SCALP RECONSTRUCTION
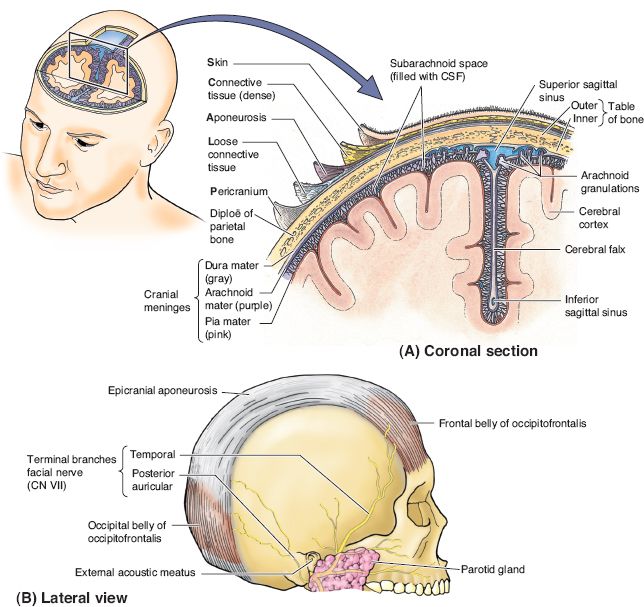
I. ANATOMIC LAYERS OF THE SCALP—ACRONYM SCALP (FIG. 23-1)
A. S: Skin
B. C: Connective tissue
1. Hair follicles, sweat glands, and fat cells
2. Connective tissue fibers between the galea and skin
C. A: Aponeurotic layer or galea aponeurotica: A fibrous tissue layer that is continuous with the frontalis and occipitalis and temporoparietal (TP) fascia
D. L: *Loose areolar tissue: This layer allows the scalp to move on the cranium and is the most common plane of scalp avulsion injuries
E. P: Pericranium/periosteum: A thick collagenous layer with firm attachments to the skull
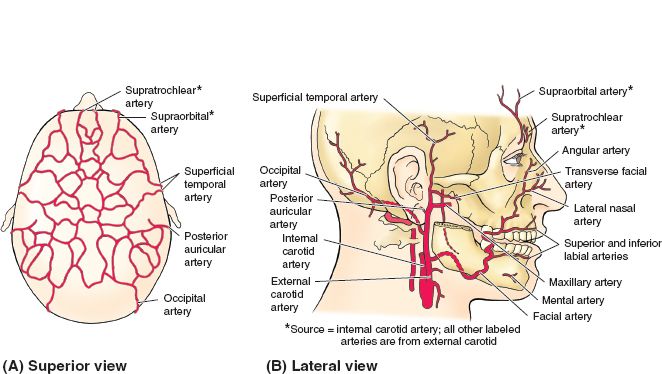
II. SCALP VASCULAR SUPPLY (FIG. 23-2)
A. Internal carotid artery branches
1. Supraorbital artery
2. Supratrochlear artery
B. External carotid artery branches
1. Superficial temporal artery
2. Postauricular artery
3. Occipital artery
4. Extensive interconnections are present between branches and across the mid-line. These anastomoses allow potential replantation of a scalp based on a single artery and vein.
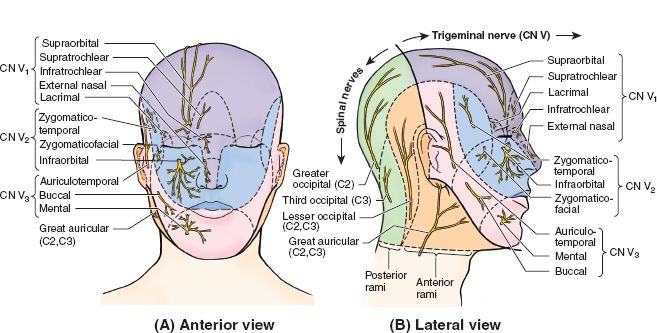
III. SCALP INNERVATION (FIG. 23-3)
A. Motor
1. Frontalis: Frontal branch of CN VII
2. Occipitalis: Posterior auricular branch of CN VII
3. Temporalis: Deep temporal nerve of CN V
B. Sensation
1. Forehead and anterior scalp supplied by supratrochlear and supraorbital nerves (V1)
2. Supraorbital nerve
a. Superficial division: Supplies skin of forehead and anterior hairline
b. Deep division: Innervates frontoparietal scalp
3. Temporal region supplied by zygomaticotemporal nerve (V2) and auriculotemporal nerve (V3)
4. Posterior scalp supplied by greater and lesser occipital nerves (both are spinal nerves from C2/C3)
5. Ear and postauricular area supplied by great auricular nerve (cervical plexus from C2/C3)
IV. SCALP RECONSTRUCTIVE LADDER
A. Primary closure is an excellent option for defects less than 3 cm in diameter
1. Facilitated by wide undermining in the avascular subgaleal plane
______________
*Denotes common in-service examination topics
Figure 23-1. Anatomic layers of the forehead and scalp. (From Moore KL, Dalley AF, Agur AM, eds. Clinically Oriented Anatomy. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
Figure 23-2. Arterial supply to the scalp and face. (From Moore KL, Dalley AF, Agur AM, eds. Clinically Oriented Anatomy. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
Figure 23-3. Sensory innervation to the scalp and face. (From Moore KL, Dalley AF, Agur AM, eds. Clinically Oriented Anatomy. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
2. Scoring the galea allows additional advancement but may decrease the skin’s blood supply
B. Split-thickness skin grafting can provide coverage of a scalp defect but will not reconstruct hair-bearing skin.
1. Split-thickness skin grafting (STSG) can be placed directly on subcutaneous tissue, galea, or pericranium. If calvarial bone is exposed, STSG is contraindicated.
2. If bare calvarium is present, the outer table can be burred and the STSG placed on the diploe.
3. Alternatively, Integra (a bilaminate bovine collagen construct) can be placed and a thin STSG placed at a second operation in 2 to 3 weeks, once neovascularization of the construct has occurred.
4. STSG are technically easy and fast, making them a good option in systemically ill patients for whom cosmesis is of lower importance.
C. Local flaps can provide coverage of defects between 3 cm and up to 30% defects of the scalp.
1. Many local flaps can be designed, including advancement flaps, rotation flaps, and bipedicled flaps.
2. Double-opposing rotation flaps (yin-yang) are also useful. Galeal scoring can increase flap length.
3. Orticochea’s three-flap and four-flap techniques are based on scalp axial blood supply and can cover up to 30% scalp defects.
4. Local flaps provide superior cosmesis as hair-bearing skin is brought into the defect.
5. Flaps should be raised in the subgaleal plane, which keeps the pericranium as a “lifeboat” for STSG should the donor site break down.
6. Similarly, STSG of the secondary defect may be necessary in order to cover the primary defect.
7. Local rotation and advancement flaps often create a dog-ear at the base. Do not excise the dog-ear as flap compromise may result. The majority of these will flatten out over time.
D. Local axial flaps can be used for specific indications
1. Galeal flaps can be based on one or multiple axial vessels.
a. The flap is thin and pliable with minimal donor site morbidity.
b. They are particularly useful for three-dimensional (3D) intracranial defects.
2. TP fascia flaps are based on the superficial temporal vessels and can carry vascularized calvarium. Temporoparietal (TP) fascial flaps are useful for 3D defects or, if bone is included, for periorbital or facial bony defects.
3. Temporalis muscle flaps are based on the deep temporal arteries. Temporalis flaps have limited use as rotation flaps for anterior scalp and periorbital defects.
4. “Crane” flaps are interpolated flaps used to transfer soft tissue to the recipient site. Once vascularization occurs from the recipient site, the flap is raised in a more superficial plane, leaving adequate soft tissue at the recipient site. The flap is then replaced into the original donor site.
E. Tissue expansion is often used in secondary scalp reconstruction and can replace hair-bearing skin with hair-bearing skin.
1. Tissue expansion requires a staged approach with 2 to 3 months between operations.
2. Tissue expansion goal is to generate flaps that are 50% wider and longer than the defect.
3. Multiple rounds of tissue expansion may be required for large defects
4. *Up to 50% defects of the scalp can be reconstructed with tissue expansion before noticing alopecia
5. TEs are placed via incisions at the proposed flap margin, often at the junction of normal scalp and skin graft.
a. Dissection in the subgaleal plane should be just large enough to allow tissue expanders (TE) insertion.
b. Important not to have any sharp folds when placing TE.
c. A separate incision allows placement of a remote filling port over stable bone.
6. Hematoma, infection, and implant exposure are the most common complications of expansion. In children, pressure-related deformation of the cranial vault may occur.
F. Regional muscle transfers are useful for defects in the mastoid, temporal and occipital regions but cannot reach the frontal area or vertex
1. Pectoralis major muscle
2. Pedicled latissimus muscle can also be used for space-filling in orbital exenteration or other defects.
3. Trapezius muscle
G. Free tissue transfer is indicated for extensive wounds or wounds of the vertex and frontal region where regional muscle is not available
1. Free latissimus is the workhorse for scalp coverage due to its broad, flat size, and long vascular pedicle that allows anastomosis in the neck
2. Free omentum, rectus muscle, and parascapular flaps can also be used
3. Inclusion of a skin island may result in a bulky reconstruction. Both muscle and omentum can be skin-grafted.
V. SCALP TRAUMA
A. All wounds should be irrigated and debrided.
B. The scalp has excellent vascularity and may bleed extensively.
C. Closure of scalp wounds with full thickness sutures or staples will provide hemostasis.
D. Layered closure is usually unnecessary. For extensive wounds, closure of the galea may be necessary.
E. Healing by secondary intention is acceptable for small wounds.
F. *Scalp avulsion injuries most commonly occur in the loose areolar plane (e.g., between galea and periosteum). Microvascular anastamosis is the standard of treatment for total and near-total scalp avulsions.
1. The scalp should be treated similarly to a replantable digit in the field: Wrap in moist gauze, place in a plastic bag, and store on an ice slurry.
2. The entire scalp can often be replanted on one artery and vein. The superficial temporal system is preferred.
3. The ideal recipient vessels are contralateral to the zone of injury. Vein grafts are almost always necessary.
4. Contraindications to replantation include ischemia time >30 hours, failure to identify a suitable vascular pedicle, and medical condition precluding prolonged operation and potential blood loss
CALVARIAL RECONSTRUCTION
I. ANATOMIC LAYERS OF THE CRANIUM
A. The cranium is composed of hard (cortical) external and internal tables that enclose the cancellous diploe layer.
B. Periosteum covers the superficial surface of the external table and the deep surface of the internal table.
C. Average bony vault thickness is 7 mm.
D. Temporal bone is thinnest. Occipital bone is thickest.
II. PRINCIPLES OF CALVARIAL RECONSTRUCTION
A. The goals are similar to all reconstructive efforts, namely, restoration of form and function. Specifically, this includes restoration of aesthetic contour and protection of the brain.
B. The frontal region is most important aesthetically because it is not covered with hair-bearing skin. Additionally, frontal bone contributes to the superior portion of the orbit.
C. Thick temporalis muscle can camouflage contour defects in the temporal region. Defects of up to 10 cm2 may not require reconstruction.
D. The parietal and occipital regions require repair for protection of underlying structures; aesthetics in these areas are less of an issue.
III. OPERATIVE PLANNING AND TIMING
A. Physical examination allows identification of aesthetic defects.
B. Preinjury photographs are helpful when available.
C. 3D CT allows visualization of all bony defects.
D. A patient’s 2D CT can be used to produce a lifesize anatomic model; the model assists in the planning process.
E. For defects that involve the frontal or ethmoid sinus, delay of reconstruction of 1 year is preferable to minimize infection risk.
IV. ALLOPLASTIC CRANIOPLASTY MATERIALS
A. *Methyl methacrylate is formed by mixing a powdered polymer and liquid monomer. The substance hardens in an exothermic reaction over 6 to 8 minutes and requires constant irrigation to avoid burning the dura.
1. Advantages: The technique is rapid and technically less demanding than bone cranioplasty. The substance’s contour is stable and can be finely molded with a burr. Methyl methacrylate is radiolucent. No donor site. Relatively inexpensive.
2. Disadvantages: Methyl methacrylate is encapsulated, not incorporated, placing patients at a higher infection risk. The exothermic reaction can burn the dura unless constantly irrigated.
B. Custom titanium or other alloplastic implants can be created by several companies based on a CT scan.
1. Advantages: Can be contoured to match patient’s individual features. Minimum surgical time as the implant is prefabricated. No risk of dura burns. No donor site.
2. Disadvantages: Will not be incorporated and is prone to infection. Radiopaque and will cause scatter on imaging. Expensive.
C. Porous polyethylene (MEDPOR) and hydroxyapatite are less commonly used to reconstruct calvarial defects. Porous polyethylene is particularly useful for contour defects.
V. AUTOGENOUS CRANIOPLASTY MATERIALS
A. Bone is considered to be the ideal cranioplasty material by many surgeons.
1. Advantages include the potential for revascularization. Once revascularized, infection risk is minimal. No additional expense.
2. Disadvantages include need for a second donor site, although the donor site is in the operative field if cranial bone grafts are used. Graft harvest has a low but real risk of dural injury, CSF leak, and meningitis in experienced hands. Bone graft may reabsorb and remodel over time.
B. Split rib grafts
1. Provide long, stable pieces of bone to bridge gaps.
2. Can be contoured with a Tessier bone bender to fit specific defects.
3. Donor site morbidity is minimal and some bones may regenerate if periosteum is left intact.
C. Calvarial bone graft
1. Best harvested from the thick parietal region.
2. The outer table can be separated from the inner table at the diploe layer using a side biting burr and osteotome.
3. Alternatively, a craniotomy can be performed and the bone flap split with a saw. Both flaps are then replaced.
4. The sagittal sinus runs in the midline. This site should be avoided for bone graft harvest.
5. Bone dust, obtained by diffuse burring of calvarium, can be applied directly to dura or used as a final onlay for contouring.
VI. SOFT TISSUE IN CRANIOPLASTY
A. Some clinical circumstances require obliteration and infection control without cranial vault reconstruction.
B. Microvascular free tissue transfer may be required to provide soft-tissue bulk. This technique is useful when there is a history of infection, extensive dead space, or communication between the intracranial cavity and sinuses. Options include rectus muscle, latissimus muscle, or omentum.
PEARLS
1. The avascular loose areolar plane (subgaleal and supraperiosteal) is commonly dissected in scalp reconstruction. This plane is also where scalp avulsion injuries occur.
2. In a noninfected and nonurgent setting, tissue expansion is the ultimate method to replace 50% of the scalp with hair-bearing tissue.
3. Calvarial reconstruction requires careful preoperative planning, often with a 3D CT and medical modeling. Custom implant creation requires several weeks of advance notice.
4. Bone grafts (split rib or calvarial) are the preferred method for calvarium reconstruction when clinically appropriate
QUESTIONS YOU WILL BE ASKED
1. How much of the scalp can be reconstructed with tissue expansion before noticing alopecia?
50%.
2. What are the advantages of using autogenous bone over alloplastic material for calvarial reconstruction?
Less infection and extrusion.
3. At what level is the scalp commonly avulsed?
Between the galea and periosteum.
4. What technique can be performed intraoperatively to improve rotation/advancement of scalp flaps?
Scoring of the galea.
THINGS TO DRAW
Name/draw the layers of the scalp.
Recommended Readings
Chao AH, Yu P, Skoracki RJ, Demonte F, Hanasono MM. Microsurgical reconstruction of composite scalp and calvarial defects in patients with cancer: a 10-year experience. Head Neck. 2012;34(12):1759–1764. PMID: 22331614.
Lin SJ, Hanasono MM, Skoracki RJ. Scalp and calvarial reconstruction. Semin Plast Surg. 2008;22(4):281–293. PMID: 20567704.
Mehrara BJ, Disa JJ, Pusic A. Scalp reconstruction. J Surg Oncol. 2006;94(6):504–508. PMID: 17061273.
< div class='tao-gold-member'>