Defects of the nasal dorsum or sidewall can result from trauma, congenital lesions, extirpation of neoplasms, or iatrogenic injuries. Simple techniques are often used to reconstruct defects in this area with excellent outcomes. Complex defects require more sophisticated techniques including multilayer closures using pedicled flaps or free tissue transfer. This review discusses key anatomic and functional principles and techniques to assist in planning for reconstruction of nasal dorsum and sidewall defects from any cause.
Nasal dorsal and sidewall defects are often considered the least complex for nasal reconstruction. Defects in these regions may be repaired with simple techniques to produce excellent results. However, more complex defects, including full-thickness defects and those involving adjacent tissues such as the medial canthus, require thoughtful analysis and planning. Nasal defects should be analyzed with consideration of both aesthetic and functional concerns. Optimal reconstructive plans incorporate the concept of replacing like with like and strategic scar placement. Characteristics unique to the dorsum and nasal sidewall include the transitioning thickness of skin and soft tissues from the nasal dorsum to cheek, the close proximity to adjacent facial units (medial canthus, eye, cheek, and forehead) and the osseocartilaginous junction located in this region. Simple defects can be repaired with direct advancement of adjacent tissue, local flaps, or skin grafts to achieve acceptable results in this region. More complex defects may require transposition flap, interpolated flaps, or even free tissue transfer. This article addresses the multiple issues that must be considered for nasal dorsal and sidewall defect reconstruction.
Anatomy
Successful nasal reconstruction requires a thorough understanding of nasal anatomy, function, and cause of the defect being corrected. The nose functions to allow airflow and provide humidification and filtration of inspired air. The nose is a prominent facial feature and is integral to facial cosmesis, as it provides balance to the face because of its central location in both horizontal and vertical dimensions. The nose is divided into 3 layers, the mucosal lining, the osseocartilaginous framework, and the skin and soft-tissue coverage. Its surface is characterized by concave and convex curves and is divided into nasal subunits. The boundaries of the nose are the glabella superiorly, the nasofacial sulcus laterally as it transitions to the cheek, and the nasal vestibule and columella inferiorly. The nose is divided into 9 subunits: 3 unilateral structures (the dorsum, tip, columella) and 6 bilateral structures (the sidewalls, ala, and soft-tissue triangles) ( Fig. 1 ).
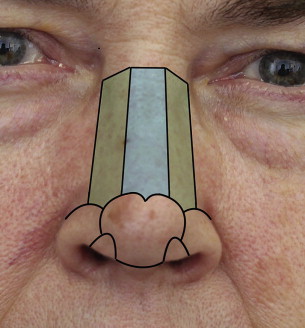
This discussion focuses on the nasal dorsum and sidewall units. From a frontal view, the dorsum of the ideal nose is symmetric and provides a gentle sweeping hourglass-shaped curve from the medial canthus to the nasal ala. The nasal dorsum contributes to nasal and midface projection from a lateral view. The nasofrontal angle defines the transition from nose to forehead and is ideally between 95° and 110°, but varies based on gender and facial harmony. The sidewall is located just lateral to the dorsum as the nose transitions to the cheek and the medial canthus adjacent to the eye.
It is important to understand the variations in the soft-tissue envelope characteristics that vary by individual skin types as well as by location. The soft-tissue envelope varies in thickness over the dorsum of the nose. The skin and subcutaneous tissue is thinnest at the rhinion, the osseocartilaginous junction, and is thicker more superiorly at the nasion and inferiorly at the nasal tip. The soft-tissue envelope thickens with lateral transition to the sidewall and cheek. Superiorly the tissues remain thin as the nose transitions to the adjacent medial canthus and eyelids. Reconstructive plans must consider the changing thickness of the soft-tissue envelope when repairing nasal dorsal and sidewall defects. For instance, when elevating the soft-tissue of the nose and cheek, the plane of dissection changes from below the superficial muscular aponeurotic system (sub-SMAS) plane over the nose to a subcutaneous plane over the cheek to avoid transferring thicker soft-tissue to the nose. Individual skin characteristics should be considered as well, when considering different types of closures. A classic example is the bilobe flap; thick sebaceous skin has a higher risk of developing flap necrosis, trap-door deformity, and depressed scars.
The internal nasal structure is critical and should not be neglected in planning for nasal reconstruction. Key portions of the osseocartilaginous structures of the nose are located within the nasal dorsum and sidewalls. The nasal bones, the upper lateral cartilages, and the keystone area, which is the junction of the bony cartilaginous septum and the nasal bones and upper lateral cartilages, are essential to proper nasal function. These structures provide shape to the nose and support to resist forces that collapse the nasal airway. The osseocartilagenous junction must be preserved during reconstruction. If this junction is disrupted during ablative surgery or as a result of trauma, efforts should be made to reconstruct and reinforce the support in this area to preserve nasal function.
The blood supply to the nose is based on the dorsal nasal artery superiorly and the angular artery from the facial artery inferiorly. The internal blood supply is based largely on the sphenopalatine artery. The venous drainage includes the facial venous and pterygoid plexus. The sensory innervation is from the infraorbital nerve of the maxillary branch of the trigeminal nerve and the sphenopalatine nerve. Motor innervation of the nose is through the facial nerve and muscles of facial expression. A thorough knowledge of the anatomy will assist the surgeon during flap elevation to ensure preservation of nasal blood supply, movement, and sensation.
Evaluation of nasal defects
Nasal defects can result from trauma, congenital lesions, extirpation of neoplasms, or iatrogenic injuries. Soft-tissue defects may be further classified as a wound, defect, or deformity. A wound is a disruption of parts and requires repair of the disrupted parts. A defect is a loss of parts and must be addressed by bringing in new parts to the defect. A deformity, which may be congenital or iatrogenic, is a distortion of parts and requires mobilization and repositioning of parts into proper alignment and relationships. This classification provides conceptual clarity and may be applied in developing a reconstructive plan based on the cause of the defect. A nasal dorsal laceration, skin excision, or scar deformity are 3 different lesions that require different reconstructive plans for successful repair.
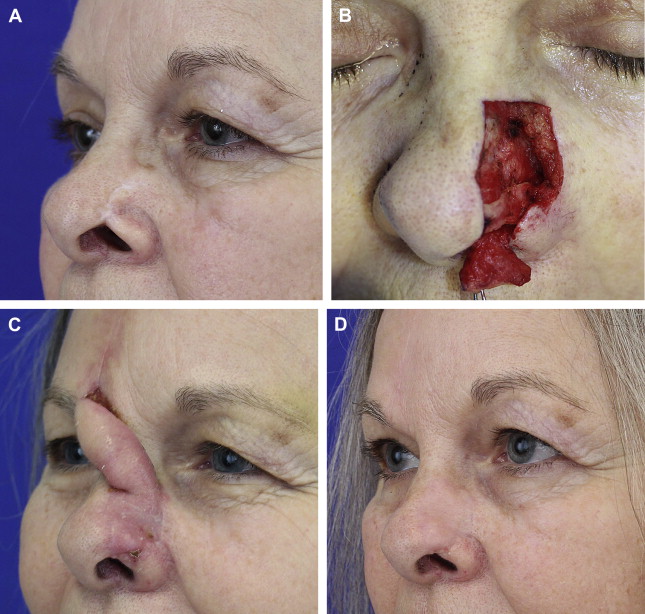
The size of the defect must also be considered. Park describes the classification of defects greater than 1.5 cm as large defects that are less likely to be successfully closed with local flaps and often require interpolated flaps for closure. Park also advocates enlarging the defect when more than 50% of a nasal subunit is involved by resecting the remaining residual subunit to have scars camouflaged within natural creases or at borders of 2 subunits to be more inconspicuous. This concept may also be applied to defects caused by a scar deformity such as the patient shown in Fig. 2 . This patient presented with a deformity of the alar rim causing airway obstruction after repair of a Mohs defect by a dermatologist. She also had a scar that extended into the central portion of the nasal sidewall subunit contributing to the deformity. A decision was made to resect the soft tissues of the nasal sidewall and place the incisions at the borders of the aesthetic subunits. A portion of the resected tissue was turned over to recreate the necessary internal lining for a full-thickness reconstruction of the contracted alar rim. The postoperative photo shows improvement at the alar rim but also a significant improvement at the sidewall where the central depressed scar was removed and less conspicuous scars are now located at the borders of the subunit.
One should also consider the reconstructive principle of replacing like with like. Depending on the size of the defect, donor tissue that adequately matches the complexity of the nose may be limited. Local tissue flaps provide similar tissue for reconstruction but may be limited by availability of sufficient tissue, donor morbidity, and scar formation. Generally, small to medium defects can be repaired by recruiting adjacent tissue. Larger defects may require a forehead or cheek flap, which tends to heal well and provide adequate tissue match. It is difficult to match tissue likeness with free tissue transfer to the external nose.
Evaluation of nasal defects
Nasal defects can result from trauma, congenital lesions, extirpation of neoplasms, or iatrogenic injuries. Soft-tissue defects may be further classified as a wound, defect, or deformity. A wound is a disruption of parts and requires repair of the disrupted parts. A defect is a loss of parts and must be addressed by bringing in new parts to the defect. A deformity, which may be congenital or iatrogenic, is a distortion of parts and requires mobilization and repositioning of parts into proper alignment and relationships. This classification provides conceptual clarity and may be applied in developing a reconstructive plan based on the cause of the defect. A nasal dorsal laceration, skin excision, or scar deformity are 3 different lesions that require different reconstructive plans for successful repair.
The size of the defect must also be considered. Park describes the classification of defects greater than 1.5 cm as large defects that are less likely to be successfully closed with local flaps and often require interpolated flaps for closure. Park also advocates enlarging the defect when more than 50% of a nasal subunit is involved by resecting the remaining residual subunit to have scars camouflaged within natural creases or at borders of 2 subunits to be more inconspicuous. This concept may also be applied to defects caused by a scar deformity such as the patient shown in Fig. 2 . This patient presented with a deformity of the alar rim causing airway obstruction after repair of a Mohs defect by a dermatologist. She also had a scar that extended into the central portion of the nasal sidewall subunit contributing to the deformity. A decision was made to resect the soft tissues of the nasal sidewall and place the incisions at the borders of the aesthetic subunits. A portion of the resected tissue was turned over to recreate the necessary internal lining for a full-thickness reconstruction of the contracted alar rim. The postoperative photo shows improvement at the alar rim but also a significant improvement at the sidewall where the central depressed scar was removed and less conspicuous scars are now located at the borders of the subunit.
One should also consider the reconstructive principle of replacing like with like. Depending on the size of the defect, donor tissue that adequately matches the complexity of the nose may be limited. Local tissue flaps provide similar tissue for reconstruction but may be limited by availability of sufficient tissue, donor morbidity, and scar formation. Generally, small to medium defects can be repaired by recruiting adjacent tissue. Larger defects may require a forehead or cheek flap, which tends to heal well and provide adequate tissue match. It is difficult to match tissue likeness with free tissue transfer to the external nose.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







