Reduction Mammaplasty Using Medial Pedicles and Inverted-T Incisions
Ethan E. Larson
Maurice Y. Nahabedian
Introduction
The evolution of reduction mammaplasty has been witness to a variety of techniques, principles, and concepts. Many of these have related to skin pattern design, parenchymal reshaping, and pedicle orientation. Skin pattern designs can include short-scar techniques such as the vertical and horizontal incisions as well as the inverted-T or Wise pattern. Parenchymal reshaping can be achieved using internal sutures or reliance of the skin envelope. Pedicle orientation can essentially be in any direction and includes inferior, superior, lateral, or medial. Each of these techniques and modifications can be a topic unto itself based on the subtleties associated with each. This chapter, however, focuses specifically on Wise pattern reduction mammaplasty using a medial or superomedial pedicle.
Anatomy
The anatomy of the breast is complex but relatively constant. The borders of the breast typically extend vertically from the second to the sixth rib and horizontally between the lateral sternal border and the anterior to midaxillary line. The breast is composed of numerous lobules and ductules that lead to the nipple-areolar complex. There is a layer of investing fascia surrounding the breast that provides shape and contour.
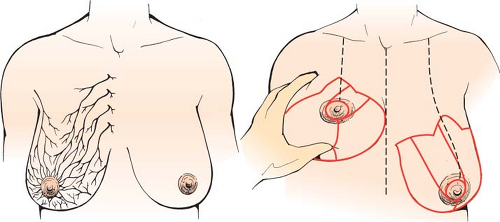
When considering a reduction mammaplasty, a thorough knowledge of the vascularity and innervation of the breast and nipple-areolar complex (NAC) is important. The vascularity of the breast is derived from various sources that include the perforating branches of the internal mammary, the lateral thoracic artery, perforating branches from the pectoral vessels, and the intercostal vessels (Fig. 97.1). The innervation to the breast and NAC includes the medial and lateral division of the intercostal nerves between the second and sixth vertebrae. Studies on the vascular territories of the breast and NAC have demonstrated the internal mammary artery to be the dominant blood supply in 70% of patients (1). Studies on the innervation of the NAC have demonstrated fine branches from both the anterior (medial) and lateral fourth, fifth, and sixth intercostal nerves (2,3).
History of the Medial and Superomedial Pedicles
Preserving the vascularity to the NAC during a reduction mammaplasty is accomplished by designing a pedicle of tissue that includes the NAC at its distal aspect (Fig. 97.2). The number of potential pedicles is large, and the indications for use are described in other chapters. There are two medially based pedicles that include the superomedial pedicle and the medial pedicle. The superomedial pedicle was introduced by Orlando and Guthrie in 1975 (Fig. 97.3) (4). Its design was intended to shorten pedicle length while broadening the pedicle as a means to enhance blood flow and maintain innervation of the NAC. Subsequent reports by Hauben and Finger et al. verified the safety, reliability, and speed of this procedure (5,6,7). The medial pedicle was introduced several years later by Hall-Findlay in 1999 using vertical scar techniques and by Nahabedian et al. in 2000 using Wise pattern techniques (8,9). The medial pedicle differed from the superomedial pedicle in that the medial edge of the pedicle was oriented at 10 o’clock (left breast) or 2 o’clock (right breast) position. The superomedial pedicle is oriented such that the medial edge is at the 12 o’clock position. The advantage of medial pedicle was to facilitate the arc of rotation and to prevent kinking of the pedicle. In 2005, Abramson et al. confirmed the durability of medial pedicle reduction mammaplasty (10). As with all pedicles, there was lengthening of the distance between the inframammary fold (IMF) and nipple that increased by 11% after 1 year when the resection volume was between 500 and 1,200 g per breast and by 34% when the resection volume exceeded 1,200 g per breast. The complication rate in this series was 6.8%. Davison et al. in 2007 reported on the benefits of the superomedial pedicle for breast reduction in a series of 279 patients and reported no cases of nipple loss and an overall complications rate of 18% with a time savings of 41 minutes over the inferior pedicle technique (11). Landau et al. in 2008 reported a series of 122 women following superomedial reduction mammaplasty and demonstrated no cases of nipple loss in women who had a resection volume that averaged 1,379 g per breast (12).
Indications for Using A Medially Based Pedicle
The indications for using the superomedial or medial pedicle are several. In general, a superomedial pedicle is used when the distance of nipple areolar elevation ranges from 4 to 6 cm (Fig. 97.4). The medical pedicle is used when the distance is greater than 6 cm (Fig. 97.5). The reason for this is based on the arch of rotation of each pedicle. When the distance of nipple elevation is less than 6 cm, the NAC will not rotate easily when based on a medial pedicle. However, it will advance easily when based on a superomedial pedicle. In some cases, a small back-cut will be necessary at the origin or base of the pedicle to facilitate rotation and advancement. In contrast, when the distance of NAC elevation exceeds 6 cm, the medial pedicle will rotate easily without kinking or twisting. When the distance of NAC elevation is less than 4 cm, it is our preference to use a central cone technique in which the vascularity of the NAC is based on
the perforating branches emanating off of the pectoralis major muscle. The NAC is easily advanced using this technique.
the perforating branches emanating off of the pectoralis major muscle. The NAC is easily advanced using this technique.
In addition to the anatomic indications, the medial pedicle offers other advantages. By conserving breast tissue medially and resecting tissue inferiorly and laterally, this technique tends to augment the medial portion of the breast, providing fullness where it is most desired and eliminating tissue where it is not. Although medial pedicles will have some degree of “bottoming out” over time, it is generally less than that associated with inferiorly based pedicles. The risk of “boxy”-appearing breasts, particularly in the immediately postoperative period, is also diminished. Medial pedicles permit ample lateral parenchymal excision and can be designed with a limited horizontal incision to improve shape and contour. With several reduction techniques, internal suturing techniques are recommended for shape and contour; however, with the medial pedicle approach, internal suturing is rarely necessary. Because the majority of skin excision is inferior, the upper cutaneous envelope is usually sufficient to support the retained parenchyma on the skin envelope alone.
In cases of severe mammary hypertrophy, defined as resection volume exceeding 1,200 g per breast, the medial pedicle is an excellent option (9). The NAC is often well vascularized based on the internal mammary and chest wall perforating
vessels. This is frequently an alternative to amputation and free nipple graft. Resection volumes in excess of 2 g per breast are frequently amenable to a medial pedicle reduction mammaplasty. In order to minimize the incidence of partial or total NAC necrosis, the distal edges of the pedicle are evaluated for arterial and venous bleeding. When absent, it can be assumed that perfusion will be compromised, and the operation is converted into an amputation technique with free nipple graft.
vessels. This is frequently an alternative to amputation and free nipple graft. Resection volumes in excess of 2 g per breast are frequently amenable to a medial pedicle reduction mammaplasty. In order to minimize the incidence of partial or total NAC necrosis, the distal edges of the pedicle are evaluated for arterial and venous bleeding. When absent, it can be assumed that perfusion will be compromised, and the operation is converted into an amputation technique with free nipple graft.
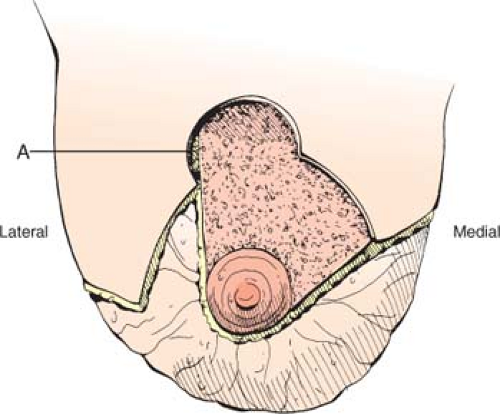 Figure 97.2. The general outline of the superomedial pedicle. Note that the central arm of the pedicle is oriented vertically. |
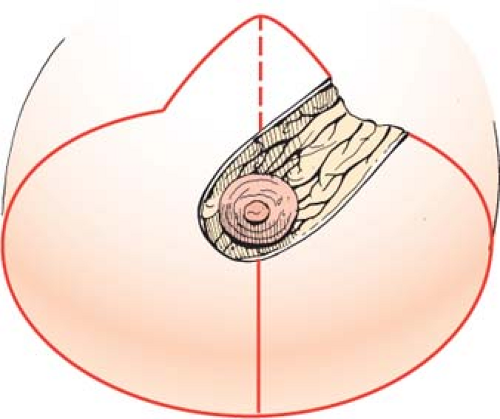 Figure 97.3. The general outline of the medial pedicle. Note that the central arm is oriented obliquely. |
Preoperative Considerations
As with all breast reductions, a standard medical history and examination of the pertinent systems should be performed (13). Special attention should be given to any history of bleeding diathesis. Similarly, conditions affecting wound healing, including tobacco use and diabetes, should be addressed. Problems arising from mammary hypertrophy, including back and neck pain, shoulder “grooving,” intertrigo, and skin ulceration, should be documented. A breast-feeding history should be documented, including maximal breast size achieved. Similarly the patient’s preoperative weight, height, cup size, and bra size should be noted and goals discussed for her ideal postoperative size. Deep vein thrombosis risk should be assessed, along with a history of contraceptive use or hormone replacement. Family history of breast cancer should be sought and a preoperative mammogram obtained in any woman younger than 40 years of age with a family history of breast cancer or older than 40 years of age without one. Subjective nipple sensitivity should also be documented and recorded.
 Figure 97.5. A typical patient for a medial pedicle. The distance of nipple-areolar complex elevation usually ranges from 6 to 16 cm. |
A set of measurements can also be useful as guidelines in selecting the ideal candidate for a medial pedicle breast reduction as well as to assess the degree of breast symmetry. These include the nipple-to-IMF distance, the nipple-to-sternal notch distance, the base width of the breast, and the proposed length of the pedicle (measured from the medial skin flap to the nipple). Body mass index (BMI) should also be calculated and an estimate of the final resection volume made.
There are several breast-related parameters that should be noted and considered before considering a medial pedicle reduction mammaplasty. The ideal candidate should have a pedicle length that does not exceed 16 cm. Pedicles exceeding 16 cm sometimes necessitate a free nipple graft (10,11). Previous breast incisions that could compromise vascularity should be noted, and the pedicle design should be adjusted accordingly. The medial pedicle can safely be employed in reductions of up to 2,500 g per side and has been reported in reductions of up to 4,100 g (6,9). Women of a larger body habitus should be counseled preoperatively regarding the additional possible problems with wound healing, the possibility of conversion to a free nipple graft, and the likely emergence of their lateral axillary fat roll and large abdomens as possible aesthetic problems in the future.
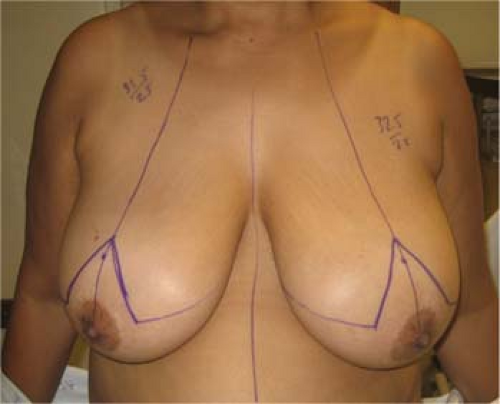
Patient Markings: Medial Pedicle
The patient is always marked in the standing position. Standard breast landmarks include the sternal midline, IMF, suprasternal notch, and breast meridians (Fig. 97.6). The anticipated nipple position is marked at the IMF along the breast meridian. The actual distance of the NAC to the sternal notch is variable and is usually ranges from 22 to 26 cm. The inverted-T pattern is delineated (Fig. 97.7). This can be drawn using the templates or freehand. It is our practice to draw it freehand based on the standard breast landmarks. The vertical limbs of the pattern are usually 8 to 9 cm. The apical angle of the vertical limbs ranges from 50 to 70 deg but is usually 60 deg. A keyhole pattern for the NAC can be delineated if desired, but it is our preference to excise the keyhole following the parenchymal resection rather than prior to it. The horizontal limbs of the inverted-T pattern extend from the inferior point on the vertical limb to the lateral point along the IMF. In larger breasts, the surgeon must choose a point laterally where the breast ends and the axillary adipose tissue begins. These marking are typically drawn outside of the operating room. The remaining markings are made in the operating room.
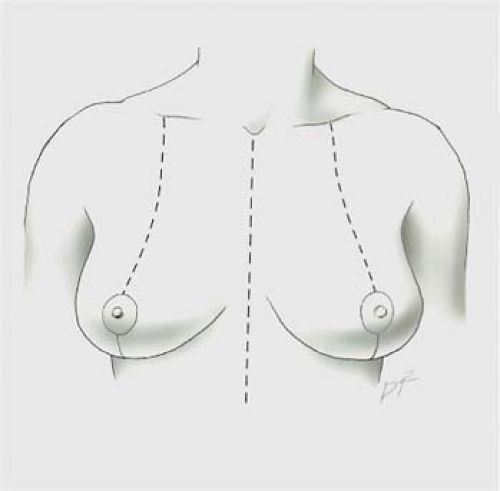 Figure 97.6. Standard preoperative markings include the sternal midline, breast meridians, and the inframammary folds. |
In the operating room, the patient is placed in the supine position. The medial pedicle is designed with a base width that ranges from 5 to 10 cm and a pedicle length that ranges from 8 to 16 cm (Fig. 97.7). The superior arm of the medial pedicle is based at the midpoint of the 8-cm vertical limb of the inverted-T pattern. This point will allow for the NAC (with a diameter of 4 cm) to rotate into the apex of the vertical limbs following the parenchymal resection.
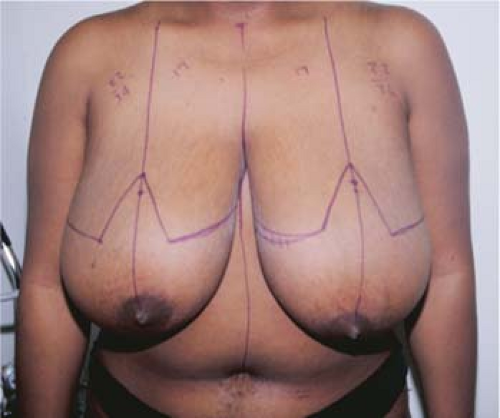 Figure 97.7. Standard inverted-T markings. The new nipple-areolar complex position is located at the level of the inframammary fold. The horizontal limbs extend to the apices of the inframammary fold.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|