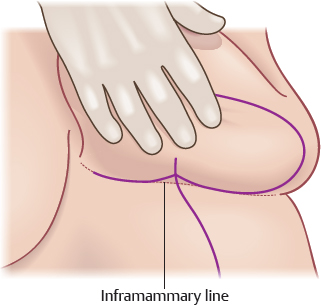
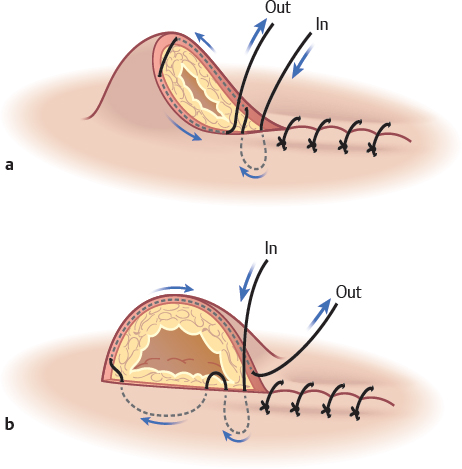
CHAPTER Macromastia can cause significant physical and psychological detriment, negatively impacting women’s daily functional capacity. Physical manifestations of breast hypertrophy can include back, neck, and shoulder pain; intertrigo; and shoulder grooving from brassiere straps.1 Surveys demonstrate a satisfaction rate of more than 95% after reduction mammaplasty. Most patients report an improved quality of life, self-esteem, and satisfaction with the surgery. This is regardless of the amount of tissue removed during the operation or the patient’s preoperative body mass index (BMI).2 The surgery can positively affect a patient’s mental state and be a stimulus for increased postoperative exercise and weight loss.1,3 According to the Cosmetic Surgery National Data Bank, breast reductions were the eighth most common cosmetic surgery performed in the United States in 2014, with a total of 114,170 surgeries completed.4 Although reduction mammaplasty is one of the most commonly performed procedures in plastic surgery and has a low rate of serious complications, the surgeon should be mindful of the minor to more significant complications that can arise and ways to potentially avoid, identify, and treat them when necessary. Disclaimers: The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. government. Dr. Yan Ortiz-Pomales is a military service member (or employee of the U.S. government). This work was prepared as part of his official duties. Title 17, USC, x105 provides that “Copyright protection under this title is not available for any work of the U.S. Government.” Title 17, USC, x101 defines a U.S. government work as a work prepared by a military service member or employee of the U.S. government as part of that person’s official duties. Summary Box Complications in Reduction Mammaplasty • Seromas and hematomas • Wound-healing issues and scars • Dog ears • Epidermal inclusion cysts • Asymmetry or recurrent macromastia • Nipple–areola complex congestion • Infection • Unplanned readmission because of pain, nausea and vomiting, dizziness, or bleeding Patient satisfaction is largely dependent on setting appropriate expectations in the preoperative evaluation. The following risk factors and their effects on surgical outcomes must be discussed with patients before reduction mammaplasty. Patients should be informed that the overall complication rate 6 months after surgery is approximately 19% and that 9% of patients require operative intervention or revision.5 This is regardless of the surgical technique used. Complications are most common within the first 30 days after the procedure.5 The patient must be informed that the perioperative complication rate is doubled in smokers. The surgeon should document whether the patient is a current or previous smoker. If the patient is a current smoker the surgeon should discuss cessation techniques and provide resources. The surgeon should also consider a less-aggressive dissection if the patient uses tobacco, because tobacco use increases infection risk (odds ratio [OR] 2.1; p = 0.008).6,7 Some surgeons will not perform the operation if the patient is an active smoker; nicotine urine testing can be used as confirmation of cessation. Chan et al8 found that wound-healing problems showed statistical significance (p < 0.05) between smokers (55.4%) and nonsmokers (33.7%). Seventy-five percent of smokers admitted denying smoking within 4 weeks of the operation. Wound healing complications are present in 33.3% of patients if they have stopped smoking for more than 4 weeks, 52.6% of patients if they stopped smoking less than 4 weeks before the operation, and 67.7% of are active smokers.8 A BMI of 35 kg/m2 or higher increases the risk of infections (OR 2.3; p = 0.00), seromas (OR 2.9; p = 0.03), fat necrosis (OR 2.0; p = 0.002), and minor wounds (OR 1.7; p = 0.001).6 Massive weight loss over a short amount of time can make surgical planning more complex. An unstable breast mound coupled with inelastic skin may require special techniques for glandular reshaping to achieve more lasting results.9 Cardiac disease increases the risk of fat necrosis (OR 5.3; p = 0.3) and the need of reoperation for scar revision (OR 3.0; p = 0.04).6 Independent factors associated with wound dehiscence are tobacco and steroid use, wound classification at the end of the case, postoperative abscess development, deep surgical-site infection, increased BMI, and paraplegia or quadriplegia.10 A study by Manahan et al6 showed that age greater than 50 years confers increased risk for infection (OR 2.7; p = 0.03). However, a recent study by the American College of Surgeons National Surgical Quality Improvement Program10 found that in regards to plastic surgery procedures, age does not confer an increased risk of wound-healing complications. This retrospective review revealed that otherwise healthy, elderly patients and younger patients have the same risk of developing wound dehiscence.10 Aging does cause a temporary delay in the healing process, but it does not impair the quality of the final scar. In regards to final scar appearance, elderly patients, in fact, tend to have an improved scar appearance. This is presumed to be a result of a reduced healing and inflammatory reaction, and thus a decreased risk for hypertrophic scars or keloids.10 Reduction mammaplasty is the most effective form of treatment of mammary hypertrophy in the adolescent population. Appropriate patient selection, however, is of paramount importance. Adolescents ( younger than 18 years of age) with macromastia can experience the same detrimental emotional and physical symptoms as adults with the condition. In addition, the psychosocial impact at this young age can have lasting psychological consequences. Physical symptoms and not aesthetic considerations should be the major deciding factor in whether to proceed with surgery.11 Conditions associated with adolescent breast hypertrophy include juvenile gigantomastia, adolescent macromastia, and obesity-related breast hypertrophy. Juvenile gigantomastia generally involves an extremely rapid growth ( approximately 6 months) of breast connective tissue during puberty, sometimes occurring with the onset of thelarche.11 After the initial rapid growth, patients then experience continued growth at a slower rate. Adolescent macromastia can be equally distressing to the patient but involves a less severe and more sustained steady breast growth.11 Adolescent patients can also have obesity-related breast hypertrophy, which is often difficult to distinguish from adolescent macromastia. Obesity should not be an absolute contraindication to adolescent breast reduction surgery. A study by Webb et al12 reveals favorable results and high satisfaction rates in both obese and nonobese patients. Patients report improved self–body image and increased participation in social activities and sports postoperatively.11 In addition to a comprehensive clinical assessment and determining a patient’s degree of debilitation, strong parental and family support and stability of breast size for 6 months to 1 year should be considerations before operative intervention.11 A thorough history must be obtained from the patient regarding prior biopsies, presence of masses, and date of last mammogram. There is no evidence-based data to confirm the benefit of unique screening protocols for women undergoing reduction mammaplasty. The official recommendations by the American Cancer Society, the American College of Surgeons, and the American Congress of Obstetricians and Gynecologists are that average-risk women begin obtaining annual screening mammography at 40 years of age. Among women younger than 40 years, the evidence supports screening mammography only for those who have a high risk for breast cancer.13 It is generally recommended to obtain a mammogram 6 to 12 months after surgery to reestablish baseline findings on surgically altered breasts.14 In appropriately selected patients with breast cancer, tumor resection with oncoplastic reduction (versus tumor resection alone) has been shown to result in fewer positive margins on pathologic analysis and a decreased need for reexcision.15 This is likely a result of the ability to take generous resection margins at the time of surgery. The plastic surgeon can work alongside the general surgeon or oncologic breast surgeon to not only obtain substantial margins at the tumor site but also improve overall cosmesis.15 Although complications occur, they have not been found to affect the initiation of adjuvant cancer therapy and are often managed conservatively. Clinical features of anxiety and depression are present in one third of women presenting with macromastia. Eating disorders are also common. These conditions alone should not preclude a patient from having a reduction mammaplasty operation. In fact, anxiety and depression rates decline in a large proportion of patients postoperatively, and patients experience improvements in self-esteem. In addition, eating behaviors as measured by the Eating Attitudes Test have shown a trend toward improved eating habits postoperatively.3,12 Reduction mammaplasty can potentially interfere with breast-feeding or the ability to produce an adequate milk volume.16–18 In a study by Makki and Ghanem,18 31% of 164 women who underwent a reduction mammaplasty with an average of 1,037 g excised from each breast reported decreased nipple sensation. In this same study, 31 out of the 36 women who became pregnant after the operation reported successful breast-feeding.18 In a cohort of seventy-eight women who underwent an inferior pedicle reduction mammaplasty, Brzozowski et al17 found that 53% did not attempt lactation postoperatively, 18% were unsuccessful, 19% exclusively breast-fed, and 10% used a combination of breast-feeding and supplemental formula. Some of these women were discouraged to breast-feed by health care workers for unknown reasons. Women who undergo reduction mammaplasty should be encouraged to breast-feed according to World Health Organization (WHO) guidelines.19 A meta-analysis of antibiotic prophylaxis in breast reduction surgery by Shortt et al20 demonstrated a 75% reduction in wound infections with the use of preoperative antibiotics (OR 0.25; 95% confidence interval [CI] 0.09–0.72). Breast surgery is classically described as a “clean” operation with an infection rate of less than 3.4%, but the use of preoperative antibiotics helps to further decrease infection rates postoperatively.21 Deep vein thrombosis (DVT) and pulmonary embolism (PE) can be devastating and potentially life-threatening complications. The American Society of Plastic Surgeons Venous Thromboembolism (VTE) Task Force uses patient risk stratification scores to help identify patients at high risk for DVT through the 2010 Caprini Risk Assessment Model.22 Important patient-related factors that have been found to increase the risk for DVT/PE include a positive cancer history, the use of oral contraceptive pills, hormone therapy, or having a bleeding disorder such as factor V Leiden deficiency. A score of 4 to 5 indicates a patient is at increased risk for DVT. A patient with a score greater than 8 has a very high risk of venous thromboembolism.23 Decreased venous return and venous pooling during induction of general anesthesia make clot formation the most likely intraoperatively. The surgeon should consider giving high-risk patients chemoprophylaxis preoperatively. Most studies show no increased bleeding risk postoperatively when chemoprophylaxis is used appropriately.23,24 Over a 10-year period involving 720 patients, Lapid et al24 found that 5.1% of patients undergoing reduction mammaplasty who had preoperative and postoperative administration of low-molecular-weight heparin (LMWH) for DVT/VTE prophylaxis required reoperation for hematoma.24 Of note, none of these patients had a documented complication associated with DVT or VTE. Their study concluded that the risk of potential hematoma development with administration of LMWH prophylaxis outweighs the morbidity and mortality associated with DVT/VTE.24 Mechanical prophylaxis through the use of stockings or sequential compression devices (SCDs) increases tissue plasminogen activator and stimulates fibrinolytic activity. SCDs should be applied approximately 30 minutes before induction and continued until the patient is ambulatory again after surgery.23 Epinephrine infiltration intraoperatively (with hydrodissection), before reduction mammaplasty, has been shown to decrease intraoperative blood loss and reduce the need for blood transfusion.25 After the induction of general anesthesia, 60 mL of a solution containing 25 mL of 1% lidocaine with 1:100,000 epinephrine is infiltrated into the skin and subcutaneous tissues along the outlined sites of incision.26 The solution is also infiltrated into the surrounding breast tissue itself. The benefit is twofold: (1) Lidocaine in the solution provides local anesthesia while (2) epinephrine, as a vasoconstrictor, helps to minimize intraoperative blood loss.26 A blood loss difference of approximately 109 to 200 mL has been demonstrated with the use of the hydrodissection technique.25,26 Care should be taken to avoid excessive tension on the incisions to decrease hypertrophic scarring.9 If possible, incisions should be made parallel to natural skin creases (Langer’s lines).27 The three most common reduction mammaplasty-associated scar patterns include the inverted-T scar (Wise pattern), vertical scar, and the “no vertical scar” technique (horizontal breast reduction) (Video 36.1).28 The operative technique should be based on the surgeon’s comfort level and appropriate method, taking into account the patient’s breast size and shape. The inverted-T scar is the most widely used technique because of its versatility. Periareolar, horizontal, and vertical scars are associated with the Wise pattern. The vertical technique includes a periareolar and vertical scar; however, it has a high rate of revision.28 The horizontal breast reduction technique is well-suited for breasts with significant ptosis but can be challenging in extremely heavy-breasted women. Periareolar and horizontal scars are associated with the horizontal breast reduction. A prospective analysis comparing patient preferences in regard to the three most common reduction mammaplasty scar patterns demonstrated that mean preference ranking was significantly higher for the horizontal scar pattern versus vertical and Wise patterns (p < 0.001).28 One method to potentially decrease tension, scarring, and wound dehiscence involves incorporating inframammary darting, in which a small triangular section of excess tissue is left projecting along the mid-inframammary line to decrease tension at the future “T-junction” site closure.26 The height of the triangle nears 0.5 cm and has an angle of 120 degrees. The base of the triangle lies on the inframammary line, and each side limb of the triangle is approximately 1 cm long26 (Fig. 36.1). Care is taken to minimize upward projection of the triangle wedge to prevent superior displacement of the nipple.26 Fig. 36.1 The incorporation of inframammary darting along the mid-inframammary line to minimize tension at the future site of closure. “Dog-ears,” excess tissue at the ends of a wound that give an out-pouched appearance, can result from closure of a circular or asymmetrical wound. Dog-ears can have two shapes—standing full-cone (excess tissue on bilateral sides) or lying half-cone (excess tissue on a single side).29 The inverted-T scar (Wise pattern) and horizontal techniques have the potential for dog-ears.28 A novel suturing technique helps to decrease the appearance of dog-ears without extending the incision. When the dog-ear is encountered, a three-bite absorbable suture is placed between the deep plane and the dog-ear skin margins. The deep fascial plane is pierced by the first bite along the skin suture axis (a few millimeters distal to the last cutaneous stitch). The second bite pierces the dermis in one dog-ear’s margin in a subcuticular fashion (entering at the level of the deep bite exit and coming out 2 mm proximal to the apex of the dog-ear. The third bite is carried out in a subcuticular fashion in the other dog-ear’s margin and is symmetrical to the second one. The suture is then tied, focusing on avoiding any purse-string effect. This technique helps to flatten the dog-ear and anchor the projecting tissue to the deep fascial plane29 (Fig. 36.2). When there is excess tissue on a single side (asymmetrical dog-ear), the first bite is the same as previously described (pierces the deep fascial plane along the skin suture axis a few millimeters distal to the last cutaneous stitch). The second bite pierces the dermis in the flat skin edge and runs in the dermis along a large bite in a subcuticular fashion and comes out 2 mm proximal to the apex of the skin incision. The third bite is again carried out in a subcuticular manner along the whole dog-ear’s margin, with the entry and exit sites symmetrical to the opposite skin margin. This suture is then tied down while evenly distributing the tension29 (see Fig. 36.2). Other described techniques include straight excision with scar lengthening, Burow’s triangle, hockey stick or right-angle excision, M-plasty, S-plasty, V-Y advancement flap, or triangular advancement flap.29 Nipple–areolar complex (NAC) venous congestion can be caused by inadequate preservation of venous drainage, pedicle constriction, or hematoma formation. Other risk factors include a history of diabetes mellitus, obesity, or tobacco abuse.30,31 NAC venous congestion can lead to NAC necrosis or conversion to a free nipple graft that can reduce lactation ability and sensation viability. Lewin and colleagues’ retrospective analysis31 on 512 patients revealed 3.1% of patients had partial areola necrosis and 0.6% of patients had total areola necrosis within 30 days after reduction mammaplasty.31 Diabetic patients had a notably increased risk of areola necrosis (OR 8.2; 95% CI 2.1–32.34, p = 0.003). Larger reduction weights and increased suprasternal notch–to–nipple distance have also been correlated with increased risk for NAC congestion or compromise (OR 1.8; 95% CI 1.20–1.60, p < 0.001).30,31 An increased notch-to-nipple distance indicates a longer dermoglandular pedicle. This reflects a more tenuous blood supply to the NAC given the distance required for perfusion.31 A superiorly-based dermoglandular flap might not be the optimal operative technique when faced with a long suprasternal notch-to-nipple distance.31 Fig. 36.2 Two different patterns of dog-ear correction. (a) The three-bite technique applied on the standing full-cone dog-ear. (b) The three-bit technique applied on the lying half-cone dog-ear. (Modified from Jaber O, Vischio M, Faga A, et al. The three-bite technique: a novel method of dog ear correction. Arch Plast Surg 2015;42[2]:223–225.) In cadaveric studies superomedial, medial, and inferior pedicle techniques have been shown to be the most reliable to have consistent venous drainage. If NAC is noted intraoperatively, the surgeon should evaluate for tight sutures that could be released, confirm there are no kinks on the pedicle, or do an exploration for hematoma evacuation.31 Promising new technologies, such as the SPY Elite Intraoperative Perfusion Assessment System (LifeCell Corporation) can provide the surgeon with real-time perfusion information. This is helpful because the surgeon can immediately resect skin or fat in the operating room if there is evidence of skin or fat necrosis.32 Also, if an extremely large reduction is being performed and the keyhole incision has not been made, perfusion findings can help the surgeon decide between nipple preservation versus amputation. Unfortunately, in most cases when nipple perfusion is poor after repositioning, there is little hope for salvage other than loosely closing the incision.33 The use of topical nitroglycerin could also have a role in preventing permanent ischemic changes of the NAC, because it has been proven to decrease mastectomy flap loss in patients undergoing mastectomy and immediate reconstruction.33 A reduction mammaplasty in combination with a mastopexy may improve breast contour in patients with recent massive weight loss. Certain techniques such as parenchymal plication can act as an internal sling to reduce the risk for breast ptosis. Monofilament resorbable suture is placed into the gland or into the dermis. This is typically overcorrected to ensure settling into position. It may require releasing of the dermis once the skin is redraped to avoid tethering.9 Another surgical technique particularly helpful in this patient population involves dermal suspension. This secures the breast mound to the chest wall. Skin flaps are elevated and the glandular or deepithelialized tissue is secured to the chest wall with 0–0 braided permanent suture. The tissue can also be secured to the rib periosteum at the level of the third or fourth rib for better fixation. The level depends on the breast size and level of the inframammary fold. As always, nipple position is important to ensure appropriate shape and level of suspension. Placing the nipple too high is difficult to correct and should be avoided. Autoaugmentation is a surgical technique using local dermoglandular and fasciocutaneous flaps to improve breast contour and upper pole volume. Incorporation of perforators into the flaps, subdermal plexus preservation, and adherence to appropriate length-to-width ratios will allow reliable transfer with minimal potential for fat necrosis or flap loss.9 The surgeon should preserve superomedial breast tissue volume during glandular tissue resection to enhance medial fullness and the overall aesthetic result and to preserve blood flow from the second intercostal space perforator of the internal mammary artery.26 A retrospective review by Wrye and colleagues34 demonstrated no increased benefit to using closed suction drains for reduction mammaplasty. Their study mainly focused on the inferior pedicle technique. Many plastic surgeons still use drains, however, to prevent seroma and hematoma formation. Placing drains is the surgeon’s choice and should take into account individual patient factors. Seromas and hematomas are the most common postoperative complications from reduction mammaplasty. This is likely because of the large tissue dissections through nonanatomic planes.24 Seromas and hematomas can contribute to increased pain, infection risk, and wound-healing complications (Fig. 36.3). Gulcelik et al35 prospectively evaluated complications associated with 286 reduction mammaplasty procedures in patients with and without breast cancer. They found an approximately 5% risk for seroma and 2% risk for hematoma regardless of cancer status.35 Gulcelik’s study35 revealed that a BMI greater than 30 kg/m2 was associated with an increased risk of postoperative complications. Manahan et al6 found a higher incidence of complications related to a BMI greater than 35 kg/m. Although uncommon, seromas and hematomas may require secondary surgical procedures for evacuation. In patients who are at risk for increased postoperative drainage, surgical drains could help decrease the incidence of seromas and hematomas. Hypotension in the operating room decreases intraoperative blood loss but increases the risk of postoperative bleeding and hematoma development.24 Patients who have had superior and medially based pedicle reductions appear to be at higher risk for postoperative drainage and may benefit from drain placement at the initial time of operation. Postoperative drainage also directly correlates with the amount of tissue resected. If drains are placed, they should remain in place until output is less than 50 mL in a 24-hour period.36 Nonresolving seromas can often be aspirated in the surgeon’s office if necessary.37 Common complications after breast reduction surgery include wounds and scars. Fortunately, wounds often resolve with simple dressing changes or bedside débridement. Rarely, wounds require reoperation or negative pressure wound therapy. Anemia, vitamin B12 deficiency, low calcium, and decreased albumin levels can impair wound healing.9 Vitamin supplementation and nutritional support can help with the wound-healing process. It is best for a patient to go into surgery with an optimized nutritional status to decrease the risk for postoperative wound-healing complications. There is an approximate 2 to 3% occurrence of minor wound dehiscence postoperatively, and this is usually located at the T-junction areas.35 These areas are at most risk for ischemia, and therefore tight closure increases the risk of wound-healing complications postoperatively.35 Major wound dehiscence is more rare (less than 2%).34 Wound dehiscence can be partial (such as “T-junction” breakdown, most commonly) or total (requiring further operative procedures).35,38 For more serious wound-healing complications involving frank skin necrosis, débridement with split-thickness skin graft (STSG) has been successful (Fig. 36.4). Scars, as defined by the patient or physician as widened, hypertrophic, misshapen, misplaced, or asymmetrical, require revision in approximately half of cases.6 Excessive scarring can lead to patient dissatisfaction because of physical symptoms such as pruritus, stiffness, and tenderness. Patients are also usually unhappy with the unpleasant aesthetic outcome associated with excessive scarring. Psychosocial disturbance can cause the patient anxiety or decreased self-esteem.27 Cutaneous scarring has a broad spectrum of presentation. Scars can range from mature, flat linear scars to abnormally raised and hypertrophic scars. Keloids represent the most extreme manifestation of scarring and are divided into minor and major variants. Major keloids are large and raised (more than 0.5 cm) and may be painful and pruritic.27 Hypertrophic scars and keloids are distinct entities; hypertrophic scars stay within the boundaries of the original lesion, whereas keloids grow beyond the margins of the original wound.27 The patient should be notified that with time hypertrophic scars tend to settle or become less obvious.11 Conversely, keloids (minor and major) do not spontaneously regress and commonly recur after excision.
36
Reduction Mammaplasty
Avoiding Unfavorable Results and Complications in Reduction Mammaplasty
Preoperative Considerations
Tobacco Use
Obesity
Comorbidities
Increasing Age
Juvenile Population
Oncologic History
Oncoplastic Reduction
Psychological Disturbances
Breast-Feeding
Intraoperative Concerns
Antibiotics
Venous Thromboembolism
Blood Loss
Scar Prevention
Avoidance of Dog-Ears
Nipple–Areolar Complex Congestion
Breast Contour
Surgical Drains
Postoperative Complications and Treatment
Seromas and Hematomas
Wound Healing and Scars
Treatment of Scars
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine