Abstract
Although the scalp represents one of the most visually and anatomically homogeneous regions of the head and neck, its unique anatomic characteristics and subtleties, however, can often make reconstructive surgery in this area quite challenging. The distribution of underlying muscle and the compartmentalization of the scalp by the galea aponeurotica, the presence of terminal hairs, and the skin biomechanics are features that must be taken into consideration. These characteristics of the scalp provide both benefits and drawbacks during reconstructive planning. Primary closures, flaps, and grafts can all be utilized to reconstruct the scalp, although their application techniques can be very different when compared to their uses on other parts of the face. The broad, inelastic nature of the galea, encompassing the scalp as a tendonlike sheath under constant tension, lends the scalp its relative immobility. As such, in comparison to facial skin, extensive undermining and longer incisions are often necessary during scalp reconstruction in order to achieve only small degrees of tissue movement. A thorough understanding of these aspects of the scalp is mandatory for attaining the best surgical outcome.
Keywords
surgical scalp defects, scalp closure, scalp flaps, scalp granulation
Although the scalp represents one of the most visually and anatomically homogeneous regions of the head and neck, its unique anatomic characteristics and subtleties, however, can often make reconstructive surgery in this area quite challenging. The distribution of underlying muscle and the compartmentalization of the scalp by the galea aponeurotica, the presence of terminal hairs, and the skin biomechanics are features that must be taken into consideration. These characteristics of the scalp provide both benefits and drawbacks during reconstructive planning. Primary closures, flaps, and grafts can all be utilized to reconstruct the scalp, although their application techniques can be very different when compared to their uses on other parts of the face. The broad, inelastic nature of the galea, encompassing the scalp as a tendonlike sheath under constant tension, lends the scalp its relative immobility. As such, in comparison to facial skin, extensive undermining and longer incisions are often necessary during scalp reconstruction in order to achieve only small degrees of tissue movement. A thorough understanding of these aspects of the scalp is mandatory for attaining the best surgical outcome.
Scalp Surgical Anatomy
The scalp extends from the superior nuchal line posteriorly to the superior border of the frontalis muscle and is delineated by the pinnae bilaterally. The scalp is composed of five layers: skin, subcutaneous connective tissue, galea, subaponeurotic loose areolar tissue, and pericranium. The skin is tethered to the underlying subcutaneous connective tissue and galea by muscle and fibrous bands. Local flaps commonly incorporate the outer three layers of the scalp, and flap undermining is easily performed through the subgaleal space, a relatively avascular plane.
The galea consists of a thick membranous tendon (galea aponeurotica) that completely encases both the frontalis muscle anteriorly and the occipitalis muscle posteriorly. These muscles are joined in the midline by posterior and anterior extensions of the galea. The galea tightly wraps over the skull because of the antagonistic actions of the frontalis and occipitalis muscles. The temporoparietal muscles originate from the superficial temporal fascia and insert into the lateral border of the galea aponeurotica. Whereas the frontalis/galea/occipitalis are at the depth of the muscles of facial expression, the temporoparietalis is at the deeper level of the muscles of mastication. The subgaleal space lies over the pericranium on the crown of the scalp but extends over the temporoparietalis muscle laterally. This is important, as undermining should be performed in the relatively avascular subgaleal plane above the temporoparietalis muscle and under the frontalis and occipitalis muscles. The scalp areas associated with muscle and fascia exhibit greater mobility than the central regions that consist only of dense underlying galea. As such, more distensible flaps arise from the peripheral scalp, where the skin overlies the frontalis, occipitalis, and temporalis muscles ( Fig. 10.1 ).

Blood vessels and sensory nerves traverse the scalp in a centripetal fashion through the subcutaneous connective tissue layer above the galea. The scalp’s abundant arterial supply is derived from the internal carotid system anteriorly (supraorbital and supratrochlear arteries) and from the external carotid system laterally and posteriorly (occipital, postauricular, and superficial temporal arteries). The extensive vascular anastomoses allow a single superficial temporal artery to provide sufficient blood supply to virtually the entire scalp; however, the midline scalp possesses a relative watershed zone where perfusion may be less predictable. The scalp lymphatic filtration system interlaces with medium-sized blood vessels in the subdermal and subcutaneous layers. Since the scalp lacks lymph nodes, there are no barriers to lymph flow. Lymph flows in a centrifugal pattern toward the parotid, occipital, preauricular, and postauricular areas.
The ophthalmic branch of the fifth cranial (trigeminal) nerve provides sensation to the anterior scalp. The occipital nerve, a second cervical nerve derivative, supplies the posterior scalp. The auriculotemporal and maxillary nerves are responsible for sensation to the temple area, while the great auricular nerve supplies the postauricular area. Infiltrating local anesthetic around the scalp’s periphery (through which all the sensory nerves traverse) can produce total scalp anesthesia.
Evaluation of the Scalp Defect
When presented with a scalp defect or a lesion to be excised, the surgeon must evaluate the various reconstructive options that will result in the optimal surgical outcome.
The following questions need to be considered:
What is the depth of the wound? Is the wound through the skin, galea, or pericranium?
Some superficial wounds can appropriately heal by second intention and may even have hair regrowth if the depth of the wound does not extend below the level of the terminal hair bulbs. Most full-thickness wounds will require undermining in the subgaleal plane for tissue movement. Without an intact periosteum, a skin graft will not likely survive unless the underlying bone is burred to induce pinpoint bleeding.
Is the defect surrounded by hair-bearing or glabrous skin?
On a bald scalp, second intention healing or skin grafting may be reasonable options, as the resulting scars will be less conspicuous on hairless skin. If the defect is surrounded by dense terminal hair growth, either primary closure or flap alternatives should be considered in order to avoid focal alopecia.
How much tissue laxity is present?
Scalp laxity can significantly vary by age and location, and from person to person. Scalps in infants, for example, are quite loose and mobile. As one ages, scalp mobility can change dramatically. The crown of the scalp usually is the least mobile area, whereas the peripheral scalp is more distensible. When evaluating for scalp laxity, one can be deceived by the amount of movement obtained by simply squeezing the sides of the defect together. This movement is partly due to the laxity of the dermis, and the actual movement of the surrounding scalp will be dictated by the galea, which is far stiffer and more immobile.
Can adequate anesthesia be obtained with local infiltration and/or nerve blocks for the type of reconstruction planned?
The degree of undermining required for a scalp closure is far greater than that in many other facial regions. These undermining requirements need to be evaluated before a reconstruction under local anesthesia is initiated. Even with adequate local anesthesia, scalp reconstruction can be quite difficult when patients hear and feel the pressure sensation of the undermining conducted through the underlying bone. General anesthesia may be more suitable for some anxious patients.
Basic Reconstruction Concepts
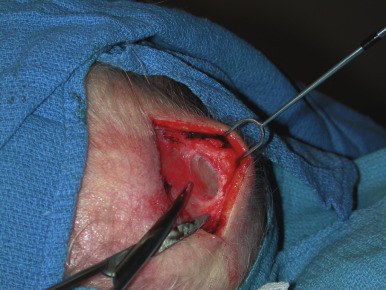
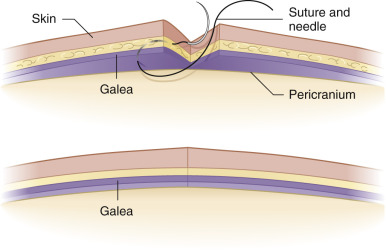
Accessing the subgaleal space is paramount in scalp reconstruction, as this plane is relatively avascular, making it ideal for atraumatic undermining ( Fig. 10.2 ). Blunt dissection of the subgaleal space is all that is needed, and this can be achieved by scissor dissection or by simply using one’s gloved finger. This relative ease of undermining can be very deceptive, however, as the degree of additional movement afforded by wide undermining can be surprisingly small. For the best reconstructive outcome, the galea must be fully reapproximated. It is common for less experienced surgeons, particularly when confronted with very tense wounds, to not fully reapproximate the galea. In these cases, the final reapproximation of the wound’s edges involves stretching the overlying skin. The undesirable tension placed on the epidermal edges results in spread and inverted scars ( Fig. 10.3 ). It is therefore important that the galea is reapproximated by reaching underneath the leading edge of the defect and grabbing a large bite of galea with the suture needle ( Fig. 10.4 ). The strength of a properly realigned galea allows for minimal tension on the overlying skin, which leads to a more aesthetically appropriate scar. If proper wound eversion is not achieved, the final scar will likely be less than ideal.

When confronted with an immobile scalp, the surgeon can enhance the movement of the scalp by performing a galeotomy. The classic galeotomy technique is accomplished by making linear scalpel incisions through the galea from within the essentially avascular subgaleal space. These incisions should be oriented parallel to the wound edge and, if possible, parallel to the course of the underlying vascular supply. The fenestrations expose overlying subcutaneous fat and allow the galea to effectively stretch. Galeotomies can be performed on large flaps without difficulty, as the skin is easily lifted to expose the flap’s undersurface. However, without special equipment such as scalp retractors, galeotomies are more difficult to perform during primary closures. In this setting, angling the scalpel blade to place fenestrations through the galea away from the wound edge is challenging because of limited exposure of the scalp’s undersurface. An electrosurgical apparatus set in the cutting mode can be utilized to reach farther back. The needle can be bent slightly upward to assist with this maneuver ( Fig. 10.5 ).

When performing galeotomies, one must take care not to incise too vigorously, as the deeper vessels in the subcutaneous fat are in close proximity to the galea. The incisions should be made at least 1 cm from the wound edges, or the galea may tear when sutures are used to subsequently reapproximate the surgical defect.
Second Intention Healing
Dermatologic surgeons are accustomed to letting many wounds granulate. Second intention healing is indicated in patients who may not tolerate or desire extensive reconstructive surgery. Allowing the wound to heal by second intention can sometimes be the most appropriate wound management strategy for wounds on alopecic scalps. Often the resultant scars are particularly cosmetically acceptable in these areas of the scalp where hair is absent.
Surprisingly, even deeper scalp wounds allowed to heal by second intention can often fill in to nearly the level of the surrounding skin, and the resulting scars usually look better than alternative split-thickness skin graft or scars from side-to-side or flap repairs. One of the main disadvantages of second intention healing is the prolonged duration of wound healing. These defects often take more than 1 month to completely granulate. If the underlying calvarium is exposed at the base of the wound, the duration of second intention healing can be much longer, but this option remains relatively safe and successful. One must be sure that the patient or a caretaker is able to provide proper wound care.
In older patients with atrophic scalp skin, the healing process can uncommonly arrest after the initial period of granulation. In these instances, the use of delayed split-thickness skin grafts can be helpful in achieving final epithelialization.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








