Reconstruction of the Maxilla and Skull Base
Eric G. Halvorson
Duc T. Bui
Peter G. Cordeiro
RECONSTRUCTION OF MAXILLARY DEFECTS
The maxilla is an essential component of the midface and has both functional and aesthetic roles. It contributes to facial appearance, determines midfacial width and height, and serves as support for the orbit, cheek, nose, and upper lip. The maxilla also supports critical functions such as mastication, speech, and deglutition. Most maxillary defects result from the surgical ablation of maxillary tumors or tumors arising from adjacent structures, including the paranasal sinuses, palate, nasal cavity, orbital contents, overlying skin, and intraoral cavity. Another cause of maxillary defects involves traumatic injuries resulting from gunshot wounds to the midface or less commonly blunt injury. Because of its close relationship to other facial components and unique three-dimensional structure, reconstruction of maxillary defects can be a formidable challenge for the reconstructive surgeon.
The goals of maxillary reconstruction are:
Reconstruct the orbital floor to maintain globe position or fill the orbital cavity following orbital exenteration
Reconstruct the intraoral, cheek, palatal, and nasal lining to restore speech, mastication, and oral continence
Separate the oral and nasal cavity from the skull base and orbit
Restore external skin and three-dimensional facial contour
Obliterate the maxillectomy defect
Traditionally, prosthetic appliances were used to reconstruct maxillary defects and are still a reasonable option in some patients (see Chapter 38). This method of reconstruction relies on adequate support from the remaining tissues and split-thickness skin grafting to line the defect. Despite successes in many cases, there are several disadvantages to the use of obturators. Leakage and oronasal regurgitation because of bulky dentures, inadequate dentition, and poor retentive surfaces, the need for cleaning, and repeated prosthetic refinements are common problems.
Autologous tissue is frequently preferable. Small defects of the maxilla can be reconstructed with local soft-tissue flaps with or without supplemental bone grafting. Prior to the advent of free tissue transfer, larger maxillary defects were repaired with a variety of pedicled flaps, including the deltopectoral, pectoralis major, latissimus dorsi, temporalis, sternomastoid, and trapezius myocutaneous flaps. These flaps were limited by their reach without tension on the vascular pedicle, circulatory compromise at the distal (and often most critical) portion of the flap, inadequate tissue to fill the defect, and/or the requirement for multiple stages to achieve a final result. More recently, microvascular free tissue transfer has significantly expanded the reconstructive surgeon’s armamentarium for maxillary reconstruction. There are many composite flaps that can be transferred to the midface without limitations of vascular pedicle length or flap geometry. Flaps can be chosen based on the precise tissue, volume, and surface area requirements of each defect.
Although free flap reconstruction now is the preferred method for the vast majority of extensive maxillary defects, flap selection is somewhat complex. The initial step is to define the maxillary defect in terms of bony and soft-tissue components. Adjacent critical structures, such as the eye, nose, and lips, are assessed. A history of radiotherapy or previous neck dissection is noted. The necessary length of the vascular pedicle and donor-site morbidity are assessed. The amount, location, and quality of residual bone, dentition, and denture-bearing alveolar arch largely determine whether a bone-containing flap is necessary.
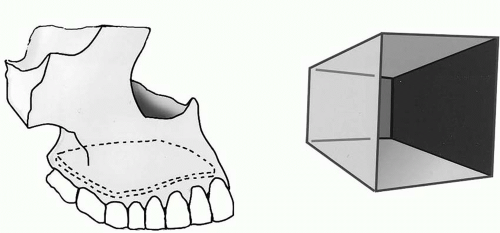
Visualizing the maxilla as a six-sided box with the roof being the orbital floor and the floor being the palate is helpful in determining which walls are missing (Figure 39.1). The three walls that require reconstruction are the superior (orbital floor), floor (palatal), and anterior (cheek) walls. Reconstruction of the highly complex three-dimensional nature of the maxillary defect can be simplified by combining bone grafts with a soft-tissue flap. Bone grafts can be rigidly fixed without interfering with flap inset. Vascularized bone is essential only in the maxillary arch, and possibly to replace a vertical buttress if both are resected. Although a variety of alloplastic products are available for bone replacement, these are not indicated in patients who have either received or will receive radiation therapy, and in general do not perform as well as autologous grafts.
Bone replacement for the orbital floor is essential to maintain globe position. The orbital floor can be reconstructed with autologous bone grafts because this area requires minimal supportive strength. The maxillary arch of the midface is reconstructed to provide anterior projection and dental support. Ideally, bony replacement of the maxillary arch must have adequate bone stock for osseointegrated dental implants. Hence, vascularized bone is required for reconstructing the maxillary arch. The palate can be repaired with the skin island of a free flap or replaced with an obturator. The anterior wall of the hypothetical box requires reconstruction but does not require bony reconstruction. The maxillary sinus in the center of the hexahedron can be filled with soft tissue (muscle or fat). The nasal lining may or may not be restored, and if the only remnant following extirpation is the septal mucosa, one option is to elevate the mucosa off the septum, fold it back, and suture it to the posterior nasal airway remnant to close off and obliterate the nasal airway on that side.
One difficulty in midface reconstruction with free flaps is that the closest recipient vessels are in the ipsilateral neck. The ideal free flap, therefore, must have a pedicle length of 10 to 13 cm to reach the neck without vein grafting. Although a variety of free flaps, including fibula, scapula, anterolateral thigh, and iliac crest flaps, can be used to reconstruct maxillary defects, the two flaps most commonly used that have large and long pedicles are the rectus abdominis myocutaneous and radial forearm flaps. The rectus flap provides reliable skin and a large soft-tissue bulk. The radial forearm flap provides a large surface area of pliable skin with minimal soft tissue and can be combined with a vascularized bone segment. Both flaps can provide multiple skin islands that can be oriented in different three-dimensional positions.
Many classification systems have been developed to describe the extent of resection of maxillary and midfacial tumors and to provide algorithms for reconstruction. A simple classification system we have previously described is presented below.
Classification System for Maxillary and Midfacial Defects
Type I (limited maxillary) defects involve resection of one or two walls of the maxilla, excluding the palate (Figure 39.2). These defects usually include the anterior and medial walls of the maxilla, and occasionally the orbital rim, in combination with the soft tissues and skin of the face. Hence, the defect has a high surface-area-to-volume ratio. The radial forearm flap is an ideal flap because it has a good surface-area-to-volume ratio, that is, it consists of a small amount of soft-tissue volume and large skin surface area. Defects of the orbital rim or orbital floor are reconstructed with split-calvarial or rib bone grafts. Other thin flaps with a high surface-area-to-volume ratio include the scapular, parascapular, and anterolateral thigh fasciocutaneous flaps, depending on the patient’s body habitus. Our preference for the radial forearm flap is due to the reliability of the anatomy, the length and caliber of the pedicle, and the consistently thin and pliable tissue.
Type II (subtotal maxillary) defects include resection of the maxillary arch, palate, and anterior and lateral walls with preservation of the orbital floor. These defects have recently been subdivided into type IIA defects that involve resection of less than 50% of the palate and type IIB defects that involve greater than 50% of the palate (Figure 39.3). Resection of these defects includes the classic hemimaxillectomy, or “infrastructure maxillectomy,” that involves most of the lower five walls of the maxilla with a medium surface-area-to-volume ratio (large surface area and medium volume). Both type IIA and type IIB maxillectomy defects are moderate-volume deficiencies with large surface area requirements, which usually require two skin islands.
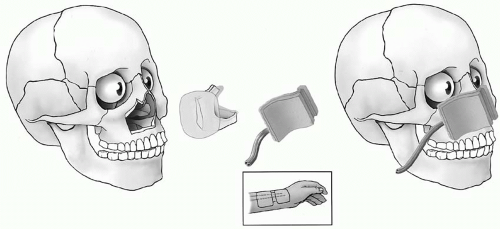
For type IIA defects, reconstruction may involve either a free flap or a combination of a skin graft and an obturator, depending on the patient and the surgeon preference. If a free flap is selected to avoid the inconvenience and maintenance of a palatal obturator, our flap of choice is the radial forearm fasciocutaneous free flap. To keep the soft palate taut, recreate the buccal sulcus, and to avoid prolapse into the oral cavity the skin paddle must be equal to or smaller than the original defect. If adequate teeth or bone stock remain, dentures or osseointegrated dental implants are used. Smaller type II defects or defects in patients who are not free flap candidates can be reconstructed with a temporalis muscle flap (Figure 39.4).
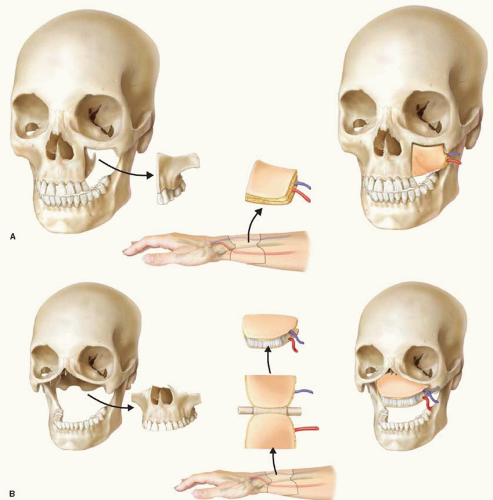
An osteocutaneous radial forearm flap folded into a “sandwich” is ideal for reconstruction of type IIB defects that by definition include much of the maxillary arch and hard palate. This technique provides anterior projection and vascularized bone for dental implant osseointegration. Additionally, the bone provides support for the upper lip. The folded skin surfaces restore the palatal mucosal lining and nasal floor lining. This flap has a “moderate” amount of volume when folded over and still maintains an adequate surface area to resurface the nasal floor and palate. Anterior bilateral subtotal maxillary defects are ideally suited for an osteocutaneous sandwich flap. Patients with these defects and intact upper external lip structures can be reconstructed with excellent aesthetic and functional results (Figure 39.5). Other options for reconstruction of type IIB defects include the scapula and fibula osseocutaneous flaps. The scapula flap has more tenuous blood supply, does not tolerate multiple osteotomies, and requires repositioning the patient preventing a two-team approach. The fibula flap supplies abundant well-vascularized bone that can tolerate multiple osteotomies. We have found, however, that maxillary arch defects do not require more bone than the radial forearm fasciocutaneous flap provides, that the fibula bone can be bulky in the maxilla, and that the fibula flap
pedicle is not as long as that of the forearm flap. In addition, the leg skin is often bulkier than the forearm skin, making inset more difficult and secondary procedures more likely.
pedicle is not as long as that of the forearm flap. In addition, the leg skin is often bulkier than the forearm skin, making inset more difficult and secondary procedures more likely.
Type III (total maxillary) defects include resection of all six walls of the maxilla. This type of defect is further subdivided into type IIIA, where the orbital contents are preserved and orbital floor is resected (Figure 39.6), and type IIIB, which is a total maxillary defect combined with orbital exenteration (Figure 39.7).
Type IIIA defects have medium-large volume and mediumlarge surface area requirements. Reconstruction of the orbital floor is required to maintain a functional eye. The floor is restored with nonvascularized bone graft, which must be supported by a well-vascularized flap. The rectus abdominis flap provides muscle coverage for bone grafts and adequate subcutaneous fat that can be contoured to fill the dead space. It can provide multiple skin islands for the palate and/or external skin and/or nasal lining as needed. A temporalis muscle flap can also cover the bone grafts for the orbital floor; however, it may not replace the palate. Consequently, an obturator may be required for palate reconstruction. Temporalis flaps are indicated in older patients who are not candidates for free
tissue transfer. Preservation of the malar eminence is helpful to maintain upper midface projection. Primary bone grafting in this area can be challenging because it can compress the flap pedicle. Another option for reconstruction of type IIIA defects is the fibula flap, as it can be used to reconstruct the orbital floor, vertical buttresses, and alveolar ridge. Muscle and/or skin taken with the flap can be used to fill dead space and provide lining. Disadvantages include a shorter pedicle length and higher complexity; however, it is an option when dental restoration is desired.
tissue transfer. Preservation of the malar eminence is helpful to maintain upper midface projection. Primary bone grafting in this area can be challenging because it can compress the flap pedicle. Another option for reconstruction of type IIIA defects is the fibula flap, as it can be used to reconstruct the orbital floor, vertical buttresses, and alveolar ridge. Muscle and/or skin taken with the flap can be used to fill dead space and provide lining. Disadvantages include a shorter pedicle length and higher complexity; however, it is an option when dental restoration is desired.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree