careful consideration by the surgeon. The pre-helical portion of the pre-auricular scar is often situated too far anteriorly in the patient presenting for secondary surgery and the illusion of the scar as an anatomical feature is lost. Moving this scar so that it rests in the helical-facial sulcus will result in a less conspicuous scar and a more natural appearance. This is generally possible in most secondary and tertiary cases if skin resection has not been overly excessive at prior procedures (Fig. 12.17).
Although it is not possible to move a pre-tragal scar to a “retro-tragal” position along the margin of the tragus in every patient presenting for secondary surgery, this is preferred when possible, for the reasons outlined above (Fig. 12.18). The feasibility of relocating a pre-tragal scar to a retrotragal position will depend on the amount of cheek skin redundancy that remains after the primary procedure. Because preoperative assessment of residual cheek skin redundancy can be difficult and exceedingly deceptive at the tragus, it is sometimes best to make the initial incision along the existing pre-tragal scar, when present. The decision to sacrifice the remaining skin over the tragus and move the scar to the tragal margin can then be delayed until after cheek flaps have been mobilized, SMAS advanced, and the actual amount of cheek skin recruited through these maneuvers, if any, determined. Often, skin recruited is needed to recreate an absent pre-tragal sulcus and to correct a “buried tragus” deformity. In such instances, relocation of a pre-tragal scar to the margin of the tragus will not be possible and the existing pre-tragal location of the scar must be accepted. If the secondary facelift incision is initially made along the margin of the tragus when a pre-tragal scar is present but before intraoperative assessment of skin redundancy can be made, needed skin may be erroneously excised. This will force an inappropriately tight closure and result in tragal distortion, tragal retraction, and obliteration of the pre-tragal sulcus.
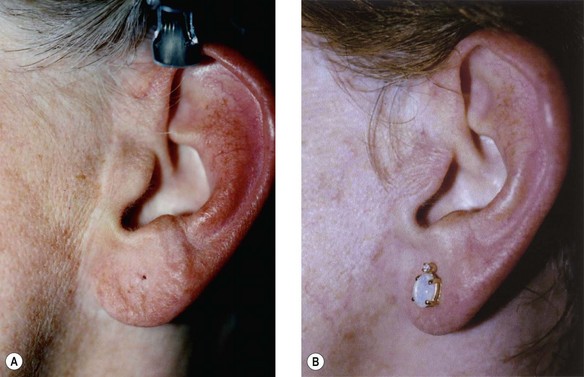
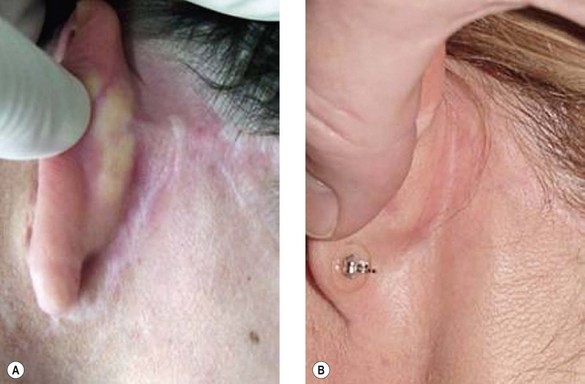
The peri-lobular area is a common location for poorly situated facelift scar in secondary and tertiary facelift patients. Typically, it is low lying due to poor planning and the skin settling that occurs after “skin only”, non-SMAS facelift techniques (Fig. 12.19).
A poorly situated post-auricular scar, although not as readily apparent and easier to disguise in most social situations than a poorly situated scar in the pre-auricular region, is nonetheless an objectionable deformity that should be corrected when possible. Typically, the poorly situated post-auricular scar will be seen to lie outside the auriculo-mastoid sulcus, and too low over the mastoid to be concealed by the pinna. Such a deformity is the result of poor planning and inferior–posterior migration of the post-auricular flap due to excessive tension placed upon it at the primary procedure (Fig. 12.20).
The submental incision will frequently be seen to have been erroneously placed directly along the submental crease in a well-intended effort to hide the resulting scar (Fig. 12.21). Regrettably, this serves only to reinforce the submental retaining ligaments and accentuate a “double chin” or “witch’s chin” appearance. In such situations, consideration should be given to moving the submental incision 1–2 cm posterior to the crease so that the existing scar car be undermined and released. Although this results in a new scar, it will be inconspicuously hidden in the shadow of the mandible in all but the unusual case (Fig. 12.22). This is preferable and a worthwhile trade-off for correction of the more obvious and objectionable contour deformity that would result if the incision were made again in the same place upon the existing scar. If limited work in the neck only is needed and minimal or no double chin deformity is present, it may be possible and appropriate to use an existing scar in the submental crease as the site for secondary incision. If more extensive maneuvers are required and a marked double chin deformity is present however, a new more posteriorly situated submental incision is indicated (Fig. 12.23).
If skin excision has been aggressive and excessive at the primary procedure, relocation of poorly situated scars may not be possible at the time of request for secondary facelift, regardless of how much the patient and surgeon would wish otherwise. These patients have typically undergone aggressive skin-only, non-SMAS procedures and have overly tight faces with wide and/or hypertrophic scars (Fig. 12.24). Often earlobes have been pulled or placed too far inferiorly into the cheek as well, compounding the problem. In such cases, it is usually best to defer surgery until scars are mature, skin has relaxed, and adequate tissue is available to make proper repair. In most cases, this will mean waiting until 2–3 cm or more of skin can be pinched up along each jaw line along a line extending from the chin to the lobule. Re-operation in the absence of adequate skin to make proper repair will be a frustrating act of futility in which little if any benefit will be gained.
Wide scars
Because the factors underlying suboptimal healing leading to wide or hypertrophic scars are still present to some extent in the patient requesting secondary surgery, each must be approached with caution. Like the patient with a skin shortage and poorly situated scars, the patient with wide or hypertrophic scars may be impossible to effectively treat if skin excision has been excessive at the primary procedure (Fig. 12.25). This is true, regardless of how much the patient and surgeon wish otherwise. Re-operation in the absence of adequate skin to make proper repair will be a frustrating act of futility in which little, if any, benefit will be gained.
Cross-hatched scars
Cross-hatched scars are a completely avoidable deformity commonly seen in patients presenting for secondary facelift. Like most secondary facelift deformities, they are the product of errors in both planning and technique. The underlying cause of most cross-hatched scars can be traced directly to skin tension and tension-based facelift techniques. When incisions are closed under tension, larger sutures must be used, and these must be tied tighter and left in longer. Inevitably, varying degrees of necrosis occur beneath each, and these spots go on to heal as scars. As skin relaxation occurs over time the hatch marks and suture hole scars stretch and migrate away from the incision scar, giving the appearance that the wound was closed in a crude fashion with large, widely placed sutures. Almost always cross-hatched scars are accompanied by other signs of over reliance on skin tension including hairline displacement, hypertrophy, and wide scars (Fig. 12.26).
Distortion of tragal anatomy
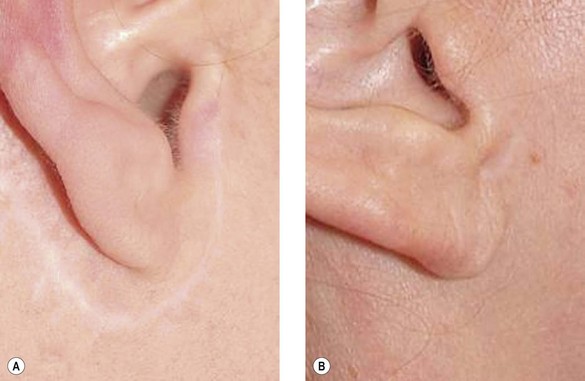
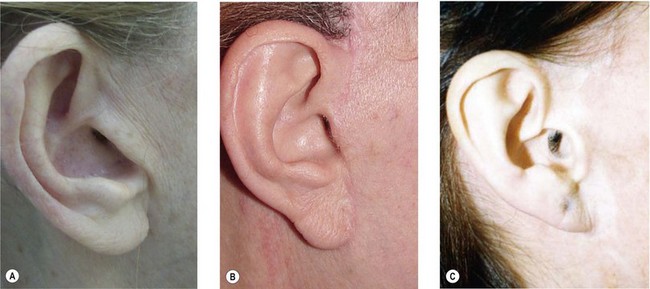
The most commonly observed forms of tragal distortion seen in patients presenting for secondary facelift are loss of tragal contour and obliteration of the pre-tragal sulcus. These are frequently seen concurrently, although they have somewhat different underlying causes. Loss of tragal contour is usually the result of improper incision planning, superior overshifting of cheek skin, and imprecise trimming of the tragal skin flap. The tragus is seen to have no distinct beginning or end and no posterior projection. A tell-tale “chopped-off” appearance results (Fig. 12.27A). This is generally correctable if tension is diverted to the SMAS, skin can recruited from secondary advancement of the cheek skin flap, and the skin flap is properly trimmed and fit over the tragal cartilage.
Loss of the pre-tragal sulcus results from failure to leave enough skin to fill the pre-tragal depression when the tragal flap is trimmed and is almost unavoidable in any technique in which tension is placed on the cheek skin flap. The over-trimmed skin flap bridges the pre-tragal sulcus which in turn is gradually filled with fibrotic tissue and scar over time. The tragus appears “buried” and indistinct from the cheek anterior to it. It can also be seen to have a flat, two-dimensional contour (Fig. 12.27B).
The “retracted tragus” represents an extreme case of the “buried tragus” deformity. It too, is the result of technical error and has its origin in an overly tight and excessively trimmed cheek skin flap. The retracted tragus deformity differs from the buried tragus deformity, however, in that not only is the pre-tragal sulcus obliterated by subcutaneous scar, but the tragal cartilage itself is pulled anteriorly by the over-trimmed skin flap. This results in an open auditory canal and a tell-tale and unnatural appearance (Fig. 12.27C). Simple recruitment of skin from the cheek and excision of pre-tragal subcutaneous scar is not sufficient to correct the retracted tragus deformity because the retracted tragal cartilage is usually stiff, fibrotic, and unable to return to its natural position and configuration on its own. Correction usually requires that the cartilage be scored on its anterior surface and then secured with a mattress suture once in its proper anatomic position (Fig. 12.28).