■ A discussion of patient’s desires and expectations following surgery is essential to avoid dissatisfaction and misunderstandings. In addition, the patient should be informed about possible complications associated with reduction mammoplasty, including changes in nipple sensation, asymmetry, unappealing breast size or shape, scarring, fat necrosis, NAC loss, inability to breastfeed, hematoma, and infection.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ The American Cancer Society recommends screening mammograms starting at age 40 years in patients with average risk of developing breast cancer.5 These patients, and younger patients at increased risk of breast cancer, should therefore undergo a preoperative mammogram prior to reduction mammoplasty. Many plastic surgeons routinely perform a preoperative screening mammogram in all patients undergoing this procedure.
SURGICAL MANAGEMENT
■ There are multiple surgical approaches to reduction mammoplasty; however, all must deal with the following four considerations: (1) reduction in the parenchymal volume of the breast, (2) creation of the NAC pedicle, (3) reduction of expendable skin followed by redraping, and (4) repositioning of the NAC.3 This chapter will describe the most commonly practiced Wise pattern (inverted T) technique, which reduces the medial, lateral, and superior breast parenchymal volume and maintains blood supply to the NAC by an inferior pedicle. Other techniques include the superior medial breast reduction,3 short scar periareolar inferior pedicle reduction (SPAIR),1 and the liposuction breast reduction,6 among others.
■ Advantages to the Wise pattern technique include its reproducibility, popularity, and applicability to a wide range of breast shapes and sizes, whereas disadvantages include longer scars and a tendency toward developing breast ptosis over the long term.
Preoperative Planning
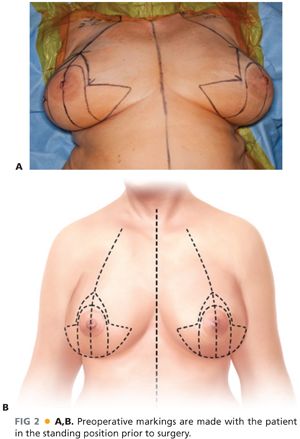
■ Preoperative markings with a permanent marker should be performed in the upright position in the preoperative holding area on the day of surgery.
■ The chest midline, breast meridian, and inframammary creases are initially marked. The inframammary crease should then be transposed onto the anterior breast to mark the desired new nipple position.7 The distance from the sternal notch/clavicle to this point is measured and transposed symmetrically to the other breast. Eight-centimeter obliquely vertical limbs are then drawn medially and laterally from this point. They should be separated by a distance of 8 to 10 cm between their inferiormost points, depending on the desired breast width reduction. The bases of the vertical limbs are subsequently connected medially and laterally with a curvilinear line that joins the inframammary crease. Minor adjustments are made to account for breast asymmetry and minimize the appearance of standing cones (FIG 2).
■ Although there is limited data to support the use of preoperative antibiotics for reduction mammoplasty, the general consensus among plastic surgeons is that prophylactic antibiotics covering skin flora should be administered at least 30 minutes prior to skin incision.8 Data can be also be extrapolated from several general surgery mastectomy studies demonstrating that antibiotic prophylaxis reduces the incidence of postoperative wound infections.9
Positioning
■ Reduction mammoplasty is performed under general endotracheal anesthesia.
■ Because the procedure requires intraoperative assessment of breast symmetry, shape, and contour in the semi-upright position, the patient should be placed in the supine position with the bed break at the hips. The patient’s arms should be securely padded on adjustable arm boards, ready for repositioning.
■ Sequential compression devices are applied to the lower extremities and a Foley catheter is inserted.
TECHNIQUES
PREINCISION INFILTRATION AND MARKINGS
■ The breast bases and planned incisions may initially be infiltrated with 1% Xylocaine with 1:100,000 epinephrine. Then, an 8- to 10-cm–wide inferiorly based dermal pedicle is marked on the skin of each breast, extending in a circular fashion above the NAC all the way down to the chest wall. Using a cookie cutter centered on the nipple, a 40- to 44-mm circular marking is made with the breast skin under minimal to no tension to reduce the diameter of the NAC (FIG 3). Tourniquets may then be placed around each breast base to assist with hemostasis (FIG 4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








