Graph from Burn Navigator showing current volume (green), Parkland (yellow) and Modified Brooke (bright green) guidelines and projected 24-hour fluid volume
A single-center cohort study showed that computerized decision support can increase how often patients meet UO goals, reduce total fluids given, reduce ventilator days, and may contribute to a reduction in mortality [32]. These results occurred even when 20% or more of the recommendations are rejected by clinicians. The rejection rate may reflect a limitation of the recommendation for the most complicated patients, general skepticism, or proof that the graphical aids and alerts are useful apart from the recommendations. For patient safety, an essential feature of any computerized resuscitation system is the ability for clinicians to override a recommended fluid rate at any time.
In practice, satisfaction with CDS seems to be based on a confidence level obtained with use and familiarity, which results in less need for late night consults between nurses and physicians. It should be noted that when urinary output is not responding to fluid rate increases, or a high 24 h fluid volume is projected, the computer alerts the bedside caregiver to contact the attending physician. CDS technology is a tool to aid, not replace, physician judgment.
Limitations of current CDS: The use of UO is both a strength and a weakness of computerized decision support. UO remains the primary target endpoint today, albeit with notable limitations when it cannot be used. End stage renal disease, hyperglycemia, and high blood alcohol (EtOH) levels make urine output a falsely low or falsely high surrogate of organ perfusion. Those scenarios require users to rely more on hemoglobin, lactate, and hemodynamic indicators for titrating fluids. Gross myoglobinuria and hematuria necessitate a kidney preservation strategy of higher target UO rates to clear high renal concentrations of toxins.
Current CDS approaches face two main limitations: manual data entry and fluid “non-responders,” who are generally defined as patients whose urine output does not increase after increasing infusion rates, or patients whose UO is adequate but only with excessively high infusion rates and a large positive net fluid balance. Patients with a total infused volume over 250 mL/kg, regardless of burn size, are at risk for abdominal compartment syndrome, which is associated with high rates of morbidity and increased mortality [10, 34]. Some patients are non-responders only temporarily, so physicians may tolerate oliguria for 1–3 h during the first 10 h post burn [35]. However, many patients will continue to be non-responders after 10 h post burn. If clinicians continue to increase a crystalloid fluid, such as Lactated Ringer’s, for chronic non-responders, then over-resuscitation and morbidities can result.
Medical providers need to remain vigilant toward intervening. Albumin is a common intervention for many burn centers facing non-responders. Although CDS tools can provide alerts and suggest considering albumin, use of albumin varies greatly by burn center and physician judgment. Albumin therapy typically requires a separate medical prescription order.
Future Technology and Automation: Clinical computerized decision support systems can be advanced in two broad ways. First, by improving approaches to UO confounding situations, as seen with electrical injuries, end stage renal disease or vitamin C use. Adjusting the UO targets higher or lower may be sufficient in some cases; however, incorporation of other endpoint variables and multivariable models may be needed. The second way is by automating UO data collection and fluid titration.
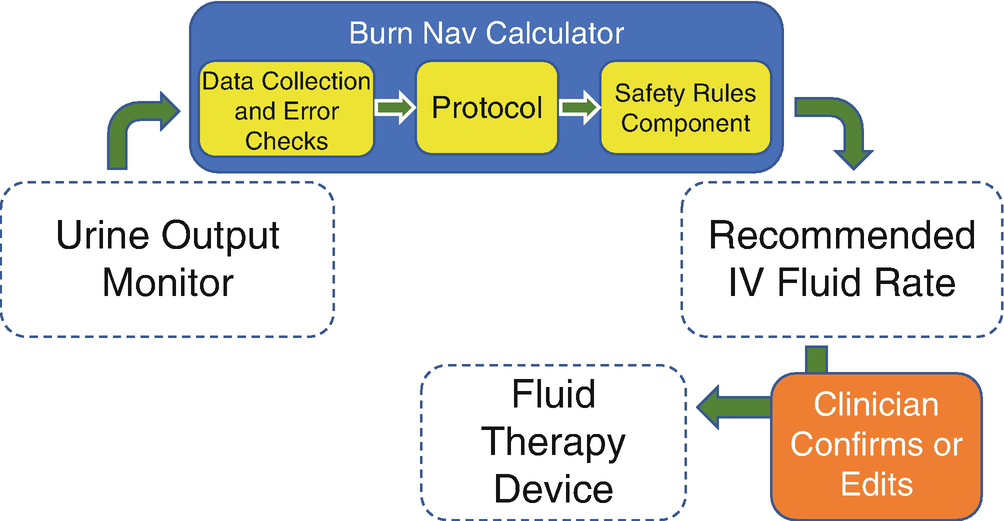
Workflow for hourly fluid updates on open-loop Clinical Decision Support system
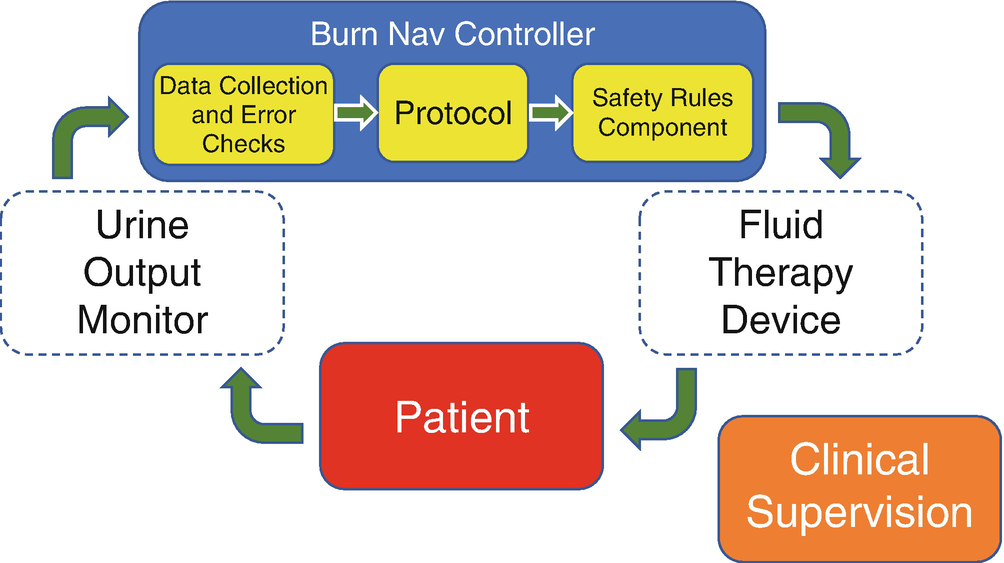
Data and control workflow for closed-loop fluid resuscitation
The response time of UO to fluid and drugs can be on the order of minutes, not an hour. A bolus of fluid delivered over 5 min takes another roughly 5–10 min to result in an increase in UO in the bladder. Fenrich presented sheep data when an automated system adjusted fluids every 10 min based on UO and infusion rates [42]. This frequency of titration would be far too impractical for clinicians to conduct with competing clinical duties, yet promises optimal resuscitation.
In the distant future, a fully automated system may set the UO target based on the patient scenario, run the resuscitation, titrating and weaning fluids, and then announce that the resuscitation phase is over. The U.S. Food and Drug Administration is defining levels of automation and laying the path toward approving physiological closed loop controllers [43].
The connection between a physiologic-based controller and an infusion pump is not a technical challenge, but a regulatory and business challenge with patient safety overtones. Infusion pump companies are extremely reluctant to allow remote rate commands by a third-party device (even an FDA cleared device) since adding such a capability requires a significant cybersecurity defense for the pump’s open port.
A clinician might wonder why the therapeutic device isn’t also the controller; why have two devices instead of one? Infusion pump companies are typically very large companies due to the advanced engineering required to develop and market an infusion pump and the significant safety hurdles that must be maneuvered. On the other hand, companies pioneering closed loop controllers are typically small and heavily reliant on federal development funds. Large, established companies expect to see little improvement in revenues from adding a closed loop feature or controller, particularly for a market as small as burn resuscitation. Despite these business challenges, we suggest that with the pull of the U.S. Department of Defense and with a clear regulatory environment, manufacturers will come to an arrangement on increasing levels of device interaction and automation.
16.1 Conclusion
Burn resuscitation is a complex and ongoing area of research. Challenges include use of surrogate endpoints, the need for physiological vigilance, tedious infusion rate changes, and high variation in patient response to therapy. Emerging strategies, such as use of high dose vitamin C, and evolving strategies, such as use of albumin, offer more options for resuscitative interventions. Novel technologies allow additional visualization and monitoring capabilities and present a vision for automating therapy in the future.
Summary Box
Following severe burn trauma, vascular fluid loss can result in reduced cardiac output, reduced tissue perfusion, and ultimately organ ischemia, failure, and death. Fluid therapy can be effective for maintaining tissue perfusion, but shortcomings with classic methods of burn resuscitation have been linked to fluid overload. In response, alternative approaches to standard of care have been developed, such as use of albumin, high doses of vitamin C and nurse-driven care. A significant recent advancement has been development of electronic urinary output monitors (eUOMs). Another major advancement is Clinical Decision Support (CDS). The Salinas model is a predictive algorithm developed to guide hourly fluid therapy using physiological trends to predict optimal infusion rates. Arcos Burn Navigator, a CDS tool, incorporates the Salinas model to provide decision support and resuscitation displays. It is anticipated that the future of fluid resuscitation will be “open loop” CDS, which involves coordination between a decision support computer, eUOM and IV infusion pumps; and “closed loop” resuscitation, a fully automated system that will customize a urine output target, run the resuscitation, then alert when the resuscitation phase is complete.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








