PREOPERATIVE WORKUP FOR ANY BREAST SURGERY
I. COMPLETE MEDICAL HISTORY
A. Family history of breast cancer
B. Abnormal mammograms or previous breast surgeries
C. Pregnancies, breast-feeding, future childbearing plans
D. Smoking history
E. History of any bleeding disorders or diabetes
F. History of deep vein thrombosis/pulmonary embolism or hypercoagulability (e.g., factor V Leiden, protein C or S deficiency, and use of birth control pills)
II. COMPLETE PHYSICAL EXAMINATION
A. Detailed breast examination for masses and axillary examination for lymphadenopathy
B. Assess breast size and shape (e.g., tuberous, wide, and loss of superior pole fullness)
C. *Evaluate the degree of ptosis
1. Grade 1 (minor ptosis): Nipple lies at or above the inframammary fold (IMF).
2. Grade 2 (moderate ptosis): Nipple is 1 to 3 cm below IMF but above the lowest breast contour.
3. Grade 3 (major ptosis): The nipple is >3 cm below the IMF and is at the lowest breast contour.
4. Pseudoptosis: Nipple is above IMF but breast tissue hangs below the fold.
D. Skin quality
1. Tone
2. Striae
3. Elasticity
E. Symmetry
1. Chest wall evaluation
2. Breast volume
3. Difference in direction and height of nipple–areolar complex (NAC)
4. Difference in IMF height
F. Key measurements to do while patient sitting upright
1. Sternal notch to nipple
2. Nipple to IMF
3. Base width
III. PREOPERATIVE MAMMOGRAM
If the patient is >35 years old or has positive family history
BREAST REDUCTION (REDUCTION MAMMOPLASTY)
I. PREOPERATIVE CONSULTATION
A. Indications for surgery
1. Physical
a. Upper back, neck, and shoulder pain
b. Shoulder grooving
______________
*Denotes common in-service examination topics
c. Recurrent intertrigo and maceration of inframammary skin
d. Exercise restriction
e. Inability to find clothes that fit
2. Psychological
a. Embarrassment
b. Feelings of physical unattractiveness
c. Uncomfortable in clothes, difficulty with clothing/bra fit
B. Patient education: Important discussion points pre-op
1. Breast reduction involves significant scarring. Patient is trading larger breasts for smaller breasts with scars.
2. Everybody is asymmetric: Point out specific asymmetries in nipple position, size, and shape pre-op. Some asymmetries will persist post-op.
3. Approximately 30% of patients cannot breast-feed postoperatively (the same percentage of patients with macromastia who cannot successfully breast-feed).
4. Nipple sensation can change post-op, 5% of patients will have permanent nipple numbness.
5. Smoking increases the risk of nipple or flap loss and delayed healing.
6. Weight gain or future pregnancies can cause recurrent enlargement.
7. All symptoms may not improve postoperatively.
8. New baseline mammogram needed ∼6 months following surgery.
9. Breast reduction patients are generally one of the most satisfied groups of patients.
III. SURGICAL APPROACHES
The most common surgical approaches are outlined below
A. Goals
1. Reduction and reshaping of the gland
2. Creation of an NAC pedicle, superior repositioning of NAC
3. Skin reduction and redraping
4. Remember, it is not what is removed but rather what is left behind that really matters in reduction surgery
B. Considerations in selecting the appropriate surgical approach
1. Skin removal: Necessary to primarily adjust the skin envelope to the reduced breast volume and to reposition the nipple
2. Areas of breast resection
3. Amount of breast reduction
4. Incision length and placement
5. Lateral and abdominal fullness
6. Preservation of breast and nipple sensation
7. Size and position of the NAC
C. Wise pattern reduction
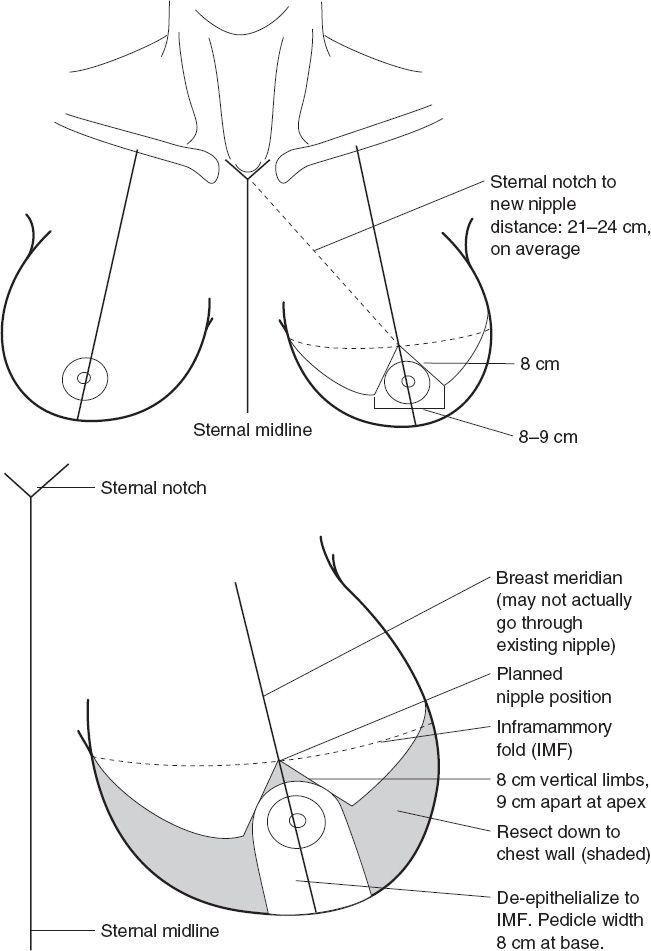
1. “Wise pattern” describes skin incisions (Fig. 36-1)
a. “W”-shaped incision allows significant skin resection, good for large volume or very ptotic breasts. Allows large movement of NAC.
b. “Pedicle” describes glandular tissue that keeps NAC attached to the chest wall for blood supply. Wise pattern reduction can be used with any pedicle (inferior, superomedial, superior, etc.).
c. Wise pattern relies on skin redraping to reshape the remaining gland.
2. Advantages
a. Reproducible, straightforward, and easily taught. To a large extent, skin incisions correspond to glandular incisions of breast parenchyma.
b. Applicable to large variety of breast shapes and sizes, especially when using inferior pedicle technique.
c. Breast-feeding is potentially more likely since a large amount of breast tissue is left beneath the nipple.
d. Higher rate of nipple sensory preservation.
3. Disadvantages
a. Produces more extensive scars than other techniques: “Anchor”-shaped scar starts around NAC, vertically down to IMF, and along entire IMF.
b. Breasts may “bottom out” over time.
Figure 36-1. Wise pattern, inferior pedicle design for breast reduction.
4. Markings (Fig. 36-1)
a. Registration marks: Sternal notch, midline, IMFs
b. Breast meridian: From midpoint of clavicle to nipple
i. Can drape a tape measure around patients neck down to the nipple and trace a line along it to find breast meridian.
ii. Line should be relocated medially if it is more than 10 to 12 cm from the midline.
c. New nipple position can be determined by several methods
i. Place hand under breast at level of IMF, transpose that point onto front of the breast along meridian.
ii. Find Pitanguy point: 1 to 2 cm below mid-humeral point on breast meridian.
iii. 21 to 24 cm from the sternal notch along breast meridian.
d. Vertical limbs are drawn obliquely from the intended nipple position. These will create an isosceles triangle—8 cm on each side and approximately 9 cm across the base (these numbers are variable based on patients’ habitus and breast size).
e. Draw curvilinear lines from the base of triangle to medial and lateral endpoint of breast, connecting to IMF line.
f. If doing inferior pedicle, mark out the base of pedicle when the patient is supine on operating room table with a base width of 8 to 10 cm.
g. Mark out 42-mm areola when patient on table.
h. Can either dissect out pedicle first and then breast flaps or breast flaps first
i. Important not to undermine pedicle
j. Can be helpful to place medial tacking suture on pedicle to prevent it from migrating laterally.
k. Tailor tack after resection is done, sit the patient up, and place 38 nipple sizer.
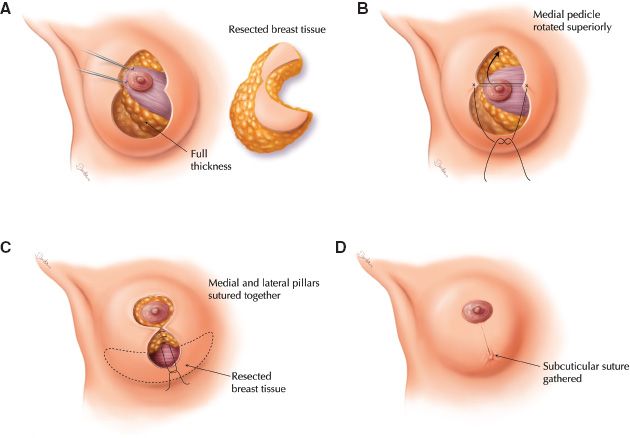
C. LeJour vertical reduction (Fig. 36-2)
1. Markings
a. IMF and chest midline and vertical axis of the breast are marked
b. Future nipple position placed at the forward projection of the center point of the IMF:
i. 18 to 22 cm to sternal notch
ii. 10 to 14 cm from midline
Figure 36-2. Vertical reduction technique (LeJour). A: Full thickness breast tissue with overlying skin is resected following the markings. Most of the resection comes from the inferior pole of the breast. The skin resection leaves the nipple attached to the underlying dermis. The blood supply comes from the superomedial dermal pedicle. The gland is sutured to the superior pectoralis fascia to position it more superiorly. B: After securing the gland to the pectoralis fascia, the skin is sutured to form the lower closure of the areola. C: The medial and lateral pillars are sutured together. D: The skin is closed, leaving “gathers” that will smooth with time. The patient must be informed that the shape of the breast will improve over time.
c. Lateral markings are determined by pushing the breast medially and laterally.
d. The lower margin is drawn 2 to 4 cm above the IMF connecting the medial to the lateral lines.
e. The periareolar markings are drawn in “mosque shape” and are typically 14 to 16 cm in length.
2. Gland reduction: Inferior central pole of breast, remaining medial and lateral pillars reapproximated to reshape the gland
3. Nipple pedicle: Superior
4. Redraping: Skin adapts to the breast shape
5. Technique
a. Periareolar area is de-epithelialized to 3 to 4 cm inferior to the areola.
b. Liposuction is performed if desired.
c. Lateral vertical markings are incised, creating 1-cm-thick flaps going obliquely downward and terminating at the IMF.
d. From the IMF the gland is undermined superiorly and a 6- to 8-cm-wide tunnel is created up to the third rib.
e. The lateral pillars and the superior gland are left intact
f. The gland is sutured superiorly to the pectoralis fascia to elevate the areola which is sutured to its new site.
g. The lateral pillars are brought together and sutured to shape the glandular cone.
h. Skin is closed with deep 3-0 and running subcuticular sutures around the areola and the vertical scar gathering the vertical component.
6. Advantages
a. Eliminates incision in IMF
b. Less “bottoming out” than with inferior pedicle technique
7. Disadvantages
a. Steep learning curve
b. On-table result not consistent with the final result. Will be significant puckering of the skin around nipple/vertical scar and flattening of lower pole which resolve within 4 to 6 weeks.
D. Periareolar reduction
1. Gland reduction: Central wedge
2. Nipple pedicle: Superior
3. Redraping: Skin redraped in purse-string manner around areola
4. Advantages: Minimal scarring
5. Disadvantages
a. Tends to flatten breast in anteroposterior dimension
b. Areola may widen with time
c. Limited to small reductions
E. SPAIR technique (Short scar, PeriAreolar, Inferior pedicle Reduction)
1. Gland reduction: Mostly periareolar
2. Nipple pedicle: Inferior
3. Redraping: Skin redraped around areola
4. Advantages
a. Maintains shape over time with less “bottoming out”
b. Minimizes scarring by eliminating IMF incision
c. Achieves attractive breast shape
5. Disadvantages
a. Steep learning curve and significant intraoperative decision making
b. Extensive glandular suturing required to obtain desired shape
F. Free nipple graft technique
1. Indications
a. Gigantomastia (>2,500 g breast tissue)
b. Thresholds vary, but strongly considered by some surgeons when nipple to IMF distance is >20 to 25 cm.
c. Comorbidities necessitating decreased operative time and blood loss.
a. Breast amputation combined with the removal of NAC with replacement as a full-thickness skin graft.
b. Helps to keep an inferior mound that is de-epithelialized to maintain projection.
3. Advantages
a. Decreased operative time
b. Straightforward, easy to perform
4. Disadvantages
a. Permanent nipple numbness
b. Eliminates the ability to lactate and nurse, so not ideal in younger patients
c. Risk of nipple graft loss
d. Risk of depigmentation of areola
G. Liposuction
1. May be performed alone or as an adjunct to excisional reduction
2. Indication: Useful in women with elastic skin, predominantly fatty breasts, and nipples in a nonptotic position.
3. Advantages
a. Minimal external scarring
b. Symmetry easily achieved
4. Disadvantages
a. Specimen cannot be sent for pathologic evaluation
b. Does not address nipple ptosis or skin laxity
c. May be difficult in patients with dense breast tissue
d. Few patients are candidates: Limited to small reductions in nonptotic breasts
IV. COMPLICATIONS
A. Wound healing delays, especially at T-junction in Wise pattern reduction
B. Asymmetry: 8% to 18%
C. Changes in nipple sensitivity: 25% to 60%
D. Unacceptable scar: 18%
E. Hematoma
F. Seroma
G. Infection
H. Fat necrosis
I. Nipple loss
J. Hypertrophic scarring
K. Inadequate reduction or over-resection
L. Inability to breast-feed
BREAST AUGMENTATION
I. PREOPERATIVE CONSULTATION
A. History
1. Motives for breast augmentation, current family situation, any recent life events influencing decision
2. Patients’ goals and expectations
3. Complete breast and medical history (see Section “Preoperative Workup for Any Breast Surgery”)
4. Obtain preoperative photographs
B. Physical
1. Complete breast examination (see Section “Preoperative Workup for Any Breast Surgery”)
2. Bring asymmetries to patient’s attention prior to surgery. Asymmetries (e.g., nipple position) may be amplified after augmentation.
3. Measure breast base width which will ultimately determine maximum size of the implant.
C. Patient education
1. Implants are not permanent and one or both may need to be removed or replaced in the future.
2. Implants may impact cancer monitoring (see “Breast Cancer Detection in Augmented Women”)
II. SURGICAL APPROACHES
A. Incision
1. Inframammary
a. Most common
b. Incision placed 1 to 3 cm above crease start at nipple and extend lateral about 3 to 5 cm.
c. Allows excellent exposure and good control of implant position; places scar on breast surface.
d. Best for women with well-defined IMF, no hypertrophic scarring and mild ptosis.
e. Mark out limits of implant pocket
i. Second rib
ii. Laterally to midaxillary line or lateral extent of proposed breast after augmentation.
iii. Medially to most medial extent of pectoralis major but not to midline
iv. Center of implant should not be above the nipple level or it will be too high.
f. When dissecting laterally, dissect bluntly to avoid any branch of lateral cutaneous nerves.
2. Periareolar
a. Incision placed along inferior half of areola from 3 o’clock to 9 o’clock position.
b. Dissection performed directly through gland, which may result in fat necrosis/nodularity post-op.
c. May get hypertrophic scar or hypopigmentation if within areola.
3. Transaxillary
a. Incision in uppermost axillary fold
b. Scar hidden within axilla; somewhat blind dissection unless endoscopy is used; less control of implant position, particularly with regard to IMF.
c. Risk of injury to intercostobrachial nerve leading to axillary and posteromedial numbness of upper arm.
4. Transumbilical breast augmentation
a. Incision at umbilicus
b. Blind dissection with least control of implant position
c. Can only use saline implants
B. Implant type
1. Saline
a. Advantages
i. Can use smaller incision since implant is inserted deflated
ii. May adjust fill volume to some degree
iii. Implant leakage easily detectable and safe since saline absorbed
iv. Lower rate capsular contracture
b. Disadvantages: Visible rippling of implant, especially in thin women
c. All air should be removed prior to filling to prevent “sloshing”
d. Overfilling not only leads to less wrinkling but also makes implant more firm.
e. Underfilling leads to increased rupture.
2. Silicone gel
a. Advantages
i. Look and feel more natural, similar to breast tissue
ii. Less visible rippling
b. Disadvantages
i. Leaks can go undetected for long periods of time
ii. Slightly higher risk of capsular contracture
c. *“Linguine sign” on magnetic resonance imaging (MRI) and “snowstorm” appearance of free silicone in the breast tissue on ultrasound are indicative of implant rupture.
d. *Previous recommendation from Food and Drug Administration (FDA) is to obtain MRI 3 years following implantation and then every 2 years to screen for rupture; however, this is under review
e. *Minimum age for silicone implants is 22.
C. Implant shell type
1. Textured
a. Designed to reduce the incidence of capsular contraction, though only demonstrated with gel implants.
b. Creates cohesion between the implant and the surrounding tissue, decreasing implant mobility.
2. Smooth
a. Higher rate of capsular contracture than textured gel implants, but not textured saline.
b. Moves freely within the breast pocket.
D. Implant shape
1. Anatomic: Includes teardrop, contoured, or shaped implants. Intended to mimic the slope of a natural breast with decreased upper pole projection. Surface is textured to prevent the implant from moving.
2. Round: Assume a natural teardrop shape when the patient stands. Smooth or textured surface.
a. Low profile
b. Moderate profile
c. Moderate plus profile
d. High profile
i. Greater projection for a given base width
ii. Get greater projection with less volume
iii. Advantageous if lower pole constriction or narrow breast base width
E. Pocket position
1. Subpectoral (complete submuscular)
a. Superior part of implant under pectoralis major, inferolateral part of implant under serratus fascia.
b. Best for mammographic visualization of breast tissue
c. Lower risk of capsular contracture and visible rippling
d. Flexing of muscles can contract implant into unnatural position
e. Less risk to compromise nipple sensation
2. Dual plane (partial submuscular)
a. Superior part of implant under pectoralis major, inferior part of implant under breast tissue only.
b. Pectoralis major can be detached from inferior attachments in women with tight IMF.
c. Risk of visible rippling of lower portion of implant.
d. Expands lower pole and decreases the risk of double-bubble appearance.
e. Allows the implant to sit along IMF.
3. Subglandular
a. Implant placed under breast tissue only, above pectoralis major
b. Less painful
c. Mammograms more difficult
d. Highest risk for visible or palpable wrinkling
e. Higher rate of capsular contracture
III. COMPLICATIONS
A. Early: Hematoma, seroma, infection—Staphylococcus aureus and Staphylococcus epidermidis most common, loss of nipple sensation
B. Late
1. Capsular contracture: Firm fibrous scar forms periprosthetic shell around implant
a. *Baker classification describes the degree of capsular contracture
i. I: Normal—soft, no visible or palpable firmness
ii. II: Palpable—minimal contracture with palpable but not visible firmness
iii. III: Visible—moderate contracture with palpable and visible firmness
iv. IV: Painful: Severe contracture with palpable and visible firmness plus pain
b. Grade III and IV contractures can only be treated with open capsulotomy (release of scar tissue) or capsulectomy (removal of scar tissue)
i. Capsulectomy done in subglandular plane with caution anteriorly
ii. Capsulotomy done with radial scoring
c. Closed capsular release is not recommended due to high recurrence and complication rates.
d. Rates close to 30% for subglandular and 10% for subpectoral
e. Higher rates in reconstruction (25% to 30%) than in augmentation (10%)
2. Implant rippling: More common with saline implants
3. Implant leak or rupture
a. Causes
i. Underfilling
ii. Fold flaw
iii. Technical errors
b. Diagnosis
i. Physical examination
ii. MRI for silicone implants may be needed
iii. Ultrasound can be used (snowstorm appearance)
4. Implant malposition or unsatisfactory shape
a. Double bubble: Contour of implant visible above breast tissue secondary to excessively high implant placement.
b. Snoopy nose: Breast tissue hangs off inferior aspect of implant secondary to ptosis.
5. Upper arm numbness secondary to injury to intercostobrachial nerve (transaxillary approach).
6. Nipple sensation altered in 15% of patients
IV. BREAST CANCER DETECTION IN AUGMENTED WOMEN
A. Physical examination and mammography more difficult due to implants.
B. American College of Radiology recommendations
1. Screening schedule should be same as for women without implants.
2. Imaging should be done at centers with experience reading augmented mammograms.
3. Implant displacement views (Eklund views) should be performed to enable more breast tissue to be visualized.
V. SILICONE IMPLANT CONTROVERSY
A. FDA mandated a moratorium on silicone implants in 1992 to investigate association between silicone implants and connective tissue diseases.
B. Multiple large, population-based retrospective studies show no association.
C. Silicone implants reapproved for cosmetic and reconstructive use in 2006.
VI. ANAPLASTIC LARGE CELL LYMPHOMA
A. Very rare non-Hodgkin lymphoma possibly associated with breast implants.
B. Patients with late seroma (>6 months post-op) should have aspiration for diagnosis.
C. Further studies needed to clarify association.
MASTOPEXY
I. PATHOPHYSIOLOGY OF PTOSIS
A. Normal breast anatomy
1. Gland spans from second to sixth rib
2. NAC sits superior to IMF and centrally over breast mound
3. Average sternal notch to nipple distance is 21 to 24 cm.
4. Average nipple to IMF distance is 6 to 7 cm.
5. Parenchymal blood supply
a. Lateral thoracic artery
b. Thoracodorsal artery
c. Perforators from internal mammary artery
d. Intercostal artery perforators
e. Thoracoacromial artery
6. Innervation
a. Branches of intercostal nerves T3–T5
b. NAC receives sensation from T4
7. Cooper’s ligaments connect parenchymal to dermis and are responsible for the degree of ptosis.
B. Anatomic changes in ptotic breasts
1. Nipple moves inferiorly, increasing sternal notch to nipple distance
2. Parenchyma of breast gland hangs below IMF
3. Connective tissue (Cooper’s ligaments) stretches with loss of elasticity
4. Etiologies include breast parenchyma involution after pregnancy, excess residual skin after weight loss, loss of skin elasticity secondary to aging, and gravitational forces.
II. PREOPERATIVE CONSULTATION
A. History
1. Complete medical history as outlined above
2. Mammographic studies
B. Physical
1. Degree of ptosis (see Section “Preoperative Workup for Any Breast Surgery”)
2. Evaluate the amount and quality of excess skin
3. Note the patient’s weight and body habitus
4. Volume of parenchyma
5. Breast asymmetry
6. Breast masses
C. Indications
1. Adequate breast parenchyma with ptosis of NAC
2. Ptosis of NAC
3. Patient willing to accept scars
D. Patient education
1. Ptosis can recur with aging
2. Scarring may be significant, depending on planned procedure
3. Augmentation may be beneficial to achieve optimal result in women with deficient breast tissue
4. Discuss asymmetries pre-op
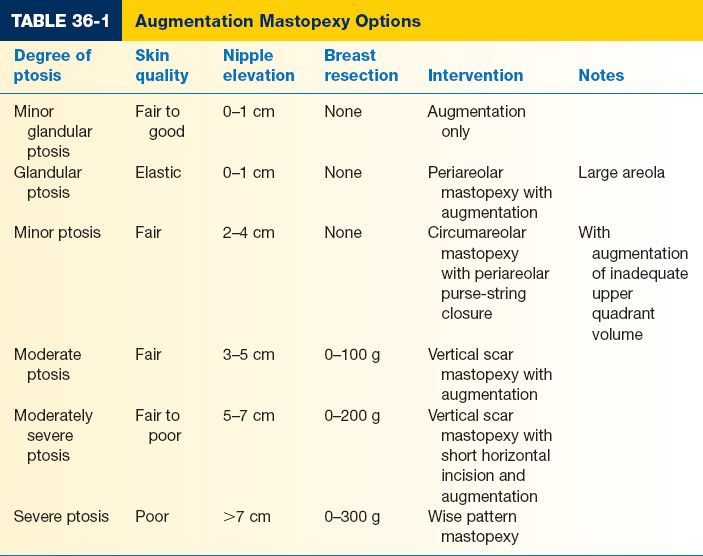
III. SURGICAL APPROACHES
A. The degree of ptosis is the most important factor in determining which procedure to perform
B. Mastopexy techniques
1. Periareolar mastopexy (Benelli)
a. Best for patients with grade I ptosis and good to fair skin quality
b. Periareolar incision with purse-string suture around NAC
c. Minimal scarring
d. Limited movement of NAC possible
e. NAC can widen over time
f. Steep learning curve
g. The upper periareolar excision can elevate the areola about 1 cm
h. Any excessive skin resection will significantly deform the areola circle
2. Vertical pattern
a. Similar markings to LeJour reduction mammoplasty
b. Best for patients with grade II ptosis
c. Final scar is periareolar plus vertical component from NAC to IMF
d. Enables more NAC movement and skin/gland tailoring
e. Takes several months for breasts to obtain final shape
f. Can add short horizontal component to increase skin resection
g. Technique
i. Markings similar to LeJour reduction: Displace the breast medially and laterally to draw vertical lines between the new NAC and a point 1 cm above the IMF
ii. Areola is left in situ and the upper and lower areas are de-epithelialized
iii. Excision of lower breast tissue in V and upward transposition
iv. Placement of subpectoral implant above and subglandular below
v. NAC transposition with inset into new position
vi. Placement of subcuticular stitch to cinch the vertical scar down
3. Wise pattern
a. Best for patients with grade III ptosis
b. Significant scarring including periareolar, vertical, and IMF scars
c. Long horizontal component allows large skin resection in significantly ptotic breasts
d. Predictable and straightforward, as the final shape of the breast is achieved in the operating room.
e. Technique
i. A superior, medial, or inferior pedicle technique may be used.
ii. The top of the new NAC is 1 to 2 cm above the IMF.
iii. Limbs of the equilateral triangle are 7 to 8 cm Augmentation + mastopexy (Table 36-1).
f. Patients with deficient breast tissue for existing skin envelope may benefit from combination augmentation + mastopexy.
g. Patients with grade I ptosis may only require augmentation in some cases for correction of ptosis.
h. May be performed as a one-stage or two-stage procedure
i. One-stage procedure is challenging and has high risk of wound healing complications and skin necrosis.
ii. Two-stage procedure separates mastopexy and augmentation by 3 to 6 months to allow delay of skin flaps and preserve blood supply.
i. Any mastopexy that involves wide undermining of skin flaps should NOT be combined with augmentation due to the risk of flap necrosis.
II. COMPLICATIONS
A. Hematoma
B. Seroma
C. Changes in nipple sensitivity
D. Unacceptable scarring
E. Nipple malposition and asymmetry
F. Nipple loss and flap necrosis
G. Recurrent ptosis
PEARLS
1. Check a urinary cotinine test preoperatively in “former” smokers before performing a breast reduction
2. Always point out any asymmetries to patients prior to surgery
3. Breast implants are not “permanent.” Most women will need one or both replaced in their lifetime.
QUESTIONS YOU WILL BE ASKED
1. How is breast ptosis categorized?
Based on the nipple position relative to the IMF.
2. What classification scheme is used to describe the degrees of capsular contracture?
Baker classification.
3. What are the advantages and disadvantages of saline and silicone gel implants?
See “Breast Augmentation IIB.”
THINGS TO DRAW
Breast markings for Wise pattern technique (see Fig. 36-1)
Recommended Readings
Jewell M, Spear S, Largent J, et al. Anaplastic large T-cell lymphoma and breast implants: a review of the literature. Plast Reconstr Surg. 2011;128:651–661. PMID: 2186599.
Noone R. An evidence-based approach to reduction mammaplasty. Plast Reconstr Surg. 2010;126: 2171–2176. PMID: 21124157.
Rohrich R, Thornton J, Jakubietz R, et al. The limited scar mastopexy: current concepts and approaches to correct breast ptosis. Plast Reconstr Surg. 2004;114:1622–1630. PMID: 15509961.
Thorne C. An evidence-based approach to augmentation mammaplasty. Plast Reconstr Surg. 2011;128:596–597. PMID: 21124159.
< div class='tao-gold-member'>