16 Scar prevention, treatment, and revision
Synopsis
 From our most precise aesthetic work to our most challenging reconstructive cases, preventing and treating problem scars are key to patient satisfaction and good surgical outcomes. Understanding scarring determines our surgical planning, our approach, and our technique. In follow-up care, minimizing scarring can lead to both improved form and function. Even long after recovery, patients with pathologic or abnormal scarring may seek the expertise of a plastic surgeon for scar revision. And the most senior of surgeons can attest to the challenges of managing scarred tissue in reoperative surgery.
From our most precise aesthetic work to our most challenging reconstructive cases, preventing and treating problem scars are key to patient satisfaction and good surgical outcomes. Understanding scarring determines our surgical planning, our approach, and our technique. In follow-up care, minimizing scarring can lead to both improved form and function. Even long after recovery, patients with pathologic or abnormal scarring may seek the expertise of a plastic surgeon for scar revision. And the most senior of surgeons can attest to the challenges of managing scarred tissue in reoperative surgery.
 To begin to tackle these obstacles, plastic surgeons have created an arsenal of tools based on the central tenets of our discipline. Published in 1957 by Gillies and Millard, The Principles and Art of Plastic Surgery defined the fundamental doctrines of plastic surgery and has formed the foundation of our field.1 Operative scar treatment and revision rely on these principles. Ideas such as diagnosing before treating, making a plan, marking landmarks, “borrowing” tissue from areas that have it to give, and restoring the beautiful normal frame our approach to managing scars. Rather than having a single operation for each defect, the plastic surgeon is charged with crafting these principles to the individual patient.
To begin to tackle these obstacles, plastic surgeons have created an arsenal of tools based on the central tenets of our discipline. Published in 1957 by Gillies and Millard, The Principles and Art of Plastic Surgery defined the fundamental doctrines of plastic surgery and has formed the foundation of our field.1 Operative scar treatment and revision rely on these principles. Ideas such as diagnosing before treating, making a plan, marking landmarks, “borrowing” tissue from areas that have it to give, and restoring the beautiful normal frame our approach to managing scars. Rather than having a single operation for each defect, the plastic surgeon is charged with crafting these principles to the individual patient.
 To our surgical armamentarium we’ve added our growing understanding of scar biology. Fetal models have shed light on the complex factors which determine scarring versus scarless wound healing. In addition, we have deepened our understanding of the mechanisms that lead to pathological hypertrophic and keloid scar formation. Advances in cell and tissue biology have revealed many new therapeutic targets currently under active investigation.
To our surgical armamentarium we’ve added our growing understanding of scar biology. Fetal models have shed light on the complex factors which determine scarring versus scarless wound healing. In addition, we have deepened our understanding of the mechanisms that lead to pathological hypertrophic and keloid scar formation. Advances in cell and tissue biology have revealed many new therapeutic targets currently under active investigation.
 Despite our tools and advances, each treatment, nevertheless, begins with the patient. A good treatment outcome is rarely achieved without first understanding the patient’s antecedent experience, current complaints, and future expectations. Herein we will describe important aspects in approaching a scarred patient, assessing a scar and understanding scar biology. We will then focus on strategies in preventing, treating, and revising scars. These strategies increasingly reflect both modern advancements in medicine as well as time-proven principles of surgery.
Despite our tools and advances, each treatment, nevertheless, begins with the patient. A good treatment outcome is rarely achieved without first understanding the patient’s antecedent experience, current complaints, and future expectations. Herein we will describe important aspects in approaching a scarred patient, assessing a scar and understanding scar biology. We will then focus on strategies in preventing, treating, and revising scars. These strategies increasingly reflect both modern advancements in medicine as well as time-proven principles of surgery.
Personal and social significance of scars
Scars may arise from both culturally sanctioned and prohibited practices. Ritual scarring, or cicatrization, was an important part of identifying tribal belonging in parts of Africa and Australia.2 In tribal communities in Sudan and Papa New Guinea, the prevalence of keloid formation in certain racial groups has been exploited for spiritual and cultural markings. Likewise, the Japanese art of tattoo, or irezumi, carried sufficient cultural weight as to be banned until 1945, when occupational forces again legalized its practice. Today tattooing and, to a lesser degree, branding and scarification, continues to be a popular form of self-expression. While accepted to some degree within society, the psychology of these scars may overlap with that of the more pathologic, but no less intentional, scars of self-injury and self-mutilation.3
In western culture, scars often carry a sinister or menacing connotation. Gender clearly plays a role in the effect of scars. A recent study suggests that some facial scars in men signal risk-taking and bravery, being perceived as more attractive.4 This effect was not found when observers were shown similarly scarred women. Nevertheless, many scars clearly carry negative social implications for both genders. Studies of quality of life measures in burn patients reveal significant interference with physical comfort as well as social and work life.5 Depression and posttraumatic stress disorder (PTSD) have been identified as potential long-term sequelae. Rates for PTSD in burn patients range from 23% to 45% at 1 year following injury.6 Risk factors include avoidant coping strategies and pre-existing psychiatric history as well as hand and face involvement and burn severity.7 Understanding what specific aspects of the patient’s life are most hampered can help direct both medical and nonmedical therapy.
Psychologist Thomas F Cash described the importance in reconciling a patient’s “view from the outside” and “view from the inside” in coping with deformity.8 Understanding the social context and patient’s emotional relationship to scars is, therefore, vital to treatment. A potentially useful tool in understanding and assessing these variables is Psychological Aspects of Reconstructive and Cosmetic Plastic Surgery: Clinical, Empirical, and Ethical Perspectives.9 Published in 2006, this title reflects a multidisciplinary effort of leading psychologists, psychiatrists, and surgeons in determining and delivering care to patients with real or perceived deformities.
History and physical examination
As with all forms of treatment, the first step in evaluating a patient with a scar is obtaining a focused history and performing a physical examination (Box 16.1). The etiology of the scar must be determined as well as relevant influencing factors such as prior dissatisfactory surgery, violent crime, or infection. The treating physician must be careful to empathize with the patient without laying or refuting blame on prior treating physicians. Often this can be accomplished by focusing on the problem and appropriate next steps instead of past mistakes. Little can be gained from implicating other physicians who may earnestly seek your expertise with managing difficult scars.
Assessing scars
Clinical evaluation of a scar is necessary in determining the best course of treatment and, once initiated, the effectiveness of therapy. Multiple objective and subjective assessment tools have been devised to characterize scars. The ideal scale must demonstrate validity, interobserver reliability, and clinical applicability. While there is yet no universal consensus on scar grading, the most frequently used measure is the Burn Scar Index, also known as the Vancouver Scar Scale (VSS) (Table 16.1).10 Originally published in 1990, the VSS was designed to assess changes in burn scars with maturity and in response to treatment. Scars are assessed for pigmentation, vascularity, pliability, and height. Scores are then assigned across these four variables based on the degree of variance from normal skin. When applied, the scale can be a useful tool in prognosis and treatment evaluation. In 1995, Baryza and Baryza11 found that adding a low-cost instrument could improve interobserver reliability. Their tool combined a ruler, a transparent piece of plastic, and a scoring “cheat sheet” with which to aid in measuring, blanching, and determining the score, respectively.
Table 16.1 The Vancouver Scar Scale
| Pigmentation | |
| 0 | Normal: color that closely resembles the color of the rest of the body |
| 1 | Hypopigmentation |
| 2 | Hyperpigmentation |
| Vascularity | |
| 0 | Normal: color that closely resembles the color of the rest of the body |
| 1 | Pink |
| 2 | Red |
| 3 | Purple |
| Pliability | |
| 0 | Normal |
| 1 | Supple: flexible with minimal resistance |
| 2 | Yielding: giving way to pressure |
| 3 | Firm: inflexible, not easily moved, resistant to manual pressure |
| 4 | Banding: rope-like tissue that blanches with extension of the scar |
| 5 | Contracture: permanent shortening of the scar, producing deformity or distortion |
| Height | |
| 0 | Normal: flat |
| 1 | <2 mm |
| 2 | <5 mm |
| 3 | >5 mm |
(Reproduced from Sullivan T, Smith J, Kermode J, et al. Rating the burn scar. J Burn Care Rehabil. 1990;11:256–260.)
While perhaps the most commonly used assessment tool, the VSS is limited by its historical focus on burn scars. Other evaluation measures, such as the Visual Analog Scale (VAS), the Patient and Observer Scar Assessment Scale (POSAS), the Stony Brook Scar Evaluation Scale (SBSES), and the MCFONTZL classification system have varying levels of validation and adoption.12 The large variety of different scales reflects the relative weakness of each system.
The VAS assesses parameters such as color, contour, and texture to correlate intraobserver as well as photographic and histologic findings.13 The scale can be applied to both burn and surgical scars. Similarly, the POSAS was developed in 2004 for burns and has since been validated for linear scars. This scale has the benefit of incorporating patient opinion and can better assess symptoms such as pain, itchiness, and thickness.14,15 A third scale, the SBSES, was initially developed as a tool for emergency medicine physicians to evaluate wounds at the time of suture removal.16 The SBSES has since been adapted for long-term evaluation of scars and has been used as an outcome measure in Food and Drug Administration-mandated clinical trials.17 Lastly, the MCFONTZL classification system was developed specifically for facial trauma (Table 16.2).18 This system incorporates billing and uses a mnemonic to divide the face into the maxilla, chin, forehead, orbits, nose, temple, zygoma, and lip. These scales have been useful in comparing outcomes from conventional versus minimally invasive surgery, use of wound closure adhesives, and new therapeutic agents for scar treatment.
Table 16.2 MCFONTZL assessment system
| A Area | MCFONTZL aesthetic unit designation |
|---|---|
| S Side | |
| T Thickness | Depth of penetration |
| E Extension | Branching |
| R Relaxed skin tension line conformality | Directionality (relaxed skin tension lines) |
| I Index laceration | Laceration with maximum continuous skin interruption |
| S Soft-tissue defect | |
| K Coding | Current procedural terminology code |
(Reproduced from Lee RH, Gamble WB, Robertson B, et al. The MCFONTZL classification system for soft-tissue injuries to the face. Plast Reconstr Surg. 1999;103:1150–1157.)
A number of instruments have also been used as tools to assess scars objectively. Blood flow has been analyzed by laser Doppler, while depth and color have been studied by ultrasound and spectrometery.19 Skin elasticity meters, commercialized for evaluation of scleroderma, have also been used to evaluate scars.20 These instruments have largely been used in research rather than clinical settings.
Scar biology
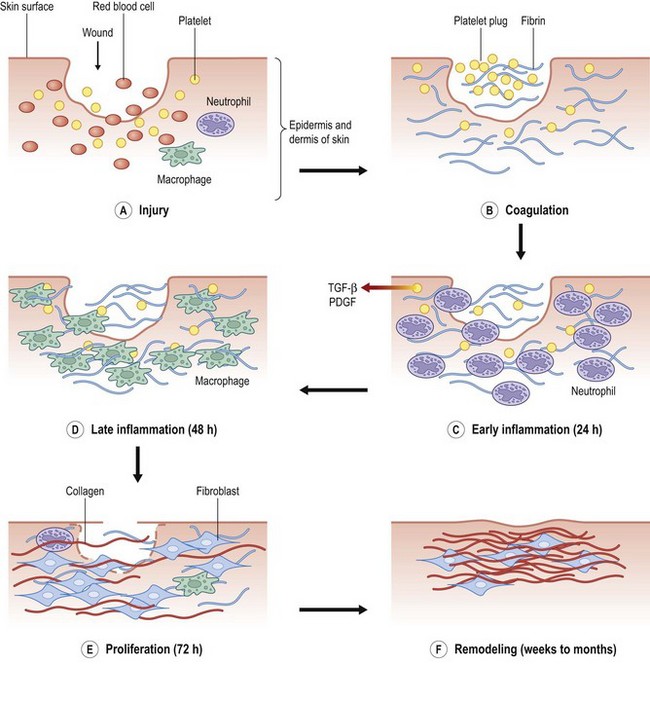
The process of scar formation proceeds temporally from the initial injury through the phases of wound healing into a mature scar, and at times into scar pathology (Fig. 16.1). Wound repair is initiated following injury from trauma, surgery, or disease. The first stage of repair is inflammation, which is characterized by a platelet and white blood cell infiltrate that typically maximizes at 2–3 days. Mediated by the clotting and complement cascades, this initial cellular response is aimed at the establishment of hemostasis and phagocytosis of injured cells. In a noninfected wound, inflammatory cells are then replaced by fibroblasts in the proliferative stage of wound healing. This phase is characterized by synthesis and secretion of the extracellular matrix (ECM).
The ECM is formed by a complex, highly regulated process of synthesis, deposition, and degradation. The initial wound environment is largely composed of fibrin and the glycoaminoglycan hyaluronic acid. As fibroblasts populate the wound, enzymes degrade the matrix and collagen is deposited. Cross-linking and organization of the collagen ultimately create tensile strength across the wound. The process of collagen deposition and degradation is in part determined by the regulation of matrix metalloproteinases (MMPs), which in turn, are inactivated by proteins called tissue inhibitors of metalloproteinases (TIMPs). The balance of MMP-TIMP function is an active area of research in wound healing and scar biology.21
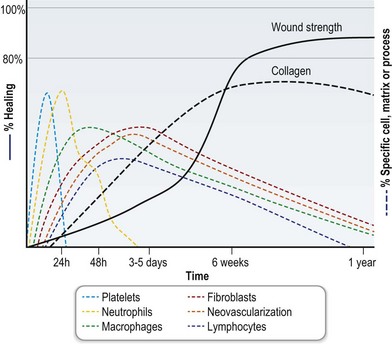
During remodeling, wounds gradually become stronger with time. Wound tensile strength increases rapidly from 1 to 8 weeks postwounding. Thereafter, tensile strength increases at a slower pace and has been documented to increase up to 1 year after wounding in animal studies (Fig. 16.2). Nevertheless, the tensile strength of wounded skin at best only reaches approximately 80% that of unwounded skin. A mature scar, the final result of tissue repair, is brittle, inelastic, and without skin appendages such as hair follicles or sweat glands. The costs of these imperfections are balanced by the benefits of rapid re-establishment of tissue integrity, debridement, and sterilization of contaminated wounds.
Conditions of excessive scarring
In general, both keloid and hypertrophic scar fibroblasts have an upregulation of collagen synthesis, deposition, and accumulation. The underlying regulatory mechanisms leading to excessive repair are not yet known. Profibrotic cytokines such as transforming growth factor-β1 (TGF-β1) have been implicated.22 Evidence also suggests a lack of programmed cell death, or apoptosis, of activated fibroblasts secreting ECM components.23 Hypertrophic scars and keloids are unique to humans and do not naturally occur in other animals for unknown reasons.
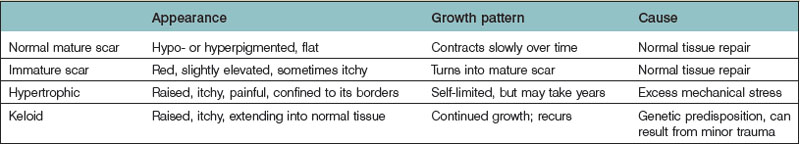
Normotrophic, hypertrophic, and keloid scar vary little histologically.24 Pathological scar types are, therefore, distinguished based on clinical characteristics. Hypertrophic scars continue to thicken and rise instead of flattening and shrinking as mature scars but stay within the original scar boundary; keloid scars continue to grow beyond the boundaries of the initial wound (Table 16.3). Because the time line from immature scar to mature scar to hypertrophic and keloid scar can vary due to a number of factors, diagnosis is not always clear. Important differences, however, do exist and are relevant to treatment.
Hypertrophic scar
Hypertrophic scars are defined as pathologic scars that have not overgrown the original wound boundaries, but are instead raised (Fig. 16.3). Hypertrophic scar is often painful and pruritic, due to a process that may be mediated by higher levels of the neuropeptide substance P.25 These scars usually form secondary to excessive tensile forces across the wound and are most common in wounds across flexion surfaces, the extremities, breasts, sternum, and neck.
Hypertrophic scar is a self-limited process after tissue injury, and usually regresses with time. These scars will eventually fade in color as well as flatten to the surrounding skin level, though the unaided process may take years. No clear histological differences between hypertrophic scar and keloid exist. Early studies found that keloids contained bundles of collagen around focal nodules of proliferation.26 Later studies, however, refuted this distinction. More recently, a study using confocal laser scanning microscopy suggested keloids can be distinguished by the presence of thicker collagen fibers.24 Advances in animal models of hypertrophic scar, including the rabbit ear, red Duroc pig, and mouse will likely be the key to future understanding of hypertrophic scar biology.23,27,28
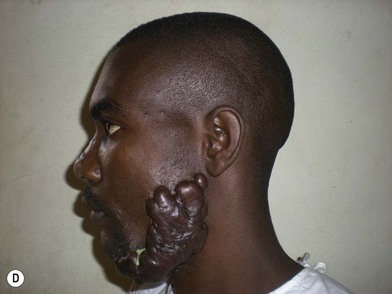
Keloid
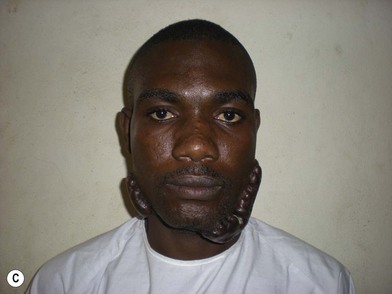
Scars that overgrow the original wound edges are called keloids (Fig. 16.4). This clinical characteristic distinguishes keloids from hypertrophic scars. True keloid scar is not common and occurs predominantly in darkly pigmented individuals, with an incidence of 6–16% in African populations. It has a genetic predisposition with autosomal-dominant features. The keloid scar continues to enlarge past the original wound boundaries and behaves like a benign skin tumor with continued slow growth. Complete excision and primary closure of the defect, however, result in recurrence in the majority of cases.
Keloid formation may be the result of excessive stimulation or an inappropriate response to stimulation. In vitro studies find that keloid keratinocytes and fibroblasts respond differently than normal wound cells to growth factors found at the repair site. TGF-ß treatment, for example, causes a greater degree of collagen gene expression in keloid compared to normal wound fibroblasts.29 In addition, a greater degree of profibrotic growth factor expression occurs in keloids compared to normal wounds.30 These and other studies suggest that keloid formation occurs because of increased expression and activity of proliferative growth factors at the wound site.
Alternatively, a defect affecting the repair process may result in the absence of appropriate “stop” signals for healing. In this proposed mechanism, a lack of stop signals in the wound results in continued and unchecked repair. Studies of apoptotic cell numbers have found similar amounts of apoptotic cells at the advancing wound edge in both normal wound scar and hypertrophic scar. In keloid scar, however, expression of apoptotic genes was decreased.31 The biology of keloids continues to raise important questions about what factors govern normal and pathologic healing.
Prevention
Surgical technique
Notwithstanding the molecular regulation of scar formation, meticulous surgical technique continues to be the cornerstone of successful scar minimization for the plastic surgeon (Box 16.2). To begin, the plastic surgical craft utilizes fine instruments and atraumatic technique to minimize trauma to tissue. Hooks for retraction and avoidance of double grasping with forceps, for instance, help prevent crush injury to delicate tissue.
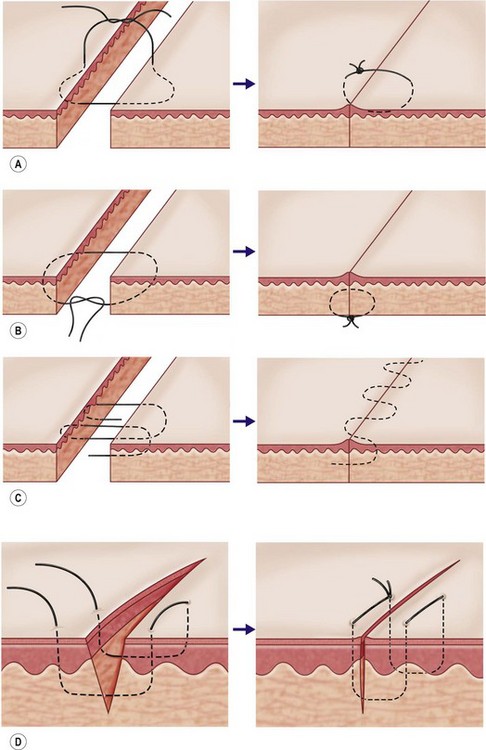
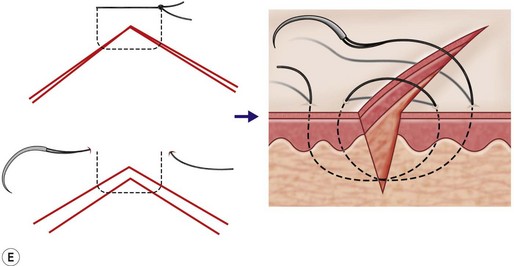
Obtaining a fine pencil line scar also relies on relieving tension on the apposed epidermal edges (Fig. 16.5). Undue tension clearly plays a role in widened and hypertrophic scars. Wound tension causes edge separation and scar widening with time. Wound edges that are defined sharply and aligned without tension heal with the least amount of scar. This is accomplished by approximating tissue with deep buried subdermal stitches, relieving tension of overlying tissue, before final apposition. The Gillies near-far pulley can be used to aid approximation of higher tension tissue. Skin eversion is simply the exaggerated application of the principle of tension-free closure. Horizontal mattress and “flask-shaped” simple sutures achieve adequate eversion; however, care must be taken not to strangulate tissue with overly tight stitches.
To minimize visible scar, elective incisions are least noticeable when placed parallel to the natural lines of skin tension (Langer’s lines) (Fig. 16.6). This placement location has two advantages: the scar is parallel or within a natural skin crease, which camouflages the scar, and the location places the least amount of tension on the wound.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree