Scalp Burn Reconstruction
Description
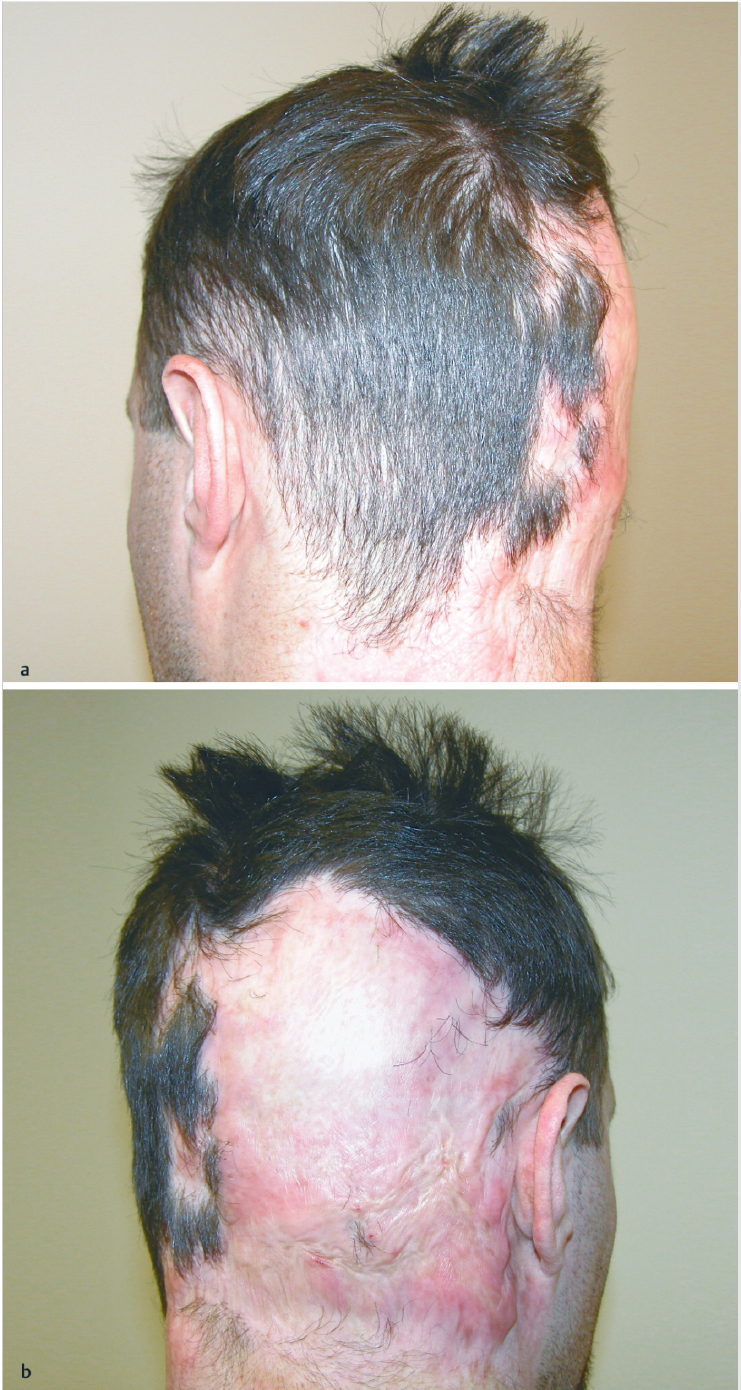
Irregular scarring and alopecia to the right occipital scalp
Extension to the superior neck and retroauricular region.
Defect involves ~ 25% of normal hair-bearing scalp surface.
Work-up
History
Etiology of scar, including mechanism and depth of burns.
Time interval since injury and reconstruction.
Medical comorbidities
Wound- healing problems.
Smoking history.
Bleeding disorders.
Social support network.
Physical examination
Assess size of scar and degree of scalp laxity.
Assess directionality of remaining hair.
Assess for other scars or affected body regions.
Treatment
Establish patient expectations for reconstruction.
Correction of alopecia (bring in new hair-bearing tissue).
Improvement in hairline.
Improvement in facial appearance (excise grafted regions and replace with local tissue, if possible).
Flap coverage
Viable option for smaller defects of the scalp.
Scalp tissue has less mobility than tissue in other parts of the body.
Large flaps should be designed to optimize result and minimize tension.
Common flap options: Rotation, advancement (V-Y), transposition, pinwheel, Orticochea.
Tissue expansion
Defects of up to 50% of the scalp can be reconstructed.
Preferred technique for scalp reconstruction.
Multiple expanders may be used for a single defect. More than one expansion may be performed.
Incisions are designed perpendicular to axis of expansion, can be placed within lesion to allow future excision.
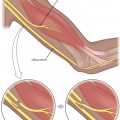
Subgaleal placement.
Internal ports are less convenient but have a lower risk for infection compared with external ports.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree