■ Fine needle aspiration (FNA) with measurement of parathyroid hormone (PTH) can confirm parathyroid tissue in questionable lesions or parathyroid adenomatosis identified by ultrasound.
■ Invasive localization studies such as selective venous sampling (FIG 2) or arteriography should be reserved for when noninvasive studies fail to localize pathology.

SURGICAL MANAGEMENT
Preoperative Planning
■ The imaging must be thoroughly reviewed to plan the operative approach.
■ Prior operative notes are reviewed and operative steps clearly determined prior to reexploration.
■ Positively localized lesions lend themselves to focused reexplorations, whereas more extensive exploration is required for multigland or nonlocalized diseases.
■ Preoperative flexible laryngoscopy is recommended prior to reoperative surgery to document vocal cord function and guide the extent of surgery.
■ Frozen section and intraoperative PTH assays are useful adjuncts to confirm parathyroid identification and biochemical cure.
Positioning
■ The patient is positioned either supine or in the semi-Fowler position. Both arms are tucked and neck extension is achieved with a shoulder roll (FIG 3).

■ Surgical prep must be wide enough to allow access superiorly to angle of mandible and inferiorly to xiphoid in the instance that sternotomy is necessary.
■ General endotracheal anesthesia permits the use of intraoperative nerve monitoring.
TECHNIQUES
CERVICAL REEXPLORATION
Incision and Flap Elevation
■ Skin incisions are placed as indicated by the preoperative localizing studies, preferably in a natural cervical skin crease or the old incision (unless the scar is too low or high). Width of incision is dependent on depth of neck but is large enough to allow access superiorly to the level of the hyoid bone and inferiorly to the anterior mediastinum (FIG 4).

■ Incisions may be placed over the site of pathology for a directed approach if preoperatively localized.
■ Skin and platysma are divided and subplatysmal flaps superficial to the anterior jugular veins are elevated superiorly to the thyroid notch, inferiorly to the sternal notch, and laterally to anterior borders of the sternocleidomastoid muscles (SCM).
Cervical Approach3
■ Surgical approach to the reoperative neck is done via focused exploration or by classic midline, posterolateral, or thyrothymic ligament approaches.
■ Focused explorations for preoperatively localized ectopic glands not accessible via prior cervicotomy should be adjusted to location and surgeon experience with incisions placed according to imaging.
■ Revision cervicotomy is indicated when multigland disease is suspected or when abnormal glands are not localized preoperatively. The previous incision is used and the cervical scar revised prior to opening the midline raphe by vertical separation of strap muscles (see Chapters 45 and 48).
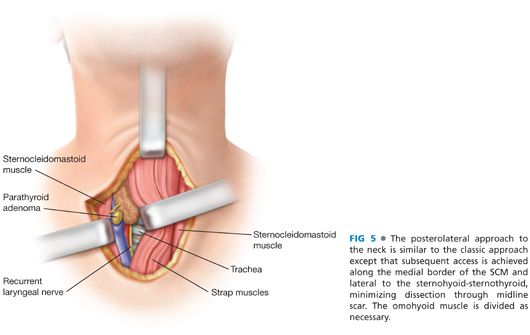
■ The back door or posterolateral approach should be considered when there is extensive scar tissue or when seeking a posteriorly localized gland. The lateral portion of a prior wound is used and entry to the neck is achieved between the lateral border of the straps and anterior portion of the SCM (FIG 5).
■ The front door or thyrothymic ligament approach should be considered when adenomas are localized anteriorly along the inferior thyroid pole or thyrothymic ligament. Infrahyoid muscles may be divided as inferiorly as possible to allow direct access to the thyrothymic ligaments, avoiding dissection between the strap muscles and thyroid capsule.
■ Once deep to the strap muscles, retraction of the thyroid involves elevation of the strap muscles off the gland and medial thyroid rotation. A Kittner, thyroid clamp, or figure-of-eight suture assists thyroid retraction.
■ The recurrent laryngeal nerve (RLN) is then identified and preserved.
Exploration
■ Steps are systematically planned and based on preoperative imaging.
■ If an abnormal gland is localized preoperatively, commence with focused exploration.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








