Rosacea: Introduction
|
Rosacea
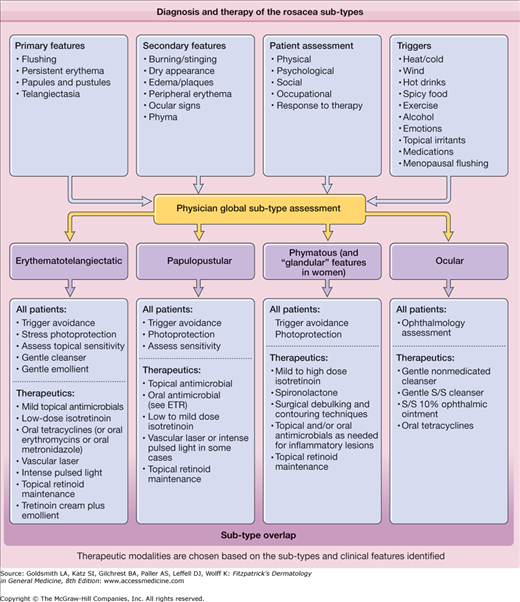
Despite universal recognition, rosacea is clinically varied and of uncertain pathophysiology. Practitioners and the public can easily identify the prototypical red face of rosacea; however, confusion arises when photodamage, perioral dermatitis, postadolescent acne, and topical steroid overuse present in a similar guise. Recent theory has shifted conceptually from staged progression of rosacea signs and symptoms to a new classification that defines four subtypes with variable severity and potential overlap.
Rosacea is characterized by erythema of the central face that has persisted for months or more. The convex areas of the nose, cheeks, chin, and forehead are the characteristic distribution. Primary features of rosacea, which may be observed but are not required for the diagnosis, include flushing, papules, pustules, and telangiectases. Secondary features include facial burning or stinging, edema, plaques, a dry appearance, phyma, peripheral flushing, and ocular manifestations. Erythema in peripheral locations (the scalp, ears, lateral face, neck, and chest) can be observed in rosacea, but is also a common feature of physiologic flushing and chronic sun damage, and therefore must be interpreted carefully.1
The subtypes of rosacea were defined provisionally by the National Rosacea Society (NRS) Expert Committee in 2002 and include erythematotelangiectatic, papulopustular, phymatous, and ocular subtypes.1 These represent the most common groupings of rosacea signs and symptoms. The subtypes coincide with the first rosacea “staging” classification devised by Plewig and Kligman.2 The erythematotelangiectatic subtype is analogous to Plewig–Kligman stage I disease, the papulopustular subtype to Plewig–Kligman stage II, and the phymatous subtype to Plewig–Kligman stage III. In contrast, the NRS classification maintains that progression of rosacea in stages (from one subtype to another) does not occur, but that subtypes may overlap in the same individual. A provisional grading system was also incorporated by the NRS Expert Committee to standardize the clinical assessment of rosacea.3 Rosacea severity assessments must additionally include consideration of the psychological, social, and occupational impacts of this disorder and individual responsiveness to treatment.
Although the prevalence of rosacea is unknown, the vast majority of cases occur in fair-skinned populations and it is common. However, persons of African and Asian descent may also develop rosacea.2,4 The NRS has estimated that rosacea affects 14 million Americans. Rosacea occurs in both men and women, with onset typically after age 30.1,5 However, children, adolescents, and young adults may develop rosacea.6–8
Because of prominent clinical variation among the rosacea subtypes, it has been hypothesized that etiologic and pathophysiologic differences may exist. Such differences may involve facial vascular reactivity, dermal connective tissue structure or composition, matrix composition, pilosebaceous structure, microbial colonization, or a combination of factors that alter the cutaneous response to rosacea trigger factors.9 Rosacea is unmasked or induced by chronic, repeated trigger exposure, in particular by triggers of flushing that may include hot or cold temperature, sunlight, wind, hot drinks, exercise, spicy food, alcohol, emotions, cosmetics, topical irritants, menopausal flushing, and medications that promote flushing.10 Both neural and humoral mechanisms produce flush reactions that are visibly limited to the face. Facial prominence occurs because baseline facial blood flow is increased compared with other body sites,11,12 and the facial cutaneous vasculature is more superficial and comprised of larger and more numerous vessels when compared with other sites.13
New investigations have demonstrated that exacerbation of the innate immune response occurs in rosacea.14,15 Individuals with rosacea express high levels of cathelicidin peptides, and those peptides are processed atypically compared to normal skin. Cathelicidin peptides appear to enable stratum corneum tryptic enzyme (SCTE)-mediated inflammation in the epidermis.14,15
Dermal factors also play a role in rosacea pathogenesis. Matrix degeneration and endothelial damage have been demonstrated histologically in rosacea specimens.16,17 Factors that contribute to matrix degeneration include inherent problems with vessel permeability and/or delayed clearance of inflammatory mediators and waste products. Alternatively, photodamaged connective tissue may alter vascular and lymphatic structure and support within the dermis.18 In either case, chronic and persistent dermal inflammation may occur and ultimately manifest as erythema of the facial convexities in predisposed individuals.19
Sun damage is considered a contributing etiologic factor, and solar elastosis is a common background on which rosacea histologic features are superimposed. However, rosacea prevalence is not increased in outdoor workers, sun damage in nonfacial locations does not progress to a rosacea phenotype, and photoprovocation studies in rosacea patients have not demonstrated increased cutaneous sensitivity to acute ultraviolet exposure.9,17,20,21
It has long been debated whether oral and topical antimicrobial agents for rosacea exert their effects by anti-inflammatory or antimicrobial mechanisms. The concept of microbe-induced, follicle-based inflammation in rosacea is controversial. It is unclear whether commensal organisms such as Propionibacterium acnes and Demodex folliculorum, which reside in hair follicles and sebaceous glands, trigger folliculocentric inflammatory papules in rosacea patients.9 Alternatively, a hypersensitivity reaction may be triggered by these microbes or by mite-associated bacteria such as Bacillus oleronius.22 Compelling arguments in favor of a microbe-induced mechanism for papulopustular rosacea (PPR) include the observation that nonsteroidal anti-inflammatory drugs and corticosteroids do not clear rosacea papules and pustules as effectively as oral tetracyclines. Furthermore, benzoyl peroxide is quite effective for papules and pustules in rosacea patients who tolerate this drug.10 It remains unclear whether clinical improvement of PPR requires a quantitative reduction of P. acnes.
Clinical Features
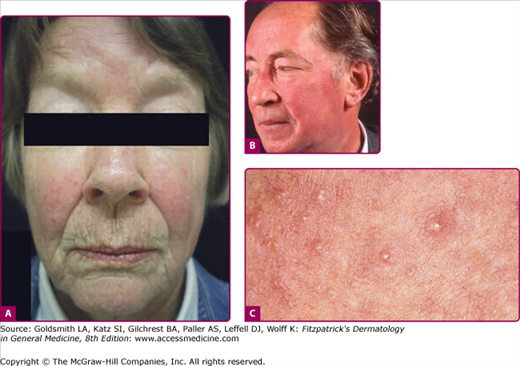
Erythematotelangiectatic rosacea (ETR) is characterized by persistent facial erythema and flushing along with telangiectases, central face edema, burning and stinging, roughness or scaling, or any combination of these signs and symptoms (Fig. 81-1). Mild, moderate, and severe subtypes are recognized. In contrast, PPR manifests as persistent, central-face erythema with papules and pustules that predominate in convex areas (Fig. 81-2).9 Again, mild (see Fig. 81-2A), moderate, and severe forms (see Fig. 81-2B) are distinguished. Burning and stinging of the facial skin may occur in PPR, but occurs less commonly compared with ETR. Flushing is often less severe in PPR compared with ETR. In both subtypes, erythema spares the periorbital areas. Edema can be mild or severe. Severe edema may take on the plaque morphology of solid facial edema.1,23 This occurs most often on the forehead and glabella and it less commonly affects the eyelids and upper cheeks.
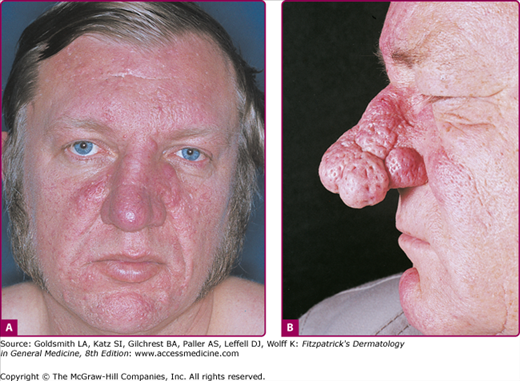
Phymatous rosacea is characterized by patulous follicular orifices, thickened skin, nodularities, and irregular surface contours in convex areas (Fig. 81-3). Here also, mild, moderate, and severe subtypes are distinguished. Phyma most often occurs on the nose (rhinophyma), but may also develop on the chin (gnathophyma), forehead (metophyma), eyelids (blepharophyma), and ears (otophyma).24 Women with rosacea do not develop phyma, perhaps for hormonal reasons, but they can manifest sebaceous or glandular features characterized by thickened skin and large follicular orifices.9
Ocular rosacea may develop before cutaneous symptoms in up to 20% of affected individuals25 (Fig. 81-4). In half of patients, ocular symptoms develop after skin symptoms. In a minority, skin and eye symptoms present simultaneously.26 Ophthalmic rosacea severity does not coincide with cutaneous rosacea severity. Ocular involvement may manifest as blepharitis, conjunctivitis, iritis, scleritis, hypopyon, and keratitis; mild, moderate, and severe subtypes are recognized (see Fig. 81-4).26 Blepharitis is the most common feature, characterized by eyelid margin erythema, scale, and crust, with the variable presence of chalazia and staphylococcal infections due to underlying meibomian gland dysfunction.25 Photophobia, pain, burning, itching, and foreign body sensation may be part of the ocular symptom complex. In severe cases, rosacea keratitis may lead to vision loss.
Granulomatous rosacea is considered the only true rosacea variant.1 Granuloma formation is a histologic feature of the condition; the clinical features of granulomatous rosacea include yellow–brown or red papules or nodules that are monomorphic and located on the cheeks and periorificial facial skin27 (Fig. 81-5). Upon diascopy, these papules reveal apple-jelly-like change in color similar to sarcoidosis or lupus vulgaris. The background facial skin is otherwise normal. Other signs and symptoms of rosacea are not required to make a diagnosis of granulomatous rosacea.
Rosacea is a clinical diagnosis; histology may be helpful when the facial distribution is atypical or when granuloma formation is suspected. In ETR, a sparse, perivascular lymphohistiocytic infiltrate is accompanied by dermal edema and ectatic venules and lymphatics.16 Severe elastosis may be present. Similar features are found in the papulopustular subtype, but the inflammatory infiltrate also surrounds hair follicles and sebaceous glands. Phymatous rosacea is characterized by prominent elastosis, fibrosis, dermal inflammation, sebaceous hyperplasia, and hypertrophy of sebaceous follicles.16,28 Epithelialized tunnels undermine the hyperplastic tissue and are filled with inflammatory debris. D. folliculorum mites may be found in all types of rosacea within the follicular infundibula and sebaceous ducts.28
Systemic diseases that must be differentiated from rosacea include polycythemia vera, connective tissue disorders (lupus erythematosus, dermatomyositis), carcinoid syndrome, mastocytosis, and neurologic causes of flushing. Neurologic causes include brain tumors, spinal cord lesions, orthostatic hypotension, migraine headaches, and Parkinson disease.29 Unilateral auriculotemporal flushing may follow parotid gland injury or surgery.30
Medication-induced flushing has been associated with all vasodilators, calcium channel blockers, nicotinic acid (niacin), morphine, amyl and butyl nitrite, cholinergic drugs, bromocriptine, thyroid releasing hormone, tamoxifen, cyproterone acetate, systemic steroids, and cyclosporine.29,31 The flush associated with nicotinic acid may be blocked with aspirin or indomethacin.32 Disulfiram, chlorpropamide, metronidazole, phentolamine, and cephalosporins induce flushing when they are combined with alcohol.29 Amiodarone has induced rosacea and multiple chalazia.33 Food additives, including sulfites, sodium nitrite, nitrates, and monosodium glutamate, may also cause flushing.29 Dumping syndrome following gastric surgery is characterized by flushing, sweats, tachycardia, and abdominal pain.
Cutaneous conditions that may mimic rosacea include topical steroid-induced acneiform eruption (formerly steroid-induced rosacea), acne vulgaris, perioral dermatitis, inflammatory keratosis pilaris, and chronic photodamage. In particular, acne vulgaris (see Chapter 80) and rosacea may coexist, although rosacea most often begins and reaches its peak incidence in the decades after acne declines. The primary differentiating feature between acne vulgaris and rosacea is the presence of open and closed comedones in acne alone.2
Rosacea fulminans, also known as pyoderma faciale and rosacea conglobata, occurs mainly in women in their 20s.2,34,35 It is characterized by the sudden onset of confluent papules, pustules, nodules, and draining sinuses on the chin, cheeks, and forehead within a background of diffuse facial erythema. Rosacea fulminans has proved controversial in its classification and was not included as a rosacea subtype or variant by the NRS Expert Committee.1,2
Perioral dermatitis (see Chapter 82) differs from rosacea in its facial distribution, signs, symptoms, and patient demographic. It is characterized by perioral, and sometimes periorbital, microvesicles, micropustules, scaling, and peeling. It affects younger women and also occurs in children. Central face erythema and inflammatory papules are not features of perioral dermatitis.9 Therapy includes topical and oral antimicrobials. Perioral dermatitis is exacerbated by topical steroid use.
Steroid-induced acneiform eruption (see Chapter 80) can mimic PPR. With prolonged use of topical steroids on the face, monomorphic inflammatory papules may develop.1 The treatment is discontinuation of the topical corticosteroid and initiation of an oral tetracycline, a topical antimicrobial, a topical calcineurin inhibitor, or a combination of these agents.36,37 This regimen is generally continued for 1 to 3 months, and relapse does not tend to occur as long as topical steroids are not reintroduced.
In chronic photodamage (see Chapter 90), telangiectases and erythema are prominent features. However, unlike rosacea, actinic damage affects the periphery of the face and neck, the upper chest, and the posterior auricular skin. Hyperpigmentation and hypopigmentation are additional feature of sun damage not observed in rosacea. Chin involvement is both mental and submental in rosacea, while in chronic photodamage there is submental sparing.9