Abstract
Second intention healing and primary closure are fundamental reconstruction options in dermatologic surgery. In general, second intention healing is best suited for wounds where the surrounding skin has a normally shiny texture, where wound contraction will not cause anatomic distortion, and where the base of the wound has a strong blood supply. Although numerous factors can influence the outcome of second intention healing, predictably good results are often seen on the temple, forehead, bald scalp, and pretibial leg. Primary closure is the workhorse reconstructive technique in dermatologic surgery. Adherence to the following design principles will optimize outcomes: preservation and restoration of free margins, preservation and restoration of normal contour, orientation of scars along cosmetic subunit junction lines, and orientation of scars along relaxed skin tension lines. While all principles are important, preservation and restoration of free margins and normal contour should be prioritized. Variations of primary closure for special circumstances include crescentic excision, S-plasty, M-plasty, and serial excision. With proper surgical technique and wound selection, second intention healing and primary closure can lead to excellent cosmetic outcomes while avoiding complications.
Keywords
second intention healing, primary closure, reconstruction, dermatologic surgery
Introduction
Second intention healing (SIH) and primary closure are the most common and basic strategies to manage wounds after skin cancer removal. SIH is defined as allowing a wound to heal without suturing together the edges. Primary closure refers to direct approximation of the wound edges with sutures. For the purposes of this chapter, “primary closure” refers to a linear, or side-to-side, closure of a wound. This chapter will discuss SIH and primary closure to manage defects after removing skin cancers and other cutaneous lesions.
Second Intention Healing
Phases of Wound Healing
Healing wounds progress through a sequence of overlapping phases: inflammation, proliferation, and remodeling ( Fig. 3.1 ). The inflammatory phase, which occurs during the first 24 to 48 hours after injury (and can last up to 2 weeks), is defined by a cellular and vascular response. This is followed by the proliferative phase, which is characterized by angiogenesis, fibroplasia, and re-epithelialization. The remodeling phase, which can last for weeks to years, is distinguished by the deposition of different matrix materials, whose composition changes over time as the scar matures.






Healing time depends on several variables, including blood supply, wound size, and host factors. Wounds with a strong blood supply and more adnexal structures heal faster. For example, facial wounds have a robust blood supply and heal faster than wounds on the lower extremity. Deeper wounds require a longer proliferative phase for granulation tissue to fill the wound. Broader wounds take longer to heal, although healing time is not linearly proportional to wound diameter. For example, a 10-fold increase in the area of a wound may only double the healing time. The health and nutritional status of the patient may also affect healing time. For example, lower extremity wounds may require excessive healing time in vasculopathic patients. Since numerous factors affect wound healing, it is not possible to generalize healing time for all wounds.
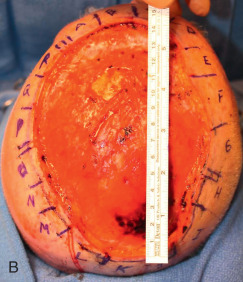
Wound contraction, which commences during the proliferative phase and extends into the remodeling phase, can account for a significant decrease in the size of the wound ( Fig. 3.2 ). The wound contracts in three phases: a plateau phase, an exponential phase, and a postexponential phase. During the exponential phase, the rate of contraction occurs in a logarithmic fashion related to the area of the wound, which explains why overall healing time is not linearly proportional to the area of the wound and why larger wounds often heal faster than expected. The amount of contraction varies widely, depending on the depth and the anatomic location. Wounds on the relatively thick and inelastic tissue of the scalp may contract by 45% of their original size, whereas wounds of the medial canthus may contract by up to 78%. Myofibroblasts begin to mediate wound contraction as early as 5 days after injury. Partial thickness dermal wounds contract less than full-thickness wounds, and adnexal structures in the residual dermis speed re-epithelialization.



Appearance of Second Intention Healing Scars
SIH produces scars that have a shiny texture and lack skin appendages, such as hair follicles and eccrine glands. Telangiectases usually develop on the scar’s surface, especially in patients with lighter skin types. Larger wounds tend to heal with larger caliber vessels on the central surface. Smaller vessels along the periphery of the scar may fade as the scar matures and becomes relatively avascular. A newly re-epithelialized scar is pink, but scars often become hypopigmented in lighter skin types and hyperpigmented in darker skin types.
Ideal Wounds for Second Intention Healing
SIH is ideal for wounds where the surrounding skin has a normally shiny texture, where wound contracture will not result in anatomic distortion, and where the blood supply at the base of the wound is robust. Many factors can influence outcomes for SIH. Certain anatomic locations are ideal for second intention healing. On the temple, forehead, bald scalp, and pretibial leg, the shiny scars formed by SIH often heal with good results and minimal morbidity ( Fig. 3.3 ). SIH may be a good option for wounds of the hands and feet, as long as tendons are not exposed and the wound does not cross joints. The pink scars from SIH mimic the natural color and texture of the vermilion lip, and the cosmetic result is often highly aesthetic.


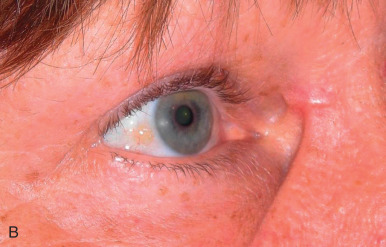
The contour of the anatomic site has traditionally been considered to be a good predictor of aesthetic outcome. Wounds have been considered to heal with better aesthetic outcomes on concave versus convex surfaces. However, this dogma is an oversimplification. For example, while SIH is often utilized for wounds of the concave medial canthus and can sometimes result in excellent outcomes ( Fig. 3.4 ), SIH in this location will often create webbing from tension on the nearby eyelid skin ( Fig. 3.5 ). SIH of the concave alar groove may result in webbing or elevation of the alar margin. By contrast, SIH can be an excellent option for wounds on convex surfaces, such as the forehead and bald scalp, which have normally shiny, taut skin.




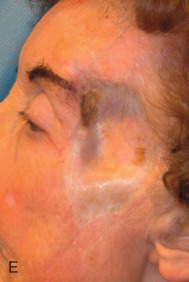
The texture and color of the surrounding skin may influence the appearance of SIH scars. The shiny scar from SIH may contrast sharply in locations with textured skin, such as a sebaceous nasal tip ( Fig. 3.6 ). By contrast, the shiny scar from SIH is often inconspicuous in locations with tight, shiny skin, such as the ear. The surgeon must anticipate the likely result from a primary closure versus SIH. In some locations, such as the upper back and shoulders, linear scars have a tendency to spread and often become more noticeable than a smaller circular scar from second intention healing.

Suboptimal Wounds for Second Intention Healing
Some wounds have predictably poor outcomes from SIH. Wounds near the eyelid, ala, and lip may contract and distort these free margins ( Fig. 3.7 ). SIH of wounds with exposed “white structures,” such as bone, cartilage, and tendons, may result in desiccation and prolonged healing. If soft tissue coverage of exposed bone and cartilage is not possible, fenestration of exposed cartilage and burring of exposed bone may improve the blood supply and promote healing ( Fig. 3.8 ). Finally, SIH may distort contours when wound contraction places tension on nearby loose skin.






Patient Factors Affecting Decisions About Second Intention Healing
Patient-specific factors may influence decisions about SIH. Patients must be willing and able to care for the wound until healing is complete. Patients with poor dexterity and vision may not be capable of independent wound care. A caretaker may be necessary for wounds in difficult-to-reach anatomic locations. Patients who are active or have wounds in visible areas may prefer reconstruction to speed healing. Finally, patients with limited income may not be able to afford expensive wound care supplies.
Second Intention Healing as an Adjunct to Reconstructive Surgery
SIH may supplement reconstructive surgery. SIH may prepare some wounds for better outcomes after skin grafting. If immediate skin grafting will not restore contour of deep wounds, grafting may be delayed until granulation tissue has filled the wound bed ( Fig. 3.9 ). Wounds that cross concavities, such as the alar groove, may benefit from partial reconstruction with a local skin flap and SIH of the portion of the wound at the alar groove. To avoid retraction after SIH of wounds near the alar margin, free cartilage grafts may first be placed at the base of the wound. To speed healing, purse-string closures may shrink the wound size prior to SIH.




Wound Care During Second Intention Healing
Two Cochrane reviews of dressings, topical agents, and antibiotics for use during SIH both concluded that there is a lack of high-quality studies showing superiority of any particular regimen. A relatively basic regimen is usually sufficient. The wound is initially covered with petrolatum and a nonadherent, absorbent pressure dressing that remains in place for 24 to 48 hours. After this period, the wound may be cleansed with a mild soap and water once or twice daily, and kept moist with petrolatum and a bandage until re-epithelization is complete. The moist environment prevents crust formation, decreases pain, and accelerates healing. When crusting or scabbing occurs, manual or enzymatic debridement may be necessary to reduce delays in the healing process. SIH has consistently been associated with less postoperative pain than other reconstructions and has a low incidence of infection with proper wound care.
Complications
Failure to account for contraction can lead to anatomic distortion after SIH of wound near free margins, such as the nasal ala and eyelid. Formation of excess granulation tissue can delay healing ( Fig. 3.10 ). High potency topical steroids reduce granulation tissue and speed healing. Erosive pustular dermatosis is thought to be associated with trauma, and can occur with SIH. As it is easily confused with infection, the surgeon must be aware of this potential complication. It is commonly treated with topical corticosteroids. Newly re-epithelialized wounds tend to be more fragile and can be easily sheared with incidental trauma. Contour of the healing wound is unpredictable, so wounds may heal with either hypotrophic or hypertrophic scars.