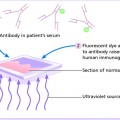
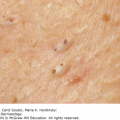
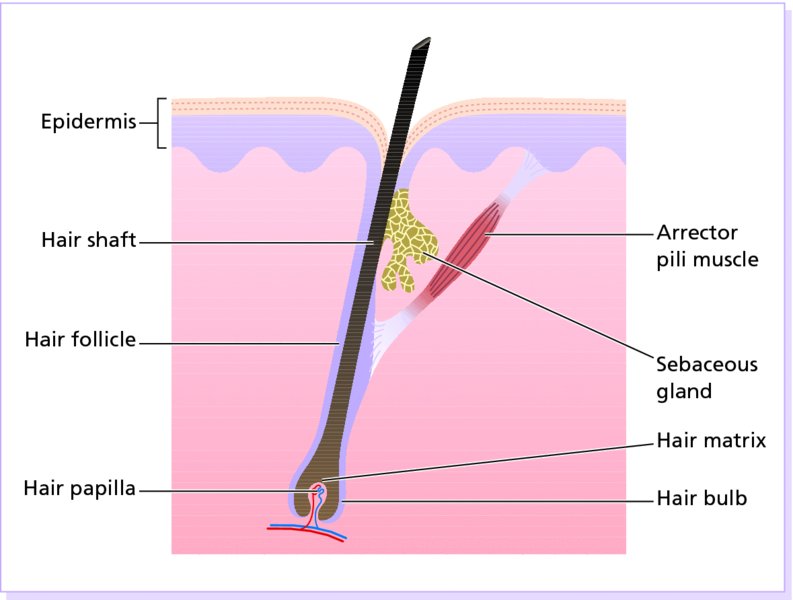
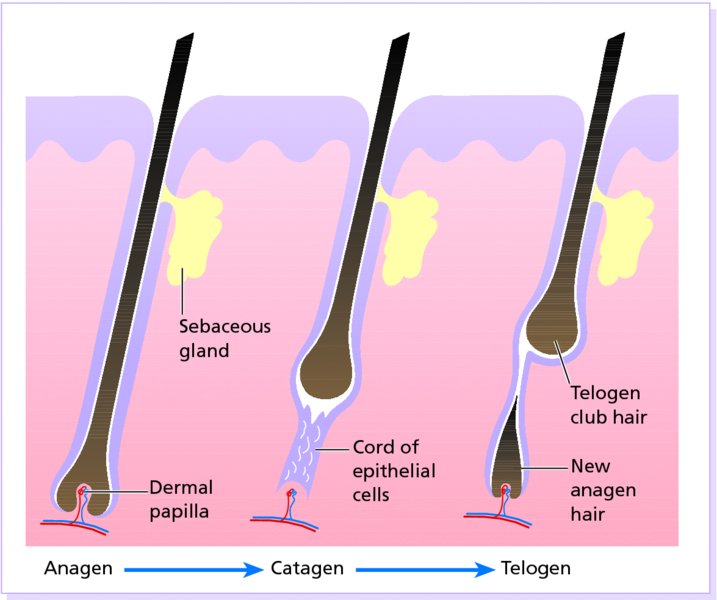
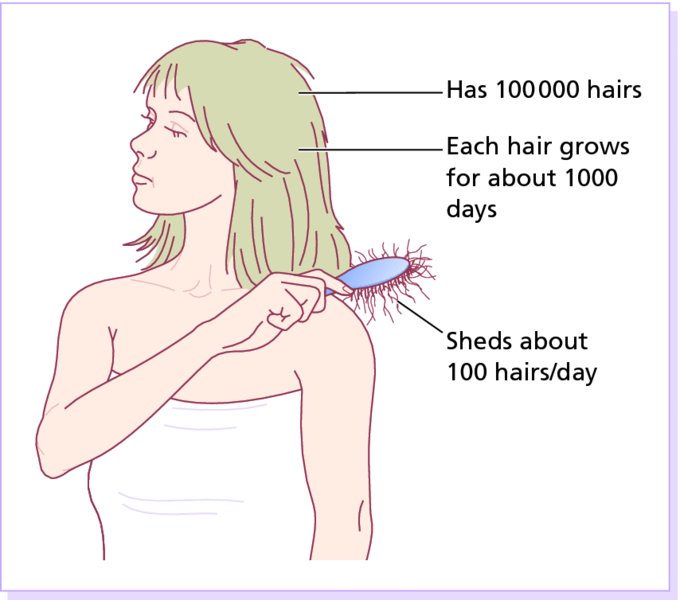
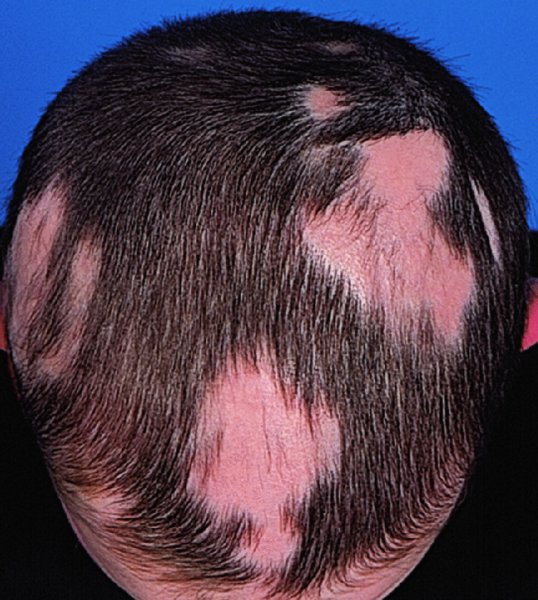
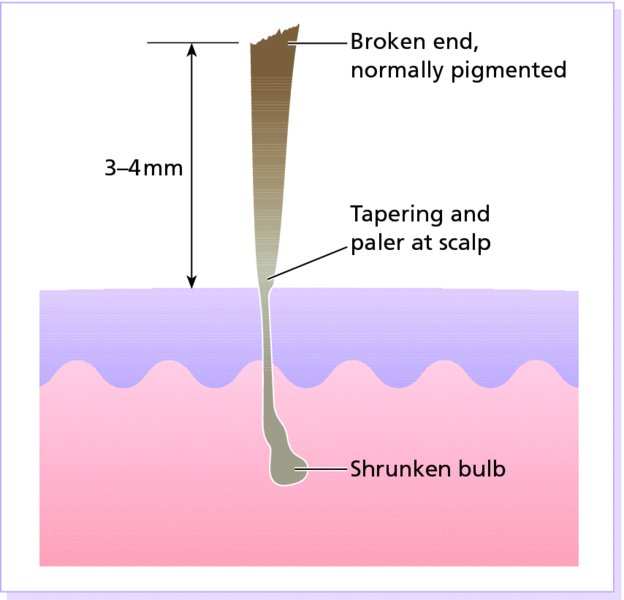
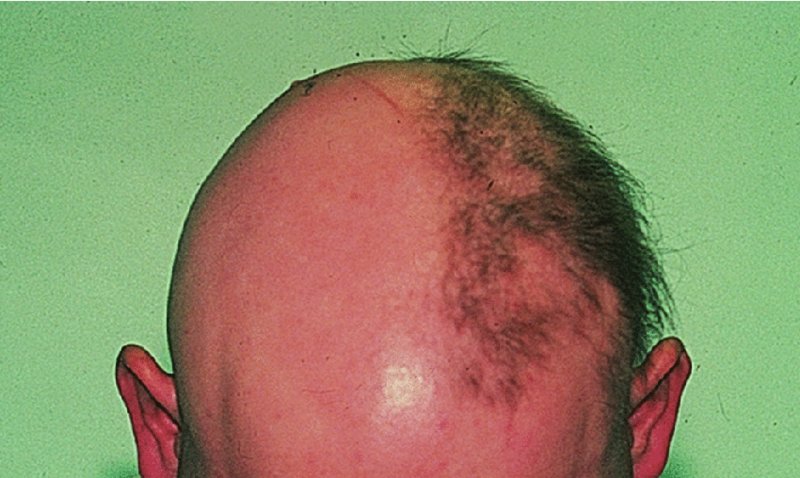
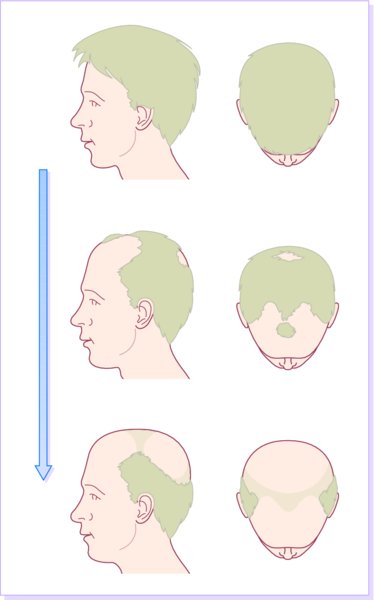
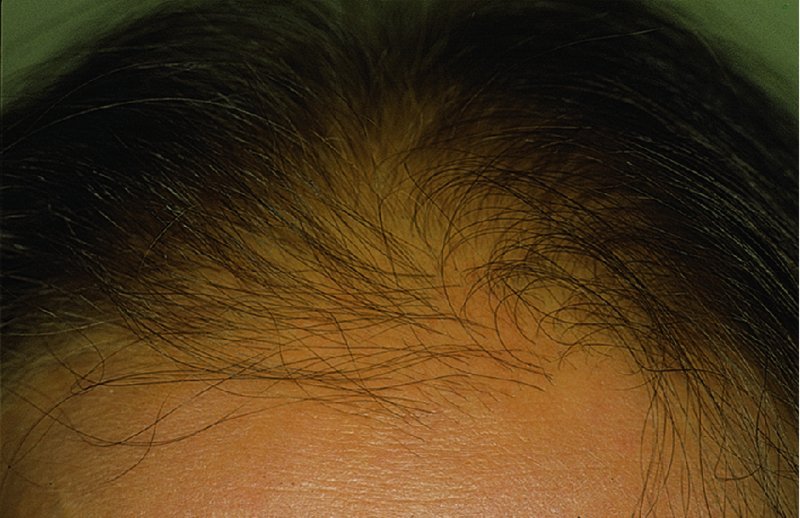
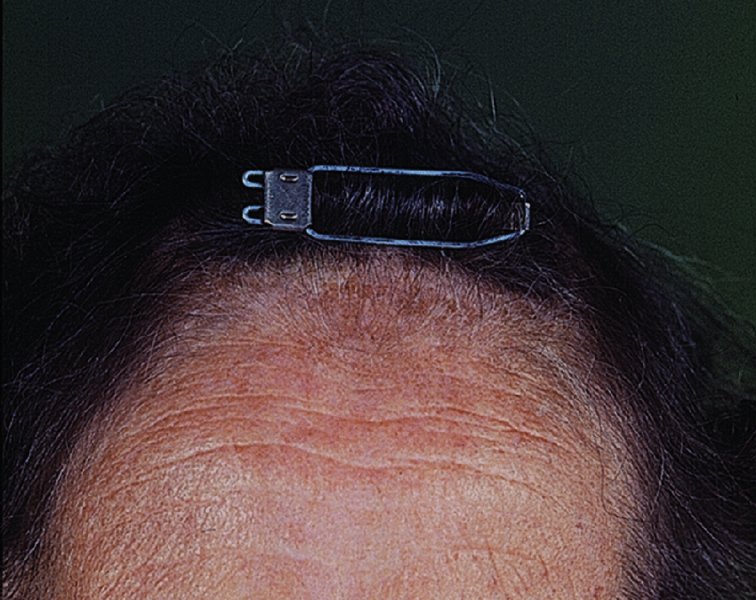
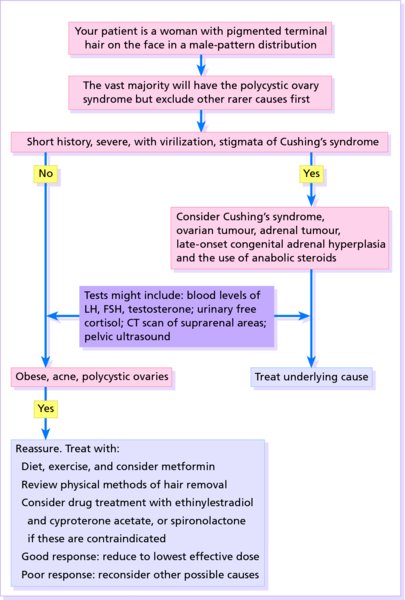
13 Hair is human plumage: we need just the right amount, in the right places. The twin torments of having too much or too little hair can be understood only when seen against the background of the formation and activity of normal hair follicles. Hair follicles form before the ninth week of fetal life when the hair germ, a solid cylinder of cells, grows obliquely down into the dermis. Here it is met by a cluster of mesenchymal cells (the placode) bulging into the lower part of the hair germ to form the hair papilla. Eventually, the papilla contains blood vessels bringing nutrients to the hair matrix. The sebaceous gland is an outgrowth at the side of the hair germ, establishing early the two parts of the pilosebaceous unit. The hair matrix, the germinative part of the follicle, is equivalent to the basal cells of the epidermis. Adjacent to the sebaceous gland is the region of insertion of the arrector pili muscle called the bulge. This area contains hair follicle stem cells which presumably can regenerate the entire hair follicle and sebaceous gland. Damage to this area will cause permanent hair loss. Melanocytes migrate into the matrix and are responsible for the different colours of hair (eumelanin, brown and black; phaeomelanin and trichochromes, red). Grey or white hair is caused by low pigment production, and the filling of the cells in the hair medulla with minute air bubbles that reflect light. The structure of a typical hair follicle is shown in Figure 13.1. Figure 13.1 Anatomy of the hair follicle. Hairs are classified into three main types. Terminal hairs convert to vellus hairs in male-pattern alopecia, and vellus to terminal hairs in hirsutism. The lips, glans penis, labia minora, palms and soles remain free of hair follicles. Each follicle passes, independently of its neighbours, through regular cycles of growth and shedding. There are three phases of follicular activity (Figure 13.2). Figure 13.2 The hair cycle. The duration of each of these stages varies from region to region. On the scalp (Figure 13.3), said to contain an average of 100 000 hairs, anagen lasts for up to 5 years, catagen for about 2 weeks and telogen for about 3 months. As many as 100 hairs may be shed from the normal scalp every day as a normal consequence of cycling. The proportion of hairs in the growing and resting stages can be estimated by looking at plucked hairs (a trichogram). On the scalp, about 85% are normally in anagen and 15% in the telogen phase. The length of hair is determined by the duration of anagen (e.g. the hairs of the eyebrows have shorter cycles than those of the scalp). Figure 13.3 An average scalp. Each hair follicle goes through its growth cycles out of phase with its neighbours, so there is no moulting period. However, if many pass into the resting phase (telogen) at the same time, then a correspondingly large number will be shed 2–3 months later (see Telogen effluvium). There are important racial differences in hair (see Chapter 14). Asians tend to have straight hair, Negroids woolly hair and Europeans wavy hair. These differences are associated with different cross-sectional shapes (round, flattened, etc.). Asians have less facial and body hair than Mediterranean people who also have more hair than northern Europeans. The term means loss of hair and alopecia has many causes and patterns. One convenient division is into localized and diffuse types. It is also important to decide whether or not the hair follicles have been replaced by scar tissue; if they have, regrowth cannot occur. The presence of any disease of the skin itself should also be noted. Some of the most common types are listed in Table 13.1; only a few are dealt with in detail. Table 13.1 Causes of localized alopecia. The lifetime risk of getting alopecia areata is about 2% and, by a coincidence, it is the reason for about 2% of consultations in our skin clinics. An immunological basis is suspected because of an association with autoimmune diseases such as Hashimoto’s thyroiditis, atopy, vitiligo, inflammatory bowel disease and autoimmune polyendocrinopathy syndrome. Histologically, T lymphocytes cluster like a swarm of bees around affected hair bulbs, having been attracted and made to divide by cytokines from the dermal papilla. Alopecia areata is probably inherited as a complex genetic trait, sometimes HLA-DQ3, -DR11 or -DR4 act as susceptibility factors, with an increased occurrence in the first-degree relatives of affected subjects and twin concordance. It affects some 10% of patients with Down’s syndrome – suggesting the involvement of genes on chromosome 21. Environmental factors may trigger alopecia areata in the genetically predisposed. A typical patch is uninflamed, with no scaling, but with empty hair follicles (Figure 13.4). Pathognomonic ‘exclamation-mark’ hairs may be seen around the edge of enlarging areas. They are broken off about 4 mm from the scalp, with the proximal end more narrowed and less pigmented (Figures 13.5 and 13.6). Patches are most common in the scalp and beard but other areas, especially the eyelashes and eyebrows, can be affected too. An uncommon diffuse pattern is recognized, with exclamation-mark hairs scattered widely over a diffusely thinned scalp. Up to 50% of patients show fine pitting or wrinkling of the nails. Figure 13.4 The characteristic uninflamed patches of alopecia areata. Figure 13.5 Exclamation-mark hairs: pathognomonic of alopecia areata. Figure 13.6 An exclamation-mark hair. The outcome is unpredictable. In a first attack, regrowth is usual within a few months. New hairs appear in the centre of patches as fine pale down, and gradually regain their normal thickness and colour, although the new hair may remain white in older patients. Fifty percent of cases resolve spontaneously without treatment in 1 year, and only 10% go on to develop severe chronic disease. Subsequent episodes tend to be more extensive and regrowth is slower. Hair loss in some areas may coexist with regrowth in others. A few of those patients who go on to have chronic disease lose all the hair from their heads (alopecia totalis) or from the whole skin surface (alopecia universalis). Regrowth is tiresomely erratic but the following suggest a poor prognosis. Patches are not scaly, in contrast to ringworm, and are usually uninflamed, in contrast to lupus erythematosus and lichen planus. In the hair-pulling habit of children, and in traction alopecia, broken hairs may be seen but true exclamation-mark hairs are absent. Secondary syphilis can also cause a ‘moth-eaten’ patchy hair loss. A form of scarring alopecia, pseudopelade (see Scarring alopecia), can look similar. None are usually needed. The histology of bald skin shows lymphocytes around and in the hair matrix. Syphilis can be excluded with serological tests if necessary. Organ-specific autoantibody screens provide interesting information but do not affect management. A patient with a first or minor attack can be reassured about the prospects for regrowth. Topical corticosteroid creams of high potency can be prescribed, but it is difficult to tell whether the regrowth is spontaneous or results from the use of creams. The use of systemic steroids should be avoided in most cases, but the intradermal injection of 0.2 mL intralesional triamcinolone acetonide (5–10 mg/mL), raising a small bleb within an affected patch, leads to localized tufts of regrowth (Figure 13.7). While not affecting the overall outcome, this may be useful to re-establish eyebrows or to stimulate hope. It works so reliably that some patients come regularly for reinjections into eyebrows or small areas of the scalp. The downside of this treatment is dermal atrophy evident as depressed areas at the sites of injections. Figure 13.7 Regrowth within a patch of alopecia areata after a triamcinolone injection. Mild irritants, such as 0.1–0.25% dithranol, have been used but with limited success. Ultraviolet radiation or even psoralen with ultraviolet A (PUVA) therapy may help extensive cases, but hair fall often returns when treatment stops. Topical immunotherapy with contact sensitizers (e.g. diphencyprone and squaric acid dibutyl ester) is another promising treatment for patients with extensive disease (Figure 13.8). The efficacy of topical immunosuppressive agents (e.g. tacrolimus) has yet to be proved. Extensive cases should be directed to support groups and given information on wigs and cosmetics. Figure 13.8 A trial of diphencyprone to one side of the scalp caused some regrowth. Although clearly familial, the exact mode of inheritance has not yet been clarified. The idea of a single autosomal dominant gene, with reduced penetrance in women, now seems less likely than a polygenic type of inheritance. Men seem to have a stronger family history of the disorder than females with pattern hair loss. Androgen hormones are clearly implicated in the pathogenesis; in particular, androgenetic alopecia is linked to high levels of dihyrotestosterone (DHT) levels. Testosterone is converted to DHT by the enzyme 5α-reductase. DHT is responsible for temporal scalp hair recession, terminal hair growth in the beard, external ears, nostrils and limbs, and acne, In female-pattern hair loss, there may be an increased sensitivity to circulating androgen, as androgen levels are usually within normal limits. The common pattern in men (Figure 13.9) is the loss of hair first from the temples, and then from the crown. However, in women the hair loss may be much more diffuse (Figure 13.10), particularly over the crown. In bald areas, terminal hairs are replaced by finer vellus ones. Figure 13.9 Variations on male-pattern baldness. Figure 13.10 Androgenetic alopecia beginning in the frontal area. Hair loss is relentless, tending to follow the family pattern with some losing hair quickly and others more slowly. The diffuse pattern seen in women tends to progress slowly. Even minor hair loss may lead to great anxiety and rarely to a monosymptomatic hypochondriasis (p. 336). Bald scalps burn easily in the sun, and may develop multiple actinic keratoses. It has been suggested recently that bald men are more likely to have a heart attack and prostate cancer than those with a full head of hair. The diagnosis is usually obvious in men, but other causes of diffuse hair loss have to be considered in women (Table 13.2). Table 13.2 Causes of diffuse hair loss. None are usually needed. In women virilization may have to be excluded. Scalp surgery, hair transplants and wigs are welcomed by some. Topical application of minoxidil lotion may slow early hair loss and even stimulate new growth of hair but the results are not dramatic (Formulary 1, p. 409). Small and recently acquired patches respond best. When minoxidil treatment stops, the new hairs fall out after about 3 months. Some women with diffuse type of androgenetic alopecia may benefit from suppressing ovarian androgen production with oral contraceptives or an antiandrogen such as spironolactone. Finasteride (Propecia, Formulary 2, p. 417), an inhibitor of human type II 5α-reductase, reduces serum and scalp skin levels of DHT in balding men. At the dosage of 1 mg/day, it may increase hair counts and so lead to a noticeable improvement in both frontal and vertex hair thinning. However, the beneficial effects slowly reverse once treatment has stopped. This treatment is not indicated in women or children. Side effects are rare, but include decreased libido, erectile dysfunction and altered prostate-specific antigen levels. This is dealt with on p. 339. Hair can be pulled out by several procedures intended to beautify, including hot-combing to straighten kinky hair, tight hairstyles such as a pony tail or ‘corn rows’, and using hair rollers too often or too tightly. The changes are usually seen in girls and young women, particularly those whose hair has always tended to be thin anyway. The pattern of hair loss is determined by the cosmetic procedure in use, hair being lost where there is maximal tug. The term marginal alopecia is applied to one common pattern in which hair loss is mainly around the edge of the scalp – at the sides or at the front (Figure 13.11). The bald areas show short broken hairs, folliculitis and, sometimes, scarring. Figure 13.11 Traction alopecia. The rollers she thought would help to disguise her thin hair actually made it worse. Patients are often slow to accept that they are responsible for the hair loss, and notoriously slow to alter their cosmetic practices. Even if they do, regrowth is often disappointingly incomplete. The pattern of hair loss provides the main clue to the diagnosis and, if the possibility of traction alopecia is kept in mind, there is usually no difficulty. The absence of exclamation-mark hairs distinguishes it from alopecia areata, and of scaling from tinea capitis. Patients have to stop doing whatever is causing their hair loss. Rollers that tug can be replaced by those that only heat. Inflammation, often with pustulation, occurs mostly after infection with fungi from animals or soil, and the resultant scarring can be severe. The classic scalp ringworm derived from other human beings causes areas of scaling with broken hairs. The subject is covered in more detail on p. 240. The rough removal of adherent scales can also remove hairs, but regrowth is the rule. Hair follicles can be damaged in many ways. If the follicular openings can no longer be seen with a lens, regrowth of hair cannot be expected. In most cases, there is permanent damage to the follicular stem cell region, or the bulge. Sometimes the cause is obvious: a severe burn, trauma, a carbuncle or an episode of inflammatory scalp ringworm. Discoid lupus erythematosus (p. 129), lichen planus (p. 69) and morphoea (p. 135) can also lead to scarring alopecia. The term pseudopelade is applied to a slowly progressive non-inflamed type of scarring which leads to irregular areas of hair loss without any apparent preceding skin disease. If inflammation is present, a biopsy may help to establish the diagnosis. Some cases of long-standing non-scarring alopecia (such as traction alopecia and alopecia areata) can convert to permanent hair loss after decades of involvement. Central centrifugal cicatricial alopecia (CCCA) is characterized by hair loss with scarring over the vertex of the scalp. The condition is known by many different names in the past, including hot comb alopecia, pseudopelade, follicular degeneration syndrome, and follicular decalvans. While the pathogenesis is multifactorial, hair styling practices including chemical hair relaxer and hot comb use, have been reported in a majority of all female patients presenting with CCCA. However, discontinuation of hair styling practices do not often result in resolution of the disease. Genetically, the curly African hair may be more prone to breakage by these styling methods. CCCA is the most common form of scarring alopecia among black women, often presenting in the third decade of life. Beginning at the vertex of the scalp, the disease gradually spread centrifugally, causing permanent loss of the hair follicles. Pruritus, tenderness and polytrichia (tufted hairs) are common findings. Some patients may note pustules and crusting. This is chronic and progressive. Other causes of scarring alopecia affecting the vertex of the scalp (see Scarring alopecia) can mimic CCCA. Patients with female pattern hair loss have visible follicular openings. Lichen planopilaris shows characteristic perifollicular erythema and follicular keratosis. As permanent hair loss cannot be reversed, treatment is focused on halting the progression of the disease. Topical and intralesional corticosteroids are often used in combination with oral antibiotics such as doxycycline for their anti-inflammatory properties. Patients should be encouraged to stop damaging hair styling practices. Hair is lost evenly from the whole scalp; this may, or may not, be accompanied by a thinning visible to others (Figure 13.12). Some of the most common causes are listed in Table 13.2, but often a simple explanation cannot be found. Figure 13.12 Diffuse hair loss causing much anxiety. Telogen effluvium can be triggered by any severe illness, particularly those with bouts of fever or haemorrhage, by childbirth and by severe dieting. All of these synchronize catagen so that, later on, large numbers of hairs are lost at the same time in the telogen phase. The diffuse hair fall, 2–3 months after the provoking illness, can be mild or severe. In the latter case Beau’s lines (p. 185) may be seen on the nails. Regrowth, not always complete, usually occurs within a few months. This is from other types of diffuse hair loss (Table 13.2). In androgenetic alopecia in females the onset is gradual in mid adulthood, and hairs remain rather firmly anchored to the scalp. In telogen effluvium the onset is abrupt and follows acute illness, an operation or pregnancy by 1–2 months. Hair fall is prominent and lightly pulling on scalp hairs dislodge many. In diffuse alopecia areata, the hair loss is more patchy, and the onset abrupt with waxing and waning. Shedding may be prominent. Exclamation-mark hairs are often present. This condition is unaffected by therapy, but patients can be reassured that their hair loss will be temporary. The causes mentioned in Table 13.2 should be considered. If no cause is obvious, it is worth checking the haemoglobin, erythrocyte sedimentation rate (ESR), antinuclear antibody, serum iron, ferritin, thyroxine and thyroid-stimulating hormone (TSH) levels. Also consider checking the serum free testosterone and dihydroepiandrosterone sulfate levels in women with menstrual irregularities or hirsutism. Despite these, often no cause for diffuse alopecia can be found. More than 300 genetic conditions exist that have hair abnormalities as one component. The hypohidrotic ectodermal dysplasias are a group of rare inherited disorders characterized by sparse hair, scanty sweat glands and poor development of the nails and teeth (Figure 13.13). Heat stroke may follow inadequate sweat production. One type is inherited as an X-linked recessive. The responsible gene for this type (on chromosome Xq12) has recently been shown to encode for a protein (ectodysplasin) involved in the regulation of ectodermal appendage formation. The genes responsible for the dominant or recessive types encode for the ectodysplasin receptor. Figure 13.13 The cone-shaped incisors of hypohidrotic ectodermal dysplasia. In other inherited disorders the hair may be beaded and brittle (monilethrix), flattened and twisted (pili torti), kinky (Menkes’ syndrome caused by mutations in a gene encoding for a copper transporting membrane protein), like bamboo (Netherton’s syndrome, caused by a gene on chromosome 5q32 encoding a serine protease inhibitor), partly broken in many places (trichorrhexis nodosa) or ‘woolly’ or ‘uncombable’. Hirsutism is the growth of terminal hair in a woman (Figure 13.14), which is distributed in the pattern normally seen in a man. Hypertrichosis is an excessive growth of terminal hair that does not follow an androgen-induced pattern (Figure 13.15). Figure 13.14 Moderate hirsutism caused by polycystic ovaries. Figure 13.15 Hypertrichosis in a young man of Mediterranean extraction. Some degree of hirsutism may be a racial or familial trait, and minor facial hirsutism is common after the menopause. In addition, some patients without a family background of hirsutism become hirsute in the absence of any demonstrable hormonal cause (idiopathic hirsutism). Some patients with hirsutism will have one of the disorders shown in Figure 13.16, most commonly the polycystic ovarian syndrome. Figure 13.16 An approach to hirsutism. CT, computed tomography; FSH, follicle stimulating hormone; LH, luteinizing hormone.
Regional Dermatology
The hair
Classification
The hair cycle
Alopecia
Localized alopecia
Non-scarring
Scarring
Alopecia areata
Androgenetic
Scalp ringworm (human)
Hair-pulling habit
Traction alopecia
Burns, radiodermatitis
Aplasia cutis
Kerion
Carbuncle
Cicatricial basal cell carcinoma
Lichen planus
Lupus erythematosus
Necrobiosis
Sarcoidosis
Central centrifugal cicatricial alopecia
Alopecia areata
Cause
Presentation

Course
Differential diagnosis
Investigations
Treatment

Androgenetic alopecia (male and female-pattern hair loss)
Cause
Presentation
Clinical course
Complications
Differential diagnosis
Telogen effluvium
Endocrine
hypopituitarism
hypo- or hyperthyroidism
hypoparathyroidism
high androgenic states
Drug-induced
antimitotic agents (anagen effluvium)
retinoids
anticoagulants
vitamin A excess
oral contraceptives
Androgenetic
Iron deficiency
Severe chronic illness
Malnutrition
Diffuse type of alopecia areata
Investigations
Treatment
Trichotillomania
Traction alopecia
Cause
Presentation
Clinical course
Differential diagnosis
Treatment
Patchy hair loss caused by skin disease
Tinea capitis
Psoriasis
Scarring alopecia
Central centrifugal cicatricial alopecia
Cause
Presentation
Clinical course
Differential diagnosis
Treatment
Diffuse hair loss

Telogen effluvium
Cause
Presentation and course
Differential diagnosis
Treatment
Other causes of diffuse hair loss
Rare genetic causes of hypotrichosis

Hirsutism and hypertrichosis


Hirsutism
Cause
Presentation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree