Reconstruction of the Forefoot
Rachel Hein
Scott T. Hollenbeck
DEFINITION
The primary goal in forefoot reconstruction is to preserve function of the lower extremity. Given the unique bony and skin arrangements in the foot as well as the high functional demand for this area, an understanding of multiple reconstructive approaches is necessary.
ANATOMY
The forefoot contains the distal third of the foot from the base of the metatarsals to the distal phalanges of the toes on both the plantar and dorsal surfaces of the foot.
The plantar surface of the foot has highly specialized glabrous skin with a thick epidermis. Beneath the skin and subcutaneous tissue is the plantar aponeurosis, which is a thick fibrous band adherent to the skin. This resists shearing forces as it attaches to the skin via the retinaculum cutis ligaments distal to the metatarsals. In contrast, the dorsal skin of the forefoot is extremely thin and relatively mobile.
The bones of the forefoot are somewhat analogous to the hand with the first toe containing only a distal and proximal phalanx. The second through the fifth toes have a middle phalanx. There are five metatarsal bones, which span from the midfoot bones (cuneiforms and cuboid) to the proximal phalanx of each digit.
There are four separate plantar fascia compartments and one dorsal fascial compartment that are divided by intermuscular septa. These separate the intrinsic muscles of the foot.
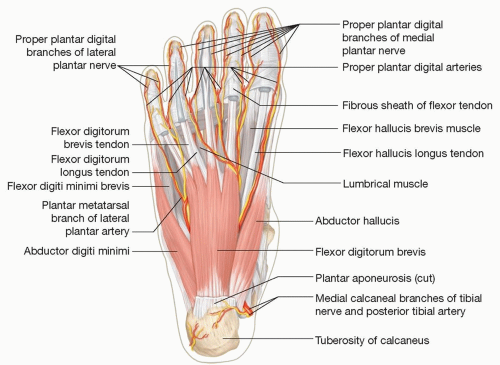
The medial and lateral compartments are the most relevant for reconstruction as the muscles are most superficial and amenable to flap use. Of note, the medial compartment contains the abductor hallucis (AH) and flexor hallucis brevis (FHB) whereas the lateral compartment contains the abductor digiti minimi (ADM) (FIG 1).
There are extrinsic and intrinsic muscles of the foot.
The extrinsic muscles originate in the leg and insert onto the bones of the foot.
The peroneus tendons insert onto the 5th metatarsal and allow for foot eversion.
The extensor digitorum longus (EDL) tendons insert onto an extensor mechanism of each of the lateral four digits.
The extensor hallucis longus (EHL) tendon has its own muscular unit and inserts onto the first phalanx.
In addition to the digit extending muscles, the foot may be brought into extension by the tibialis anterior (TA), which inserts onto the medial cuneiform/first metatarsal junction.
Preservation of at least one of these three systems is needed to prevent a functional footdrop. The digital flexors have a similar arrangement to the extensors, with the flexor digitorum longus (FDL) inserting onto each of the lateral four digits and the flexor hallucis longus (FHL) tendon inserting onto the first toe.
Plantar flexion is primarily driven by the Achilles mechanism of the heel, but digit flexors do have some importance as it pertains to the toe push off phase of the gait cycle.
The intrinsic muscles are contained in the compartments of the foot and primarily act on the toes.
The flexor digitorum brevis (FDB) occupies the central aspect of the superficial muscles of the plantar surface of the foot. There are two additional deep layers of muscles in the plantar foot that are not commonly used in reconstructive surgery.
Secondary action of intrinsic muscles includes maintaining posture and foot concavity.
The dorsal aspect of the foot is primarily made up of the extrinsic tendons, deeper intrinsic digit extensors, and still deeper interosseous muscles.
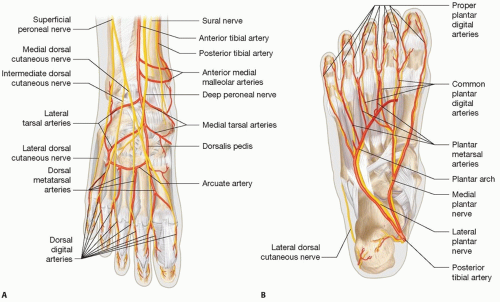
The main vascular supply to the foot comes from the posterior tibial artery. The artery splits into the medial and lateral plantar arteries beneath the flexor retinaculum. These two arteries join at the base of the metatarsals to form the deep plantar arch.
The lateral plantar artery is the dominant artery supplying the fourth and fifth toes through metatarsal and then proper digital arteries.
The medial artery supplies the first through third toes in a similar fashion. The dorsalis pedis artery supplies the dorsum of the foot and also gives terminal branches completing the plantar arch. For reconstructive purposes, the plantar intrinsic muscles of the foot are typically supplied via the medial and lateral plantar arteries (FIG 2).
Cutaneous sensation to the forefoot is supplied via terminal branches of the sciatic nerve. The plantar surface of the forefoot sensation is mainly derived from the medial plantar nerve (tibial origin) and the lateral plantar nerves (tibial origin).
The dorsal forefoot sensation is mainly derived from the superficial peroneal nerves (common peroneal origin) and the unique first web space distribution of the deep peroneal nerve (common peroneal, sciatic, L5 origin).
PATHOGENESIS
Traumatic foot injuries are typically associated with highenergy events. This may lead to extensive and complex wounds involving lacerations, contusions, skin degloving, open fractures, and severe crush injuries.
Cancerous lesions may require extensive surgical resection and reconstruction within the foot. Many of these are amenable to isolated digit or ray amputation but some may require large skin resections on weight-bearing areas of the foot.
Postsurgical complications following foot and ankle surgery may also present with complex problems involving necrotic skin, exposed tendons, colonized hardware and bony nonunion.
Chronic vascular disease including venous stasis and peripheral vascular disease can be a cause of tissue loss within the forefoot. This should mainly be addressed by controlling the inciting factor. Amputation and debridement are often needed in these cases prior to any consideration of reconstruction.
Diabetes is a major contributor to forefoot wounds and ulcers. Many of these patients have diabetic neuropathy and develop pressure-related ulcers over the metatarsal heads. Prior to consideration of reconstruction, the patient’s status should be optimized and nonsurgical options should be considered. This may include weight-bearing restrictions and/or use of shoe inserts to deflect pressure away from the affected area.2
NATURAL HISTORY
The lower extremity is commonly involved in motor vehicle injuries, and this is the most common scenario requiring forefoot reconstruction. These are often complex injuries and may involve multiple levels of the lower extremity and multiple systems within the patient. Standard principles of trauma care must be followed. Once the patient has been stabilized, foot reconstruction may involve a multidisciplinary limb salvage team including plastic and orthopedic surgeons.
A unique trauma scenario involving the forefoot is that related to lawn mower injuries and amputations. These are often isolated foot injuries but may be severe in nature.
Replantation of amputated digits is not typically performed in the lower extremity.
PATIENT HISTORY AND PHYSICAL FINDINGS
Gait cycle and biomechanics
Reconstructive surgeons managing wounds of the foot should be familiar with the gait cycle as it pertains to functional outcomes. Classically, there are three cycles of the stance phase of ambulation including heel strike, midstance, and propulsion. This is followed by the noncontact swing phase.
For the purpose of forefoot injuries, it is important to note that high pressures occur during propulsion and include the final contact point at the first toe. Higher pressures and abnormal gait may lead to skin breakdown and development of wounds over the forefoot.3
Evaluation of forefoot wounds
Initial evaluation of a patient with an acute traumatic injury to the foot includes assessment of the mechanism, energy, and contamination associated with the event. This often occurs during the initial washout and debridement of the wound. The associated soft tissue injury and underlying bony injury should be appreciated as well as the integrity of the vascular and neurologic systems within the foot.
Understanding a patient’s underlying comorbidities as well as preinjury functional status and work demands is also important.
Doppler examination is useful to determine arterial perfusion as well as planning for operative intervention. However, severe edema may prevent accurate Doppler assessment, and additional angiographic studies may be required. Any presumed acute arterial injury warrants a vascular surgery consultation and subsequent evaluation for compartment syndrome.4
Neurologic evaluation of the injured foot may be limited due to associated neuropraxia and tissue edema. Declaration of a nonsalvageable foot based on neurological injury should be deferred during the acute injury phase.
For chronic wounds, duration of wound and measurements should be taken including length, width, and depth. Involvement of skin, dermis, fascia, muscle, tendon, and bone should be noted as well as any concurrent cellulitis. Photographs should be taken, and previous therapies should be noted. Gait analysis is also important in these patients as disease processes can affect weight bearing over the forefoot. Vascular and neurological status is also important to take into account.
IMAGING
The physical exam will dictate the imaging studies needed when evaluating foot wounds. In the trauma setting, plain films are typically obtained first to rule out fractures. In some circumstances, a CT scan or MRI is obtained for better bony and ligamentous imaging. Angiography is typically reserved when evaluating more proximal injuries, but may be useful on certain occasions.
Chronic infectious wounds such as diabetic ulcers and postoperative wound breakdown require plain films to rule out pathologic fractures and gas in the subcutaneous tissues along with MRI to rule out osteomyelitis. Bone biopsies are the standard, but MRI may help delineate operative management in these cases. Ankle-brachial indices and duplex arteriogram should be obtained to assess arterial insufficiency and need for possible vascular intervention.
DIFFERENTIAL DIAGNOSIS
Traumatic
Postsurgical
Infectious
Diabetic
Acute arterial
Venous ulceration
Connective tissue disorder
NONOPERATIVE MANAGEMENT
Traditionally, dressing changes are helpful for managing small superficial wounds through healing by secondary intent. Negative pressure wound therapy (NPWT) may also be used to achieve secondary healing or to prepare a complex wound bed for a skin graft or flap.
Newer wound dressings have also aided in the treatment of open forefoot injuries including semipermeable dressings, hydrocolloids, and hydrogels. These new dressings can aid in chemical debridement as well as hydration of the wound.
Additionally, synthetic products and xenograft products exist and may have some utility in managing these wounds. More data are needed to prove the clinical efficacy of these treatments.
Hyperbaric oxygen (HBO) treatment may be used as an adjunct to traditional wound healing methods but remains somewhat unproven in its efficacy for foot wounds. HBO works by promoting angiogenesis and ultimately increasing the amount of vascularity in the wound bed, thereby promoting wound healing. It may be indicated in crush injuries, refractory osteomyelitis, and gas gangrene.
SURGICAL MANAGEMENT
Preoperative Planning
Debridement remains one of the most important preoperative principles in lower extremity salvage. For an acute wound, it is important to perform serial debridement if necessary until all nonviable tissue has been removed. Chronic wounds should be serially debrided until negative cultures are obtained. Comorbidities should be managed for optimization.
Once a decision has been made to proceed with reconstruction, the timing of intervention should be determined. Typically, this will be based on the underlying source of the wound.
In acute trauma settings, debridement and bony fixation should be complete. An understanding of vascular and nerve injury should be established. At this point, the extent of the reconstruction will be known and a proper approach may be determined.
The ideal window to operate on traumatic injuries is within the first week, if not sooner. Bacterial contamination and traumatic edema make reconstruction more difficult and warrant delay.
Positioning
A modification of standard supine positioning is required for most procedures. For plantar defects, it is often best to place the patient in a lateral decubitus or possibly prone position. Of course the positioning will be influenced by the planned reconstruction. A thigh or calf tourniquet is often used during these procedures to optimize visualization. Bipolar cautery should be available when procedures involve deep structures near the neurovascular bundles.
Approach
Reconstructive options for forefoot wounds include secondary closure, skin graft or skin substitute, local or random patterned flap, pedicled flap, or free flap with microvascular anastomosis.
Function and aesthetics must be taken into account. For example, a split-thickness skin graft to a wound bed is not likely to be a durable option for a plantar defect. Likewise, a large bulky flap placed on the dorsal forefoot is likely to make shoe fitting difficult. The specific approach for each reconstructive option is listed below.
Delayed primary closure is often difficult to perform secondary to refractory edema and minimal skin laxity of the foot.
Tissue expansion is often not an option for the same reasons listed above.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree