Reduction Mammoplasty With Inverted-T Incision
Ethan E. Larson
Maurice Y. Nahabedian
Shiliang Chang
Introduction
The evolution of reduction mammoplasty has been witness to a variety of techniques, principles, and concepts. Many of these have been related to skin pattern design, parenchymal reshaping, and pedicle orientation. Skin pattern designs can include short-scar techniques such as the vertical and horizontal incisions as well as the inverted-T or Wise incision. Parenchymal reshaping can be achieved using internal sutures or reliance of the skin envelope. Pedicle orientation can essentially be in any direction and includes superior, superomedial, medial, inferior, lateral, or central. Each of these techniques and modifications can be a topic unto itself. This chapter, however, focuses on Wise pattern or inverted-T skin incision in reduction mammoplasty.
Anatomy
The anatomy of the breast is complex but relatively constant. The borders of the breast typically extend vertically from the second to the sixth rib, and horizontally between the lateral sternal border and the anterior axillary line. The breast is composed of numerous lobules and ductules that lead to the nipple areolar complex (NAC). There is a superficial fascia layer, the breast capsule surrounding the breast to provide its shape and contour.
When considering a reduction mammoplasty, a thorough knowledge of the vascularity and innervation of the breast and NAC is important. There are several sources of blood supply to the breast. The perforating branches of the internal mammary, the lateral thoracic artery, the perforating branches from the pectoral vessels, and the intercostal vessels (Fig. 40-1). Studies on the vascular territories of the breast and NAC have demonstrated the internal mammary artery to be the dominant blood supply in 70% of patients (1). The innervation to the breast and NAC includes the medial and lateral branches of the intercostal nerves between the second and sixth vertebrae. The dominant innervation to the nipple is derived from the lateral cutaneous branch of the fourth intercostal nerve. Studies on the innervation of the NAC have demonstrated nerve branches from both the anterior (medial) and lateral fourth, fifth, and sixth intercostal nerves (1,2,3).
History of the Inferior Pedicle
Wise described his inverted T skin incision for reduction mammoplasty in 1956. Back then, Strombeck breast reduction technique utilizes deepithelialized horizontal bipedicle flap to reposition the NAC. In 1962, Paul McKissock rotated the pedicle design 90 degrees and performed the first vertical bipedicle flap for reduction mammoplasty. Later in 1977, Robbins described the inferior pedicle breast reduction (4,5,6).
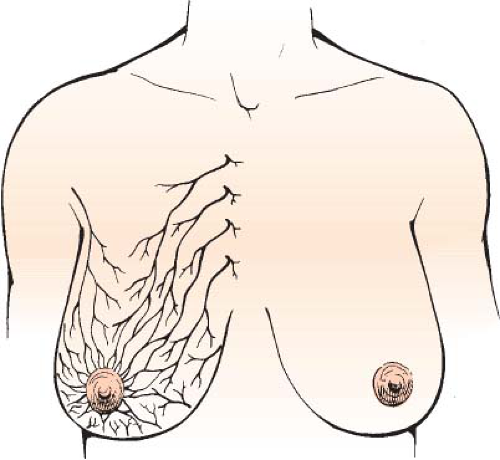 FIGURE 40-1 The principal blood supply to the breast includes perforating branches from the internal mammary and lateral thoracic systems. |
 FIGURE 40-2 Anteroposterior (A) and lateral (B) view of the typical posture seen in patients with symptomatic macromastia. |
Indications
Women with excessively large breasts who seek breast reduction often experience chronic pain and tension in their neck, shoulders, and upper back. Symptoms generally worsen later in the day. Associated symptoms include recurrent intertriginous skin irritations along the inframammary fold (IMF) and shoulder grooves from the pressure of supportive brassiere straps. Due to the excess breast tissue weight that pulls the shoulders forward, trapezius muscles may hypertrophy to compensate (Fig. 40-2).
Preoperative Considerations
As with all breast reductions, a standard medical history and examination of the pertinent systems should be performed (7). Special attention should be given to any history of bleeding disorders and conditions affecting wound healing, including tobacco use and diabetes. Problems arising from mammary hypertrophy, including back and neck pain, shoulder grooving, and intertriginous skin rashes or ulceration, need to be documented. The patient’s preoperative weight, height, cup size, and bra size should be noted and goals discussed for her ideal postoperative size. Deep vein thrombosis risk should be assessed, along with a history of contraceptive use or hormone replacement. Subjective nipple sensitivity should also be documented.
Findings on physical examination, family history of breast cancer, and patient’s age determine the need for screening mammogram. A preoperative mammogram is recommended for any woman younger than 50 years of age with a family or personal history of breast cancer. Otherwise, a biennial screening mammogram is recommended for women between age 50 and 74 years according to the U.S. Preventive Services Task Force guidelines released in 2016 (8). The incidence of occult breast cancer found during pathologic examination of breast reduction specimens is reported as 0.06% to 2.4% (9,10,11,12).
A set of measurements can be useful as guidelines to design the pedicle width and estimate the resection breast volume. These include the nipple-to-sternal notch distance, the nipple-to-IMF distance, and the nipple-to-nipple distance. Several methods have been used to estimate resection breast volume including the Schnur, Appel, Descamps, and Galveston scales (13,14,15). The Schnur sliding scale estimates resection weight based on the patient’s body surface area. On the other hand, Descamps method estimates resection volume based on a regression analysis using breast measurements such as the nipple-to-sternal notch distance and nipple-to-IMF distance. Appel scale uses a combination of breast measurements and body mass index to estimate the resected volume. Galveston scale adds age into the regression analysis of breast measures and body mass index (15).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







