Reconstruction of the Cheeks
Babak J. Mehrara
The cheeks represent the largest surface area of the face and frame the central facial units. This anatomic arrangement exposes the skin of the cheek to trauma and to the effects of sun exposure, and, in turn, there is a frequent requirement for reconstructive surgery. Reconstruction must be planned carefully and executed meticulously to (1) restore the natural contours; (2) maintain hair patterns; and (3) camouflage scars.
The face can be divided into units based on a number of characteristics, including skin color, skin texture, hair, contour, relaxed skin tension lines, and boundaries between anatomic structures. The cheek, however, is less amenable to “aesthetic unit” analysis. Zide and Longaker1 divided the cheek into three overlapping zones: suborbital, preauricular, and buccomandibular based on reconstructive needs. Similarly, Jackson divided the cheek into five areas based on reconstructive techniques and anatomic characteristics (lateral, lower, malar, superomedial, and alar base-nasolabial).2 The classification systems are helpful for planning, but principles used for subunit reconstruction in other areas (e.g., resurfacing entire units, discarding remaining tissues of a subunit, and using the contralateral side to make exact templates) are less applicable to cheek reconstruction.
ANATOMY
The cheek is bounded by the preauricular crease laterally, the zygomatic arch and lower eyelids superiorly, the nasal sidewall and nasolabial fold medially, and the mandibular border inferiorly.
The sensory innervation of the cheek is provided by the maxillary and mandibular divisions of the trigeminal nerve, as well as a small contribution from the anterior cutaneous nerve of the neck and the great auricular nerve, both of which arise from the cervical plexus.
Motor innervation of the superficial facial muscles is provided by the facial nerve. The masseter and temporalis muscles (muscles of mastication) are innervated by the trigeminal nerve. In the preauricular area, the facial nerve is protected by the superficial lobe of the parotid gland and runs deep to the parotid masseteric fascia over the masseter muscle.
The arterial supply of the cheek is provided by branches of the external carotid artery, including the facial artery, the superficial temporal artery, and the transverse facial artery. Venous drainage follows the arteries and is abundant. The lymphatic drainage of the cheek is provided by lymphatic channels within the parotid nodes and along the facial vessels to the submandibular nodes.
DEFECT ANALYSIS
Analysis of the defect or anticipated defect is a critical part of any reconstructive procedure. Defects may be superficial (simple) and include only the skin and subcutaneous tissues, or may be more complex and include the muscle, parotid gland, facial nerve, mucosa, and bone. Ideally, surgical incisions are placed at the cheek margins or within established skin creases to camouflage the resulting scars. Care is taken to avoid, if possible, placement of hair-bearing skin into non-hair-bearing areas. Similarly, rotation of non-hair-bearing skin into areas of the male beard and distortion of the sideburn are avoided. Contour deformities and color mismatches are avoided when possible. Distortion of surrounding structures such as the lower eyelid and upper lip is disfiguring and is an important consideration in any reconstructive plan. According to Zide and colleagues, vertical incisions placed medial to a line drawn from the lateral canthus remain obvious on frontal view and ideally should be replaced by incisions along the nasolabial fold or by blepharoplasty incisions.3 Defects involving the full thickness of the cheek occur from invasion of skin cancers, from extensive trauma, or as a result of advanced intraoral cancers. Appropriate reconstruction of all layers, while maintaining reasonable contour, is planned if possible. A successful reconstruction will recreate the missing tissues using the most similar tissues. As with nasal reconstruction, plans for lining, support, and coverage are developed individually. Secondary revisions for contour may be necessary, particularly for complex reconstructions, and should be described to the patient prior to initiation of therapy.
Facial nerve reconstruction is ideally performed as a planned procedure, with the ends of the nerve stimulated and tagged at the time of resection since later identification of nerve ends is difficult and tedious. In addition, nerve transection is performed sharply to avoid cautery damage at the site of neurorrhaphy. Nerve grafts may be harvested from the neck (ansa cervicalis and great auricular nerve) or from distant sites (e.g., sural nerve).
For a given defect, more than one reconstructive option is usually available. The best option is determined based on the relationship of the defect to the surrounding structures, hairbearing status, skin laxity, natural wrinkles, previous surgical scars, relaxed skin tension lines, and avoidance of lower eyelid and lip distortion. Contaminated wounds undergo serial debridement and dressing changes until bacterial content is reduced to an acceptable level before definitive reconstruction is accomplished. Previous radiation therapy may prohibit local flap reconstruction.
RECONSTRUCTIVE OPTIONS
Healing by Secondary Intention
The simplest method of closure is healing by secondary intention. Unfortunately, the indications for this technique are limited as large wounds may result in contour irregularities, distortion of surrounding structures, and unstable coverage. This technique may be useful for small (<1 cm), superficial defects located in cosmetically inconspicuous areas (e.g., below the sideburns) in patients with solar-damaged, irregularly pigmented skin.
Primary Closure
Primary closure is the reconstructive method of choice if excessive tension and distortion of surrounding tissues can be avoided. The scars are ideally placed along minimal skin tension lines or within natural skin contours, such as the nasolabial or preauricular folds (Figure 35.1). This technique results in the simplest scar, avoids donor-site deformity, and avoids interpolation of distant tissues into the defect. The size of the defect suitable for primary closure is variable and depends on the amount of skin laxity present. Wide undermining in an elderly patient with significant skin laxity may allow closure of relatively large defects. Dog-ears created by wound closure should be excised while avoiding excessive lengthening of the
scar. The disadvantage of primary closure for larger defects is the long, straight scar in an area where there are normally no straight lines. The nonlinear scar from a local flap is preferable in many circumstances.
scar. The disadvantage of primary closure for larger defects is the long, straight scar in an area where there are normally no straight lines. The nonlinear scar from a local flap is preferable in many circumstances.
Skin Grafts
On rare occasions, skin grafts are useful for cheek reconstruction. Although skin grafts may be associated with shiny, patchlike, depressed scars, they may be reasonable in patients with significant comorbid conditions. Skin grafts have also been advocated by some authors in patients at high risk for local recurrence. In addition, skin grafts may be used to resurface less critical areas of the cheek (e.g., just below the sideburns), particularly when the defects are donor sites of flaps used to resurface more critical, medial areas. Full-thickness skin grafts exhibit less secondary contraction and should be used in situations where contracture would result in distortion of adjacent structures (e.g., lower eyelid). Full-thickness skin grafts have the additional advantage of better color match if harvested from the neck, preauricular/postauricular skin, or upper back. Full-thickness skin grafts are also thicker than split-thickness skin grafts and may be more useful for deeper defects. In general, excisions greater than 5 mm in thickness treated with skin grafts will likely exhibit a permanent contour deformity.
Local Flaps
Advancement Flaps.
Advancement flaps are useful for reconstruction of superomedial defects, particularly in elderly patients with significant skin laxity. These flaps may be performed as advancement flaps with excision of Burrow triangles or as V-Y advancements. Ideally, the lesion is excised as a rectangle or square to avoid trapdoor scarring. Advancement flaps are random pattern flaps raised in the subcutaneous plane and should be of appropriate width to avoid tip necrosis. A base-tolength ratio of 1:1 is usually safe. In addition, advancement flaps should be anchored to the periosteum of zygoma or maxilla at points higher than the lower eyelid to prevent ectropion.
V-Y advancement flaps are an excellent choice for closure of defects that lie along the medial cheek and alar base, particularly if primary closure of the defect results in distortion of the lower eyelid or nasal base (Figure 35.2).4 The excision is performed as a square or rectangle in the medial cheek or as a wide crescent at the alar base. Skin incisions are preformed to the subcutaneous tissues and the flap is advanced based on a subcutaneous blood supply. The length of the flap should be sufficient to avoid tension on the closure.
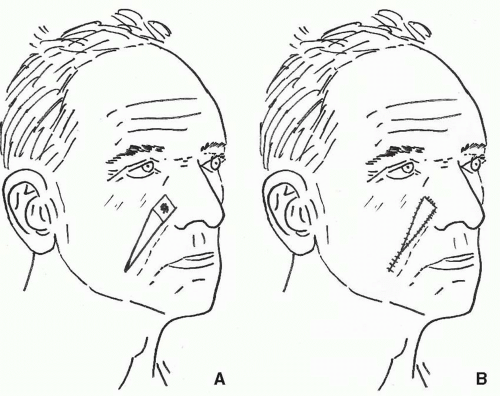 FIGURE 35.2. V-Y advancement flap to medial cheek defect. A. Flap design. B. After advancement. Note the advancement of nasolabial flap with rectangular excision of the defect. |
Zide and colleagues described the deep-plane cervicofacial “hike” repair as an advancement flap that removes dog-ears in a cosmetically acceptable blepharoplasty incision.3 The flap is dissected together with the SMAS (superficial musculoaponeurotic system), and the authors believe that it has a better blood supply than a subcutaneous flap. The dissection of the facial nerve is performed with blunt scissors, using vertical spreading, thus enabling advancement of the remaining cheek unit. Dog-ears are excised as an upper or lower blepharoplasty incision. Alternatively, the redundant upper eyelid skin may be used to reconstruct lower-lid defects, while the advancement flap is used to reconstruct the cheek defect (Figure 35.3).
Transposition Flaps.
Transposition flaps such as banner flaps, bilobed flaps, and rhomboid flaps are useful for most medium to large defects of the cheek and are designed to transfer lax skin while the donor sites are closed primarily. Although these flaps have some drawbacks (e.g., complex scars, pincushioning, trapdoor scarring, patchlike scarring,
and alterations in hair pattern), good results can be obtained in appropriately selected patients and with carefully designed flaps. Donor scars are planned carefully to fall, as much as possible, within relaxed skin tension lines or existing folds. Dog-ears are excised without narrowing the base of the flaps.
and alterations in hair pattern), good results can be obtained in appropriately selected patients and with carefully designed flaps. Donor scars are planned carefully to fall, as much as possible, within relaxed skin tension lines or existing folds. Dog-ears are excised without narrowing the base of the flaps.
Banner flaps are the simplest form of transposition flap and transfer the skin from the preauricular or nasolabial area to close the defect (Figure 35.4). Secondary revisions may be necessary to remove remaining dog-ears or to defat pincushioned flaps. Although these repairs usually have excellent contour and reasonable color match, the scars may be conspicuous, particularly with facial animation.
Bilobed flaps are an extension of the banner flap and use a secondary flap to close the defect created by the primary flap (Figure 35.5). Bilobed flaps are used when the defect created by the primary flap (i.e., the banner flap) is too large to close primarily. The flaps are designed on a 45° to 90° axis to the primary defect and are elevated in the subcutaneous plane. Generally, the primary flap may be drawn somewhat smaller than the defect and is designed, as much as possible, to place the scars along minimal tension lines and within natural skin creases. Flaps designed at 45° angles minimize dog-ear formation. The resultant scars are complex and may be quite conspicuous. Pincushioning is a problem with bilobed flaps, particularly relatively small flaps, and may require secondary revisions. Because of the laxity in the cheek, bilobed flaps are infrequently used on the cheek.
Rhomboid flaps are a geometric modification of banner flaps and are useful in the treatment of medium to large defects (Figure 35.6). These flaps are more difficult to design but have a decreased propensity for trapdoor scarring or pincushioning. Rhomboid flaps are useful primarily for lateral, lower cheek, and temporal defects. The excision is performed using a rhombus with 60° and 120° angles. The donor flap bisects the 120° angle. The flap is drawn to place the donor site scar within a normal facial crease or wrinkle. This can be determined by identifying the area of adjacent skin with the greatest laxity. Thus, redundant surrounding skin is transferred to the defect while the donor area is closed primarily. Modifications of the flap may be performed to avoid unnecessary excision of normal skin; however, more circular excisions resembling banner flaps may be complicated by pincushioning.
Rotation Flaps
Cervicofacial Flaps.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree










