Sclerotherapy of Large Varicose Veins
 GENERAL PRINCIPLES
GENERAL PRINCIPLES
No matter what the size, all varicosities result from an elevated venous pressure that produces dilatation of the vein walls. To effectively treat large varicose veins, abnormal sources of high pressure must be found and eliminated. In treating veins of any size by any method, the best results will be obtained when the treatment plan is based on a complete understanding of the anatomy of the refluxing circuit. Main high-pressure reflux points should be treated first, even though more distal areas may be more visibly disturbing to the patient.
When a correct underlying diagnosis has been made and an appropriate treatment plan developed, sclerotherapy can be an effective therapy for veins of any caliber. However, the larger and more proximal the reflux entry point, and the higher the pressure at that point, the greater the likelihood of early recurrences.
Although there is a widespread preference for endovenous ablation in patients with junctional incompetence, successful sclerotherapy of the saphenofemoral junction (SFJ) is possible under Duplex guidance.1 Many experienced practitioners do use sclerotherapy for junctional incompetence, but sclerosis of truncal varices with high-grade junctional reflux often requires special techniques and high-potency sclerosants that are not part of the basic armamentarium. The inexperienced phlebologist is unlikely to have success in such efforts and this is not accepted standard of care in the United States. A reasonable rule of thumb is that if maneuvers such as Valsalva can elicit reflux through the SFJ with the patient supine, the junction probably will be resistant to basic methods of large vessel sclerotherapy.
Varicosities that arise from perforator incompetence usually are amenable to sclerotherapy, no matter how large and convoluted they may appear.2 Large varices can be as much as 30 mm or more in diameter, but the same basic approach is useful for all vessels in which reflux can be identified. Principles of large-vein sclerotherapy are listed in Table 12-1.
TABLE 12-1
Principles of Large Vein Sclerotherapy
• Identify and treat specific reflux points
• Proximal to distal is the order of treatment
• Treat larger veins before smaller veins
• Empty vein of blood by various maneuvers
• Treat entire varicosity at one time
• Compress immediately and adequately
• Patient ambulates following treatment
Make a Correct Diagnosis
It is possible to have a certain amount of short-term success with the occasional patient simply by injecting sclerosants into any visible spider veins and varicose veins. However, this haphazard approach will not lead to a successful phlebology practice, because the number of treatment failures and of complications will be too much high. Long-term success depends upon first making the correct diagnosis: identifying the sources of reflux that have caused the problem and that will cause it to recur if not properly treated.
 STEPS PRIOR TO TREATMENT
STEPS PRIOR TO TREATMENT
When patients present for treatment of varicose veins, history and physical examination are very important (see Chapter 25 for appropriate questionnaires and forms). The patient’s legs must be thoroughly examined with the patient standing so that more subtle varicosities may become visible. Noninvasive testing (see Chapters 6, 8, 9, and 10) is critical to establish the abnormal anatomy. As discussed above, a malfunctioning SFJ must be corrected before distal associated varicosities are treated.
Education and consent of the patient are also important (see Chapter 11). Contraindications to sclerotherapy treatment must be investigated (Table 12-2). After photographs are taken and pre- and posttreatment instructions reviewed, one may proceed with a first treatment “test” injection. The first treatment session is usually limited to a small number of sites of telangiectasias rather than varicosities, for several reasons. One can thus observe the patient for any allergic reactions, judge the effectiveness of a particular concentration and class of sclerosing agent, and observe any reactions to the tape or foam pads used for compression. It also serves to familiarize the patient with sclerotherapy, the treating physician, clinic surroundings, and the sensation of the fine needle. The test site also complies with the recommendation of the manufacturer (Angiodynamics/Henry Schein) in the package insert of sodium tetradecyl sulfate. Although the package insert of the newly available Asclera® (polidocanol) (Merz Aesthetics, USA), does not require a test injection.
TABLE 12-2
Contraindications to Sclerotherapy
• Bedridden patient
• Severe arterial obstruction
• Diabetes (severity dependent)
• History of deep venous obstruction with antegrade flow in varicosities
• Allergy to sclerosing agent or urticaria after previous treatment
• Hypercoagulable states—may predispose thrombosis extending into the deep venous system
• Pregnancy (compression is treatment of choice)
• Massive obesity
• Poor tolerance of support hose
• Uncontrolled medical condition
If a patient presents with bulging varicosities, a strong family history of varicose veins, an extensive reticular network, and prominent blushing or telangiectasia around the ankle, or has symptoms of leg pain or swelling, a screening Doppler or Duplex examination will be performed at the first visit. If the screening is positive for large vessel incompetence, a full Duplex mapping of the affected leg is performed prior to the patient’s first full treatment session (Chapter 10).
Adopt an Appropriate Treatment Plan
1. Start with reflux entry points: Whether the treatment of larger veins is by ablation or by sclerotherapy, the principal site of high-pressure reflux must be corrected first. If it is not controlled, the patient will nearly always suffer the early reappearance of spider veins and varicose veins—either newly recruited vessels or treated vessels that have reopened. Every treatment plan is aimed first at the ablation of high-pressure reflux, and only secondarily at the ablation of superficial vessels that may be of more concern to the patient.
2. Treat proximal varices before distal telangiectasia: Proximal vessels and larger vessels are most often conduits that deliver high pressure to smaller, more distal vessels; thus, treatment generally should move from proximal to distal and from larger to smaller vessels. Patients often try to insist that the most visible vessels be treated first, even if they are smaller and more distal. Thorough explanation of the treatment rationale will usually convince the patient to follow the physician’s recommendations. Unassociated telangiectasias can be treated at any point.
3. Pitfalls of beginning treatment distally. There are several problems that often arise when an area of distal branch varicosities or spider veins is treated without first addressing the principal site of reflux. Once the most obvious vessels are gone, the patient may consider the treatment complete and may fail to return for treatment directed at the site of reflux. This leads to early recurrence in nearly every case. In some cases, distal varicosities serve as a “runoff” conduit that reduces the pressure in the refluxing circuit by allowing reflux to reenter the deep veins at a more distal location. When this is the case, closing the distal veins before addressing the proximal reflux causes an immediate rise in static pressure in the circuit. This often causes a very rapid appearance of large numbers of new exuberant telangiectasia that are very distressing to the patient (Figure 12-1). Sclerotherapy beginning with distal vessels may cause secondary thrombosis of more proximal segments, making it impossible to inject the proximal segments at a later visit. Lacking a sufficient endothelial injury, the thrombosed vessel will recanalize and the original problem will recur.

![]() FIGURE 12-1 New telangiectasias occurring at a site of previous treatment in which a distal outflow vein has been sclerosed. Treatment of the proximal refluxing vein might have prevented this.
FIGURE 12-1 New telangiectasias occurring at a site of previous treatment in which a distal outflow vein has been sclerosed. Treatment of the proximal refluxing vein might have prevented this.
4. Treat an entire vessel at one time: When one portion of a varicosity is treated and another is not, the untreated segment often becomes thrombosed and feels hard and tender. However, since there has been no real endothelial destruction, that portion of the vessel recanalizes quickly and appears as a treatment failure.
5. Empty veins of blood before/after injecting: Any blood remaining in the vein will serve to dilute the injected sclerosant, rendering it less effective. Maneuvers that can reduce the amount of blood in the vein will lead to a better result with a lower initial concentration of the sclerosant. Reducing the amount of blood also theoretically reduces the risk of post-sclerosis pigmentation. Most commonly, this is accomplished by treating the patient while supine on a power table. The legs may be in a neutral position or the table may be tilted in reverse Trendelenberg to further reduce blood volume in the veins. After the injection, the leg can be elevated to drain the blood. Manual compression can be done first, followed by compression with pads and wraps. Finally, the vein can be compressed posttreatment by the application of 30- to 40-mmHg compression hose.
6. Maintain compression after treatment: Effective ablation of a treated varix is much more likely when collagen microfibrils can span the entire vessel from wall to wall, and this is more likely when the vessel is kept compressed after treatment. Compression also reduces the amount of intravascular coagulum (posttreatment thrombus) in the treated vessel, thus reducing pain, inflammation, bruising, and hemosiderin deposition in the tissues. Compression is also desirable because it is an effective form of prophylaxis against deep vein thrombosis in the posttreatment period.
7. Keep the patient ambulatory: Injection sclerotherapy produces local endothelial injury and alteration of circulating coagulation and fibrinolytic factors. This increases the theoretical risk of deep venous thrombosis. To prevent this complication, it is extremely important that venous stasis be avoided after sclerotherapy. Together with compression, increased ambulation is an important way to prevent or reduce thrombus formation.
8. Reassess the diagnosis when necessary: Whenever a patient fails to respond to treatment as expected, the underlying diagnosis should be called into question. Although some patients can be very resistant to treatment, most treatment failures result because previously unrecognized high-pressure points have been left untreated. Duplex ultrasound examination is extremely helpful in reassessing a patient who has failed treatment or who has had an early recurrence after apparently successful treatment.
 TECHNIQUE FOR SCLEROTHERAPY OF LARGE VARICES
TECHNIQUE FOR SCLEROTHERAPY OF LARGE VARICES
If the varicosity is superficial and easily visible from the surface of the skin, sclerotherapy may be performed without Duplex guidance (Figure 12-2). A 27- to 30-gauge needle on a 3-cc syringe is often employed for this technique. The needle is advanced while aspirating the syringe until aspiration of dark venous blood indicates penetration of the lumen. At this point, 0.5–1.0 cc of concentrated or foamed sclerosant is slowly injected at the site. If any resistance is felt while advancing the needle plunger, if disruption of the vein is detected, or if the patient experiences severe pain, the injection is immediately stopped. The most common concentrations and dosages of sclerosants are listed in Table 12-3. The needle is withdrawn and redirected to the next site. At the conclusion of treatment, the vein should visually be seen contracted. Examples of successful varicose vein treatment are shown in Figure 12-3.
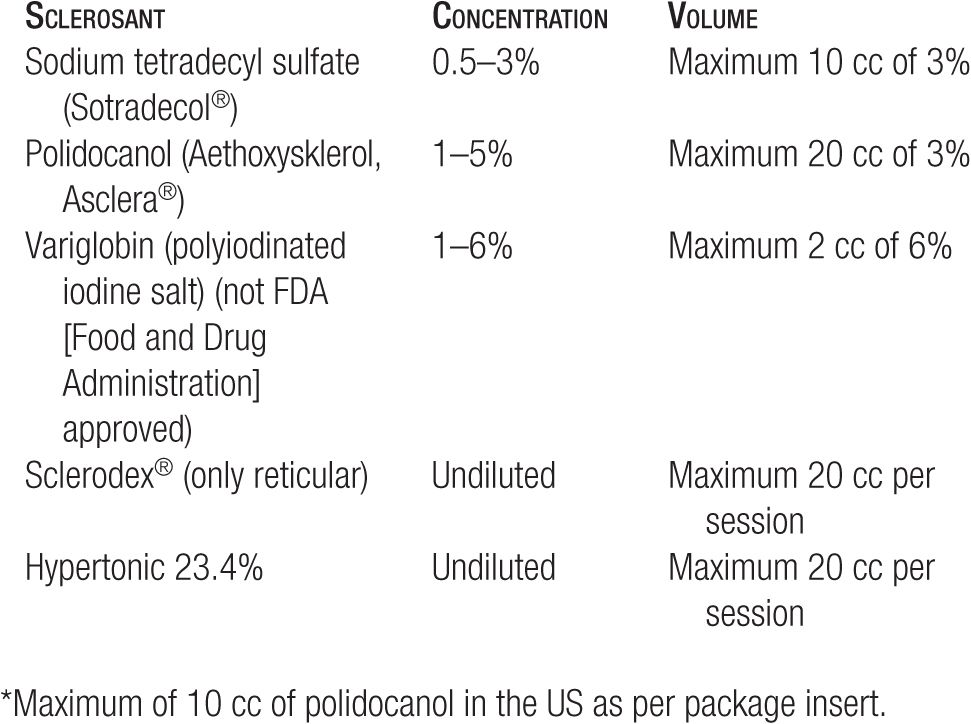
TABLE 12-3
Dosage of Sclerosants for Large-Vein Sclerotherapy
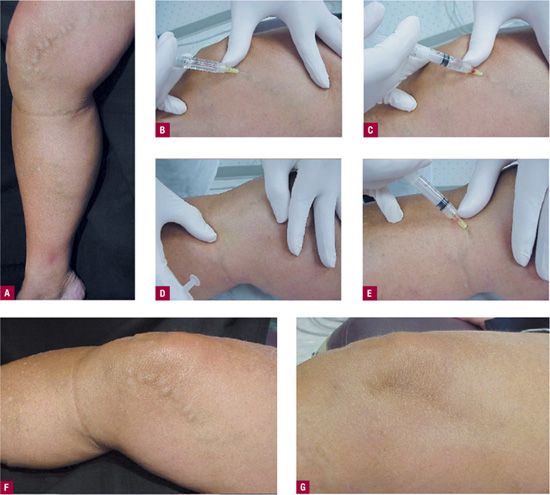
![]() FIGURE 12-2 Method of large-vein injection by the supine direct cannulation technique. A.
FIGURE 12-2 Method of large-vein injection by the supine direct cannulation technique. A.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


