Rheumatoid Arthritis
David T. Netscher
Matthew E. Koepplinger
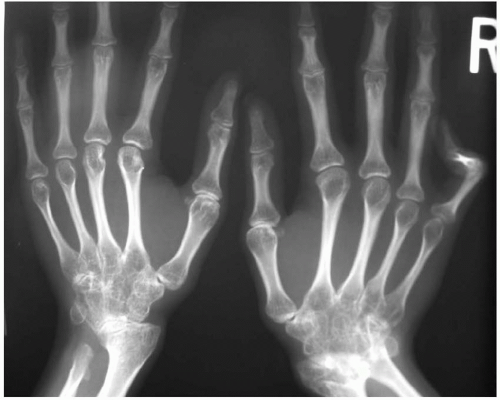
There are multiple overlapping clinical syndromes of inflammatory arthritis, all of which are generically lumped under the diagnosis of “rheumatoid arthritis.” However, these must be distinguished from each other as treatment and prognosis vary. Characteristic clinical features include1,2:
Rheumatoid Arthritis. This is the most common and the most likely to be seen by the hand surgeon. Most cases have an insidious onset with initial symptoms of fatigue, malaise, diffuse musculoskeletal pain, and morning stiffness. Others present with acute onset. Symmetrical involvement is common. For example, if a swan-neck problem occurs in one finger, it is likely to develop in the same finger of the opposite hand. Reasons for this symmetry remain a mystery. Migratory arthritis is uncommon.
By far the most commonly involved joints are the metacarpophalangeal (MP), proximal interphalangeal (PIP), and wrist. Larger joints generally become symptomatic after the small joints. Subcutaneous nodules may occur especially on the extensor aspects of the elbows (Figure 91.1).
Juvenile Rheumatoid Arthritis (JRA) (Figure 91.2). Three types occur–polyarticular, oligoarticular, and systemic illness with fever, rash, and lymphadenopathy (Still’s disease). The polyarthritic type affects primarily the large, rapidly growing joints (knees, wrists, elbows, and ankles). Small joints of the hand and feet are less commonly affected. Temporomandibular joint involvement is common, leading to limitation of bite and micrognathia. The oligoarthritic type most frequently involves isolated knee, ankle, or wrist.
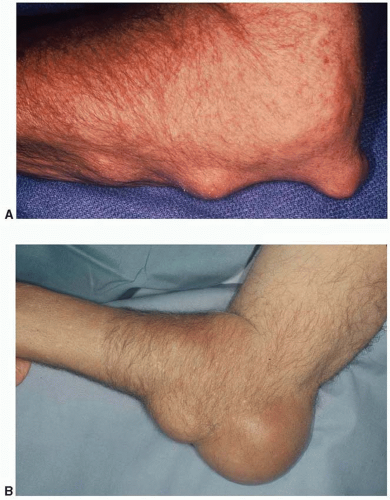
FIGURE 91.1. Rheumatoid arthritis patient with (A) subcutaneous rheumatoid nodules and (B) olecranon bursitis.
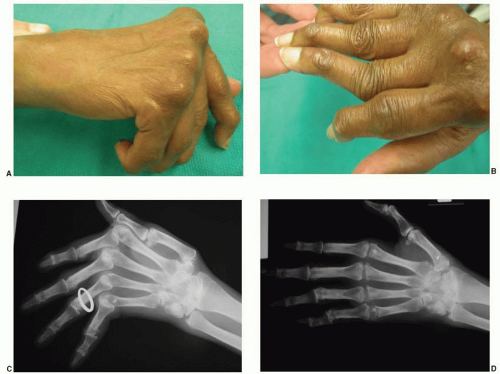
Psoriatic arthritis.1 Distal interphalangeal (DIP) joints are predominantly involved. Occasionally, arthritis mutilans occurs with dissolution of bone and radiographic “pencil in cup” joint changes. This gives the telescoping deformity of the fingers (“opera glass hands”) that can only be treated by arthrodeses to restore stability3,4 (Figure 91.3). Some cases may be clinically indistinguishable from rheumatoid arthritis. Ankylosing spondylitis may occasionally occur. Subcutaneous nodules do not occur. There is frequently a circumscribed shiny, exfoliative rash on the extensor aspects of the extremities and pitting of nails.
Systemic lupus erythematosus (SLE).2 Joint involvement is the most common manifestation although systemic involvement is also frequent. Most common joints involved are PIP, MP, wrist, and knee. Deforming erosive arthritis does not occur, and articular surface preservation is commonly seen on radiographs. However, swanneck deformities and finger ulnar deviation occur and have the clinical appearance of rheumatoid arthritis. Deformities are due to involvement of tendons and ligaments. Vasospastic Raynaud’s phenomenon may occur (Chapter 87). Systemic involvement includes malar rash, sun sensitivity, nail deformities, renal, gastrointestinal, central nervous problems, and lymphadenopathy.
Scleroderma (systemic sclerosis). A small percentage of patients have symmetrical polyarthritis suggestive of rheumatoid arthritis, but are usually seronegative, with nonerosive changes, and without subcutaneous nodules. More commonly there is tight dorsal skin of the fingers and hands with PIP flexion contractures, MP extension contractures, distal bone resorption, with fingertip ulcers. Systemic cardiovascular, pulmonary, renal, and central nervous problems may occur. CREST syndrome (subcutaneous calcinosis, Raynaud’s phenomenon, esophageal hypomotility and strictures, sclerodactyly, telangiectasias) tends to be more indolent and slowly progressive (Figure 91.4).
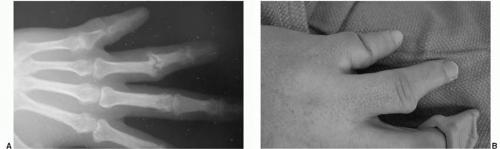
FIGURE 91.3. Arthritis mutilans. A. Radiographic phalangeal bone resorption and (B) “telescoping” or “opera glass” deformity of the digits.
Reiter’s disease. There is an association with arthritis, urethritis, eye problems (conjunctivitis and uveitis), and mouth ulcers. Ligament problems lead to Achilles tendonitis, plantar fasciitis, and back pain.
Enteropathic arthritis. Peripheral arthritis may occur with ulcerative colitis and Crohn’s disease. Ankylosing spondylitis may occur.
Ankylosing spondylitis. Peripheral arthritis does not occur, but psoriatic arthritis, Reiter’s syndrome, and enteropathic arthritis may be present. There is an association with HLA-B27 histocompatibility antigen. Low
back pain and sacroiliitis are the hallmark. Paraspinal ossification occurs.
Mixed connective tissue disease (MCTD). Nearly all patients with MCTD have joint pains and morning stiffness, and 60% develop peripheral arthritis. It is generally not as destructive as rheumatoid arthritis but the appearance of swan-neck deformity and ulnar deviation of fingers is often severe. Unlike SLE, classic joint erosions do occur and some may develop “arthritis mutilans” with severe osteolysis. Systemic pulmonary and gastrointestinal problems occur.
Crystal-induced arthropathy. These include gout (uric acid crystals) and pseudogout (calcium pyrophosphate crystals). The former crystals are needle-like in shape and are negatively birefringent under the polarizing microscope, and the latter are rhomboid in shape and are positively birefringent. Although not pathognomonic for pseudogout, chondrocalcinosis of the triangular fibrocartilage and of the knee meniscus may occur as well as linear calcifications of hyaline cartilage. These conditions may present as acute arthritis or tenosynovitis, but chronic varieties occur with progressive degeneration of multiple joints. The surgeon may be called upon to operate on late-stage tophaceous gout that involves the wrist or fingers. Of importance to the hand surgeon is that these conditions may mimic acute or chronic infections, and even perhaps a tumor (secondary to bone and joint destruction). Gout is often called the “great imitator.”
PATHOGENESIS OF DEFORMITY
Synovitis results in distention of the joint. Ligamentous restraints are destroyed and tendon orientation around affected joints is deranged. This results in changed force vectors. Irregular joint articular surface destruction then leads to further joint imbalance. Tendon ruptures may add to the instability. Finally, secondary zigzag deformities occur at the next distal joint:
Finger deformity
Swan-neck deformity
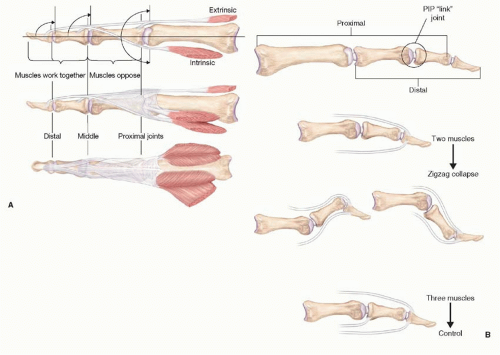
Precise tendon balance exists volar and dorsal to PIP and DIP joints (Figure 91.5). The extensor central slip and flexor digitorum superficialis (FDS) insertion together with the volar plate form opposing dorsal and volar force vectors at the PIP joint. The extensor and flexor digitorum profundus (FDP) insertions likewise form opposing vectors at the DIP joint. Additionally, the intrinsic muscles and extensor hood mechanism are in fine balance with the intrinsics acting volar to the fulcrum of flexion of the MP joint and dorsal to the fulcrum of the PIP and DIP joints.
Swan-neck deformity results from disturbances of the volar/dorsal vector balance or from intrinsic muscle imbalance. Correct diagnosis of the specific cause of swan-neck deformity is important to institute correct treatment. Joint distention and stretch of the volar plate or FDS rupture may lead to PIP joint hyperextension. Chronic mallet deformity can also lead to swanneck problems. Simple placement of an external splint across the DIP joint may be used diagnostically to correct the swan-neck problem in the clinic. If successful, DIP joint fusion may offer a simple solution.
MP joint volar subluxation (a common deformity in rheumatoid arthritis) may also result in swan-neck deformity (Figure 91.6). By clinical examination, one may be able to relocate the MP joint which, in turn, may resolve the swan-neck deformity. In this case, treating the MP joint problem resolves the swan-neck deformity.
Finally, intrinsic tightness is a characteristic problem with rheumatoid arthritis (perhaps secondary to myofibrosis). This can be assessed by the intrinsic tightness test of Bunnell (Figure 91.7). Intrinsic release will resolve the problem (Figure 91.8A). Thus, potential causes of swanneck deformity are5:
Mallet deformity
MP joint volar subluxation
FDS rupture
Intrinsic tightness
Volar plate laxity
Sometimes, there may be a combination of factors. Hence, at the time of MP joint surgery, one may simultaneously perform ulnar intrinsic release.
Corrective surgery for the swan-neck deformity is performed for functional reasons. Due to hyperextension at the PIP joint and dorsal “centralization” of the lateral bands, there is difficulty initiating PIP joint flexion. This will be complicated by an uncomfortable or painful snap as one attempts active PIP flexion, eventually leading to a fixed swan-neck deformity. The degree of PIP joint mobility and radiographic appearance of the affected PIP joint serve as the basis of the Nalebuff classification of swan-neck deformities and their treatment6,7,8:
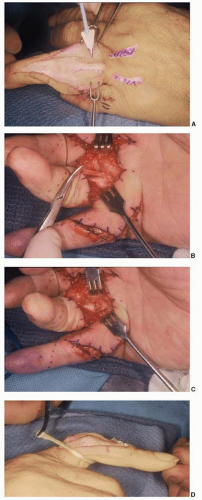
Type I. (Full PIP joint flexibility without intrinsic tightness)–Treatment may be nonoperative, using a Silver ring splint. Operative treatment may involve DIP fusion (if the prime pathology is a mallet finger) or flexor tenodesis at the PIP joint. The latter may be accomplished by using a distally based slip of FDS and suturing it around the leading edge of the A1 pulley or securing it into bone at the base of the proximal phalanx (Figure 91.8B and C). One can recreate the tenodesis of the oblique retinacular ligament of Landsmeer. Littler described releasing the ulnar lateral band proximally and rerouting it volar to the PIP joint axis of rotation (using Cleland’s ligament as a fulcrum). In rheumatoid arthritis, this fulcrum tends to stretch with time. A free tendon graft attached distally to the dorsum of the distal phalanx and routed spirally volar to the PIP joint and anchored to the proximal phalanx is a more reliable technique to correct swan-neck deformity9 (Figure 91.8D).
Type II. (PIP joint flexibility, but with MP joint volar subluxation, and associated intrinsic tightness)–It is insufficient to prevent PIP hyperextension alone. Distal intrinsic release is also required, and possibly also MP joint realignment or even MP implant arthroplasty.
Type III. (Motion of PIP joint limited by the extensor mechanism, but with radiographic preservation of joint surfaces)–Lateral band releases are necessary so that they can slide volar to the condyles. Lateral bands are sharply released from the central slip by two parallel longitudinal incisions. Occasionally, central slip release or lengthening may be required. PIP joint dorsal capsulotomy may also be required.
Type IV. (Stiff PIP joint with intra-articular joint destruction).
–A salvage procedure is necessary–either fusion or arthroplasty, with the former being preferred.
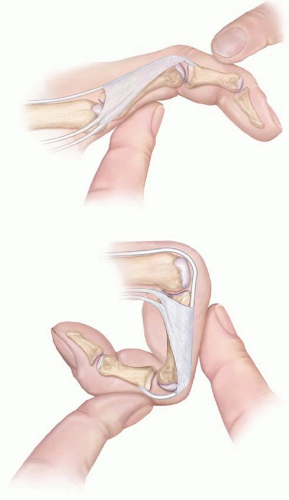
Boutonniere deformity
There is unopposed flexion of the PIP joint and secondary hyperextension at the MP and DIP joints occurs. The central slip and triangular ligament undergo stretch attenuation from PIP joint synovitis. The latter results in lateral band migration volar to the PIP joint axis of rotation, so that they become flexors of the PIP joint and extensors of the DIP joint (Figure 91.9). Nalebuff described a three-stage progressive classification of this deformity8,10:

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree