I. NASAL ANATOMY (FIG. 30-1)
A. Skin: The thickness of nasal skin is a crucial consideration during preoperative analysis
1. Thickness varies between ethnic populations
2. Thin skin will readily reveal the underlying structural irregularities and is less forgiving to extensive dissection.
3. Thick skin will require more significant cartilage/bone manipulation to achieve the desired aesthetic changes.
4. The skin of the lower third of the nose is almost twice the average thickness of the skin of the upper two-thirds. In addition, the lower skin is much less mobile and contains more sebaceous glands.
5. The external appearance of the nose is a balance between the skin layer and the osseocartilaginous framework.
6. Patients with thicker nasal skin are more prone to postoperative edema and scar formation, which results in a longer recovery period.
7. The unique skin-to-skin relationship at the soft triangle predisposes to notching after incisions are made in this delicate region.
B. Muscle
1. There are four groups of paired nasal muscles that are part of the superficial musculoaponeurotic system (SMAS) of the face
2. The blood vessels and nerves run on the undersurface of the nasal SMAS. Therefore, the proper plane of dissection is within a relatively avascular plane deep to the SMAS layer and just superficial to the periosteum and perichondrium.
3. Elevators shorten the nose and dilate the nostrils: Procerus, levator labii superioris alaeque nasi (opens external valve), and anomalous nasi.
4. Depressors lengthen the nose and dilate the nostrils: The alar portion of the nasalis muscle (dilator naris posterior) and depressor septi (can be hyperactive causing decreased tip projection when smiling).
5. The minor dilator is the dilator nasalis anterior.
6. Compressors lengthen the nose and narrow the nostrils: The transverse portion of the nasalis muscle and compressor narium minor.
C. Blood supply: A rich vascular network is comprised of branches of the ophthalmic, internal maxillary, and facial arteries. Venous drainage accompanies the arterial supply.
1. The dorsal nasal artery (branch of ophthalmic) perforates the orbital septum superior to the medial canthal ligament and courses inferiorly along the nasal sidewall.
2. The facial artery bifurcates into the angular artery and the superior labial artery. The latter supplies the nostril sill and the columella, via the columellar artery.
3. The nasal tip receives blood from the columellar artery, the external nasal branch of the anterior ethmoidal artery, and the lateral nasal artery (branch of angular)
______________
*Denotes common in-service examination topics
Figure 30-1. Frontal (above) and lateral (below) views of the anatomy of the external portions of the nose.
4. *With a transcolumellar incision, the columellar branch is divided and blood supply is largely dependent on the lateral nasal artery, which runs 2 mm superior to the alar groove. Therefore, alar base excision should be performed conservatively in these instances.
D. Innervation: Motor innervation is from the zygomatic and buccal branches of the facial nerve. Sensation to the external nose is through divisions of CN V.
1. The radix, the upper dorsum, and upper nasal side walls are supplied by supratrochlear and infratrochlear branches of the ophthalmic nerve
2. *The external nasal branch of the anterior ethmoid nerve (V1), which emerges between the nasal bones and the upper lateral cartilages (ULCs), supplies sensation to the distal dorsum and the nasal tip.
3. Sensation to the lower half of the nasal sidewall, columella, and ala is supplied by the infraorbital branches of the maxillary nerve.
E. Osseocartilaginous framework
1. Bony vault
a. Comprised of the paired nasal bones and the ascending frontal process of the maxilla.
b. Upper one-third to one-half of the nose
2. ULC
a. The cartilaginous vault (or midvault) is comprised of the ULCs and the cartilaginous septum. This vault is actually one single anatomic entity, which during dorsal reduction is separated into three separate units.
b. At the “keystone” area, the nasal bones broadly overlap the cephalic aspect of the ULCs by about 8 to 10 mm in the midline
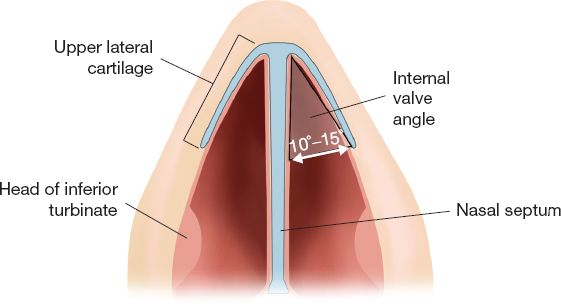
c. At the caudal end of the midvault, *the relationship between the ULC and septum forms the internal nasal valve, which ideally is 10 to 15 degrees (Fig. 30-2)
d. There is a contiguous perichondrial lining from the undersurface of the ULCs to the septum. During component dorsal hump reduction, this lining must first be released from the apex of the cartilaginous vault, creating a “submucosal tunnel” prior to dorsal cartilage resection.
e. Maneuvers that disrupt the smooth dorsal aesthetic lines of the dorsum (e.g., over-resection of the dorsal cartilage or overly narrowed mid-vault after osteotomies) may result in an “inverted-V” deformity
3. Lower lateral cartilage (LLC): Also known as the alar cartilages, the paired LLCs may be viewed as a tripod which supports the nasal tip.
a. Each LLC is subdivided into the medial crus, the middle crus, and the lateral crus. The cephalic edge of the domal segment of the middle crus creates the important “tip-defining point” or pronasale.
Figure 30-2. The internal nasal valve.
b. The junction between the lateral crus of the LLC and the caudal edge of the ULC is known as the “scroll area.” At this location, the ULC edge is rolled deep to the more superficial LLC edge.
c. The lateral crus does not extend to the pyriform aperture. Instead, the patency of the posterior aspect of the ala depends on dense fibrofatty connective tissue and accessory cartilages. These structures contribute to the arch of the vestibule and provide support for the external nasal valve.
4. Septum
a. The cartilaginous component is the quadrangular cartilage.
b. This articulates with the posterior bony septum, consists of the perpendicular plate of the ethmoid bone, the vomer, the nasal crest of the maxilla, and the nasal crest of the palatine bone.
II. GOALS AND PATIENT SELECTION
A. Patients seek rhinoplasty for cosmetic and/or functional reasons.
1. In addition to the patient’s concerns about the nose, the surgeon should also respect nasofacial balance, gender-specific characteristics, and ethnic congruence.
2. In cosmetic patients without nasal obstruction, an important goal is to preserve the nasal airway.
B. Selection of appropriate patients is key to good outcomes
1. Ask the patient specifically what they dislike about their nose and commit to a set of aesthetic/functional goals. Then examine the patient to determine if those goals can be achieved.
2. Be wary of patients with uncorrectable problems, unrealistic expectations, or unhealthy motivating factors. Poor patient satisfaction after rhinoplasty is often due to emotion dissatisfaction and not technical failure.
3. The acronym SIMON represents some red flags: Single, immature, male, overly expectant, and narcissistic.
4. Body dysmorphic disorder (BDD)
a. Somatoform disorder marked by excessive preoccupation with a trivial or perceived defect in physical appearance which causes significant psychological or social impairment
b. Look for compulsive behaviors, intrusive thoughts, camouflaging, and inability to maintain relationships or employment
c. *Affects 7% to 15% of all plastic surgery patients (general population 1% to 2%). Most common sites of patient concern: Skin, hair, and nose.
d. BDD is a contraindication for surgery. Refer the patient to the psychiatrist.
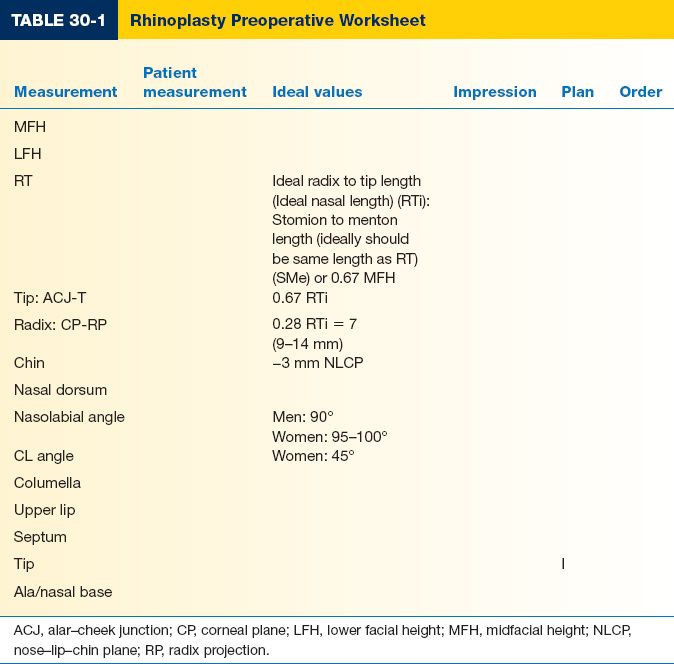
III. PREOPERATIVE ASSESSMENT (TABLE 30-1)
A. Nasal evaluation: A patient’s nasal history must be elicited in detail, as certain medical conditions, trauma, allergies, sinusitis, medications, or previous interventions may affect the final outcome.
1. Nasal obstruction: Alteration in normal aerodynamic flow from increased resistance due to medical or anatomic reasons. Diagnosis is made by history and rhinoscopic examination.
a. *The Cottle maneuver: Lateral cheek traction by the examiner opens a narrow internal valve and results in clinically noticeable improvement in airflow.
b. Inferior turbinate hypertrophy: Compensatory enlargement occurs on the side opposite of septal deviation. Combined with the internal valve, the anterior aspect of the inferior turbinate can account for up to two-thirds of upper airway resistance.
2. Inquire about medications (especially antihypertensives), smoking, drug abuse, previous nasal trauma, and sinus or nasal surgeries.
3. Document allergic disorders and symptoms: Hay fever, asthma, vasomotor rhinitis, sinusitis, nasal stuffiness, dry raw pharynx, postnasal drip, and alterations in taste or smell
4. Previous operative notes may be helpful if the patient has had prior rhinoplasty.
B. Nasal analysis
1. Nasal analysis begins with facial analysis.
a. The ideal face is divided into equal vertical fifths and horizontal thirds.
b. Preexisting asymmetries and the appearance of the patient’s maxilla and mandible should be noted prior to surgery.
b. Look for underlying craniofacial diagnoses such as vertical maxillary excess or malocclusion, which may necessitate intervention prior to rhinoplasty.
c. It is more important for a nose to be in harmony with the rest of the patient’s face than to achieve ideal relationships within the nose itself.
2. Radix: The area where the nose meets the brow is called the radix.
a. The nasion is at the deepest point of the radix and is the apex of the *nasofrontal angle (ideal = 134 degree for women, 130 degree for men).
b. Because the position of the nasion affects the appearance of the rest of the nose, its location is extremely important and setting the nasion is often the first step in planning a rhinoplasty.
c. The vertical level (aka takeoff) of the nasion on profile is critical. A low nasion will give the appearance of a heavier nose, whereas a high nasion will give the appearance of a smaller nose. The nasion should ideally be located at the level of the supratarsal fold or 6 mm above the medial canthus.
d. The projection is measured from a vertical plane tangent to the cornea. Normal projection is 10 to 14 mm.
3. Dorsum: The ideal dorsum on frontal view is outlined by the dorsal aesthetic lines which begin at the medial brow and end at the tip-defining points of the nasal lobule.
a. On lateral view, the dorsal line is drawn from the nasion to the tip-defining point. For women, the ideal line is slightly concave and for men, slightly convex.
b. The nasofacial angle (ideal = 34 degrees for women, 36 degrees for men) is created from a vertical line through the nasion and the dorsal line
c. The width of the nasal bony base should be about 80% of the alar base on frontal view.
d. The distance between the anterior septal angle and the tip-defining point on lateral view determines the presence of a supratip break. This measurement should be 7 mm for thin-skinned patients and 10 mm for thick-skinned patients.
e. *Supratip deformity (aka pollybeak) is defined as a convexity of the supratip area and loss of the supratip break. It can result from inadequate resection of dorsal septum or, paradoxically, over-resection that leads to scarring within the resultant dead space.
4. Six characteristics of the tip should be evaluated—volume, width, definition, rotation, projection, and shape. Interventions to the delicate cartilages of the tip should be judicious because often a change in one characteristic will result in a change in another.
a. Excision of excess cephalic lateral crura (cephalic trim) will reduce tip volume and will also result in some increased tip projection.
b. One important landmark of a refined tip is the tip-defining point, which is created by the domal segment of the middle crus. The most aesthetic LLC configuration is a convex domal segment adjacent to concave lateral crura.
c. Tip rotation is measured by the *nasolabial angle (ideal = 95 to 100 degree for women, 90 to 95 degree for men), which is measured between a line perpendicular to the natural horizontal facial plane and a line drawn through the most anterior and posterior points of the nostril on lateral view. The nasolabial angle is not the same as the columellar– labial angle.
d. The columellar–lobular angle is produced by the junction between the columella and the infratip lobule (ideal = 30 to 45 degrees). Fullness can be due to a prominent caudal septum; deficiency will usually require grafting.
e. Tip projection is measured from a line tangent to the alar–cheek junction (ACJ) and a perpendicular line drawn to the tip-defining point. Tip projection is affected by maxillary projection, columellar length, and abnormalities of the LLCs.
f. The depressor septi nasi muscle can cause downward tip rotation and decreased tip project on animation and may require transposition
5. Ala: The ala should demonstrate a slight outward flare in an inferolateral direction. Note that the width of the base will change with alterations in tip projection.
a. On frontal view, the width of the alar base should be about the same as the intercanthal distance.
b. The relationship between the alar rims and the columella should allow slight nostril show and give a gentle “seagull in flight” appearance.
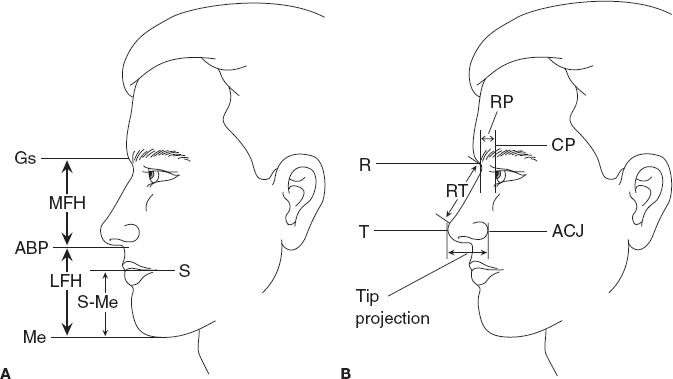
6. Perform Byrd’s analysis with 1:1 photographs and acetate tracing paper to determine objective surgical goals during rhinoplasty (Fig. 30-3). Steps in Byrd’s analysis
a. Check occlusion
b. Measure midfacial height (MFH) on frontal view: Glabella soft tissue to alar base plane (ABP)
c. Measure lower facial height (LFH) on frontal view: ABP to menton soft tissue (Me). Note that MFH should be equal to or slightly less (~3 mm) than LFH.
d. Measure the chin vertical: Stomion (S) to Me. When the mandible is normal, the chin vertical ≈ ideal nasal length.
e. Measure current nasal length on lateral view: Radix (R) to the tip-defining point (T). Note that R should be taken at the level of the supratarsal fold (or 6 mm above the medial canthus) and not the existing nasion, which is frequently abnormal.
Figure 30-3. Key landmarks and reference planes for Byrd’s analysis. A: Landmarks used when measuring facial heights. B: Landmarks used when measuring nasal dimensions. ABP, alar base plane; ACJ, alar–cheek junction; CP, corneal plane; Gs, glabella soft tissue; LFH, lower facial height; Me, menton soft tissue; MFH, midfacial height; RP, radix projection; RT, nasal length; R, radix; S, stomion; T, tip-defining point.
f. Calculate the ideal nasal length (NLi): Remember that NLi = SMe, or NLi = 0.67 × MFH. The maximal amount of nasal length shortening is about 4 mm.
g. Measure current tip projection: A perpendicular line is drawn from ACJ to the tip-defining point (T).
h. Calculate the ideal tip projection (TPi): TPi = 0.67 × NLi. This should also equal alar base width.
i. Measure current radix projection: Corneal plane (CP) to radix (R)
j. Calculate the ideal radix projection: 0.28 × NLi
k. Assess chin projection: Draw the nose–lip–chin plane—mark a point on the nasal dorsum equal to one-half of NLi measured from point R. Draw a line through this point and tangent to the upper lip vermillion. The lower lip and chin should be about 3 mm behind this (in men it should meet this line).
IV. KEY PRINCIPLES OF RHINOPLASTY
A. Detailed descriptions of rhinoplasty techniques can be found within the listed references, but major points are discussed here
B. Anesthesia: An oral RAE endotracheal tube should be used and corneal shields may be placed
1. Topical: Nasal packing with pledgets soaked with either 1% lidocaine with 1:100,000 epinephrine, oxymetazoline, of 4% cocaine or just afrin. These are removed prior to incision.
2. Local: 1% lidocaine with 1:100,000 epinephrine is infiltrated to perform a ring block around the nose. Sites injected include infraorbital foramen (infraorbital artery), lateral nasofacial groove (lateral nasal artery), alar base (angular artery), columella (columellar artery), dorsum (anterior ethmoid artery), tip, and radix (infratrochlear artery). Next the incisions and septum are injected.
C. Approach: The open approach allows for complete exposure, precise diagnosis of defects, and multiple surgical techniques to be performed, but results in a columellar scar, creates more tip edema, and requires suture stabilization of nasal structures. The endonasal (closed) approach offers no external scars, less edema, and rare need for suture fixation, but involves working with restricted exposure, relies heavily on grafts, and is difficult to master.
1. Intercartilaginous: The incision is placed at the junction of the ULC and the LLC. However, due to the scrolling relationship of these two structures, an incision is in reality a cut made into the cephalic lateral crura.
2. Intracartilaginous: The incision is placed purposefully within the substance of the cephalic lateral crura and is determined by the amount of cephalic trim needed
3. Infracartilaginous (aka marginal): The incision is placed just caudal to the caudal edge of the LLC. In open rhinoplasty, this incision is connected with the transcolumellar incision.
4. Transcolumellar: Used for open rhinoplasty. Most use a chevron or stairstep incision at the narrowest aspect of the columella.
5. Transfixion: An incision is made through-and-through the membranous septum, causing downward rotation of the nasal tip. When only one side of the incision is made, this is known as a hemitransfixion incision.
E. Dorsal hump reduction: Submucosal tunnels are created by gently elevating the mucoperichondrium off the septum using a Cottle elevator
1. The ULCs are then separated from the septum and component dorsal hump reduction is performed by trimming these structures incrementally.
2. The dorsum can be reduced before septal harvest to ensure that *at minimum, a 10-mm dorsal and a 10-mm caudal strut (together known as “L-strut”) remain to provide support to the nose.
3. Over-resection of the dorsal strut will predispose to saddle-nose deformity
4. An osteotome or bone rasp is used to reduce the bony dorsum.
5. Excessive reduction will result in an “open roof deformity,” which will impart a flat and wide appearance to the dorsum.
F. Osteotomy
1. Used to close an open roof deformity after dorsal reduction and to narrow a wide bony base.
2. Several techniques are commonly used, but the type of osteotomy needed depends on how much medial movement is required from the lateral nasal wall.
3. Introduce 2-mm osteotome percutaneously at the midportion of bony nasal pyramid at the level of orbital rim and nasofacial junction
4. Must hold osteotome at a plane parallel to the surface of maxilla.
5. To avoid angular artery, sweep down the lateral nasal sidewall in subperiosteal plane.
6. Position osteotome such that one edge is in contact with the bone and strike with the mallet.
7. End point done based on feel and sound.
8. Extend osteotomy in inferior, superior, and supoblique manner at the level of piriform leaving 2 mm gap between each osteotomy.
9. Once osteotomies completed, put pressure from the thumb and index finger only at the superior aspect (not lower or will close off internal valve) to perform greenstick fx of nasal bones.
G. Nasal tip
1. Excess volume is addressed by performing cephalic trim of the lateral crura. *A minimum width of 5 to 7 mm of intact lateral crus should be left to ensure stability.
2. A variety of suturing techniques have been described to effectively increase tip definition, affect tip rotation, influence projection, and reduce tip width. Important among these is the horizontal mattress suture, which can be used to straighten or bend cartilage and provide strength to delicate concave native or donor cartilages.
3. Domal shape can be altered by placing transdomal suture in each medial crura to narrow the dome and increase domal definition.
4. An interdomal stitch will bring the two domes together and narrow the tip.
5. A medial crural suture reduces the divergence between medial footplates.
6. A rotation suture is designed to increase upward tip rotation by advancing the middle crura onto the septum.
7. A projection suture between the medial crura and the caudal septum is performed to provide modest increase in tip projection.
8. If you want to increase nasal tip projection
a. Columellar strut graft
b. Suture techniques (medial crural, interdomal, or transdomal)
c. Tip grafts: Infralobular or onlay
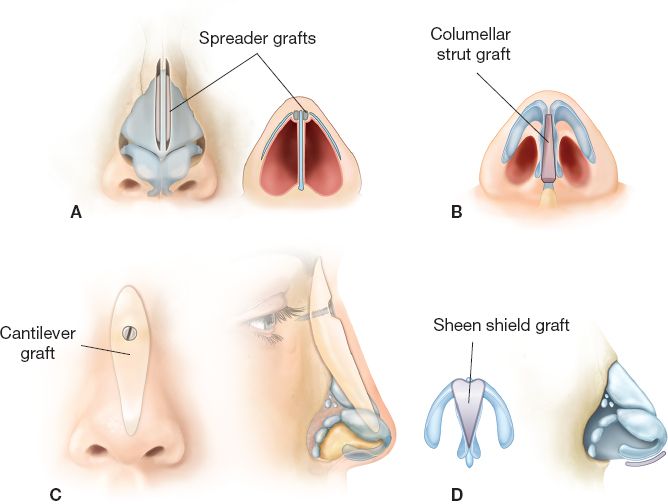
H. Common cartilage grafts (Fig. 30-4)
1. *Spreader grafts open the internal nasal valves, straighten a deviated dorsal septum, and improve dorsal aesthetic lines (such as in an inverted-V deformity). Alternatively, excess ULC that would otherwise be trimmed during dorsal reduction can be turned down and stent the internal valve, serving as spreader flaps.
2. Septal extension grafts extend from the septum and are sewn to the LLCs, acting to increased tip projection.
3. *Alar strut grafts are sutured to the lateral crura and extend over the pyriform aperture to support the external nasal valve.
4. Alar contour grafts are placed along the alar rims for support and to reduce alar notching.
5. Columellar strut grafts help to define columellar shape, strengthen the central limb of the LLC tripod, and maintain tip projection.
6. Tip grafts can provide definition or symmetry to the nasal tip, increase tip projection, and improve a deficient infratip lobule.
7. Radix and dorsal onlay grafts are useful to provide augmentation and symmetry when necessary.
8. Cantilever grafts consisting of septal cartilage, costal cartilage, or bone (e.g., rib, cranial outer table, and iliac bone) may be necessary for nasal dorsum reconstruction.
Figure 30-4. Common cartilage graft techniques. A: Spreader graft; B: columellar strut graft; C: cantilever graft; and D: infratip lobule (Sheen) graft.
I. Ala: Alar base resection (sometimes called Weir excision) can be used to decrease nostril flaring. Care must be taken to avoid injury to the lateral nasal artery during open rhinoplasty. Alternatively, nostril sill excision can be performed.
J. Inferior turbinate: Hypertrophic inferior turbinates can be addressed by submucous resection and outfracture
K. Postoperative care
1. An external nasal splint is worn for 1 week for protection.
2. Internal silastic splints are used for 1 week to compress the septum, provide stability, and prevent development of synechiae between intranasal incisions and septal incisions.
3. Nasal taping is performed for several weeks to reduce swelling.
V. COMPLICATIONS
A. Bleeding: Major epistaxis is rare (<1%) and most bleeding can be treated with head elevation, oxymetazoline nasal spray, careful pressure, and occasionally anterior nasal packing with ribbon gauze and silver nitrate.
1. *Hematoma of the septum should be drained to prevent septal perforations and subsequent saddle-nose deformity. Nasal packing or silastic splints are used after drainage to apply compression.
2. Hematoma under the nasal skin will lead to significant fibrosis and distortion
B. Infection: Acute infection after rhinoplasty is rare (<1%).
1. Some surgeons use prophylactic antibiotics with patients who have risk factors for poor wound healing or if significant grafting was performed.
2. Nasal packing has been implicated in cases of toxic shock syndrome.
C. Airway obstruction: Bruising and edema are a normal consequence of rhinoplasty and the acute swelling subsides within 3 weeks. Patients should expect transient nasal airway obstruction during this time.
1. Intranasal decongestants should not be used for more than 7 days due to rebound nasal congestion after cessation (rhinitis medicamentosa).
2. Persistent obstruction should lead to consideration of anatomic causes, such as collapse of the internal or external valves and synechiae.
D. Asymmetry: Revision surgery and treatment of mild postoperative obstruction should be delayed for at least 1 year to allow for scar maturation and complete resolution of nasal edema.
1. However, within 10 to 14 days, if there is obvious acute deformity (e.g., deviation and displacement of tip graft), it is far better to reoperate than to wait.
2. Excess scar formation may be treated with triamcinolone injections.
VI. SECONDARY RHINOPLASTY
A. Definition: Technically, secondary rhinoplasty is when the primary rhinoplasty (or multiple other rhinoplasties) is performed by another surgeon, whereas a revision surgery is when you reoperate on your own primary case
B. How is secondary rhinoplasty different from primary rhinoplasty?
1. Highly variable nasal anatomy is distorted by scar.
2. The skin envelope is more limiting due to scarring and adhesions.
3. There is often depletion of autogenous cartilage for grafting.
4. Will encounter previous interventions and inherit problems.
5. Patient expectations will be different.
6. Airway problems may have resulted from primary rhinoplasty.
C. Anatomic factors that, when missed during preoperative evaluation for primary rhinoplasty, predispose secondary rhinoplasty.
1. Low radix or low dorsum
2. Narrow midvault
3. Inadequate tip projection
4. Alar cartilage malposition
5. Alar rim weakness
PEARLS
1. Remember to factor in the quality of the nasal skin. Thin skin will easily reveal small irregularities while thick skin requires more significant changes to the underlying nasal structure.
2. If preexisting airway issues are not detected during the preoperative evaluation, a rhinoplasty may result in worsening of this underlying condition
3. The nose must be harmonious with the rest of the face. In a patient with an overprojected nose and chin, reduction rhinoplasty will exaggerate the appearance of the already prominent chin.
4. Evaluation of occlusion is a key component to a complete facial examination. Any abnormalities should be addressed prior to rhinoplasty.
5. An overprojected nose may result in a short and tense upper lip; reduction of nasal projection will in turn lengthen the lip
6. If a patient appears to be preoccupied with an imaginary defect causing significant social distress, think of the possibility of BDD. The surgeon should facilitate psychological consultation and inform that patient that such evaluation is necessary prior to further discussion of surgery.
7. Some patients with a deviated nose will pluck their eyebrows in such a way to camouflage the nasal deformity. This compensatory practice will lead to erroneous preoperative measurements and surgical planning if it is not noticed.
QUESTIONS YOU WILL BE ASKED
1. What could cause nasal deviation?
Deviated septum, deformity of the ULC, asymmetric nasal bone, prior trauma and scarring, and craniofacial abnormality.
2. What is another name for the septal cartilage?
Quadrangular cartilage.
3. What are the bones of the bony septum?
Vomer, perpendicular plate of the ethmoid, crest of the maxillary bone, and crest of the palatine bone.
4. What is the relationship between the ULC and the LLC?
At the scroll area, the caudal end of the ULC is rolled deep to the cephalic end of the LLC.
5. The attending points to the lateral ala and asks: What cartilage supports this part of the nose?
None. The alar component of the LLC sweeps superiorly to meet the ULC; thus, the majority of the substance of the ala is without cartilage. Its structure, thickness, and contour are dependent on dense fibrofatty connective tissue and tiny accessory cartilages.
6. What is the ideal angle for the internal valve?
10 to 15 degrees.
7. What is the ideal nasolabial angle?
95 to 100 degrees for women, 90 to 95 degrees for men.
8. What can we do for this patient whose nasal tip points downward upon smiling?
A hyperactive depressor septi nasi will shorten the upper lip, rotate the nasal tip down, and reduce tip projection upon smiling and can be divided during rhinoplasty.
9. Should I harvest some septal cartilage and then perform dorsal hump reduction?
No. Doral hump reduction should be done before septal harvest to ensure that there is a 10-mm-wide L-strut to support the nose. Otherwise, potential over-resection may lead to saddle-nose deformity.
10. What is a pollybeak deformity?
It is a convexity of the supratip area and loss of the supratip break.
Recommended Readings
Daniel RK. Rhinoplasty: An Atlas of Surgical Techniques. New York: Springer 2002.
Gunter JP, Rohrich RJ, Adams WP Jr. Dallas Rhinoplasty: Nasal Surgery by the Masters. St. Louis, MO: Quality Medical Publishing; 2007.
Oneal RM, Beil RJ. Surgical anatomy of the nose. Clin Plast Surg. 2010;37(2):191-211. PMID: 20206738.
Rohrich RJ, Ahmad J. Rhinoplasty. Plast Reconstr Surg. 2011;128(2):49e-73e. PMID: 21788798.
< div class='tao-gold-member'>