div class=”ChapterContextInformation”>
17. Surgical Reconstruction of Panurethral Stricture Disease
Keywords
Panurethral strictureOne stage urethroplastyLichen sclerosus17.1 Introduction
Panurethral strictures involve the urethra from the meatus to the bulbomembranous junction . Lichen sclerosus and iatrogenic causes are two of the most common causes of panurethral strictures. Iatrogenic causes are on the rise, especially because patients are often subjected to dilatation and intermittent self-catheterization. The best option for management of a panurethral stricture is urethroplasty. We have published extensively on the management of panurethral stricture and the change from dilatations to flaps to grafts. The manuscripts are available in the Hinmans Atlas of Urology and UCNA [1–3]. In this chapter, we wish to highlight the decision-making process, surgical craft tips and the management of complex panurethral strictures.
17.2 Materials and Methods
At our tertiary referral center for the management of urethral strictures in Pune, we have received patients from all over India and the world, including patients with panurethral strictures. We have performed more than 4350 surgeries to date. A detailed history of the patient is taken, including any previous surgery. The clinical examination involves looking for lichen sclerosus. Occasionally, patients will have urinary retention and they are then referred with a suprapubic tube. Ultrasound is performed to look for renal health and rule out hydronephrosis. Uroflow forms an integral part of the workup as a baseline test. Usually patients come with a urethrogram. In our unit, we perform the urethrogram ourselves in the operating room (OR) under C-Arm on the day of urethroplasty. Patients are given povidone iodine gargles and Poviodine iodine or Chlorhexidine for local application to prepare for muccal mucosa grafting. Third generation cephalosporin IV antibiotic is started the evening prior to surgery. The surgical technique will depend on the type of panurethral stricture.
17.3 Surgery Techniques
17.3.1 Panurethral Strictures: Single Stage Versus Two Stage

Lichen sclerosus causing Panurethral stricture
Our approach is to perform a small caliber endoscopy using a 4.5 Fr ureteroscope. Occasionally we have seen urethral stones and bladder stones which had to be addressed intraoperatively and would otherwise have been missed.
If the urethra accepts a 4.5 Fr ureteroscope or a 3 Fr guide wire, it can be managed with a single stage approach.
17.3.1.1 Positioning and Initial Steps
The patient is nasally intubated and two teams work simultaneously at the donor and the recipient site, with separate sets of instruments. The oral mucosa is harvested from both cheeks as described by Barbagli et al.(ref) The patient is placed in a simple lithotomy position , with heels carefully placed in Yellofin ® stirrups (Allen Medical Systems, Acton, MA; USA) with no pressure on the calves, to avoid peroneal nerve injury. The suprapubic, scrotal and perineal skin is shaved, disinfected using chlorhexidine, and draped. Methylene blue is injected into the urethra.
17.3.1.2 Incision

Injecting methylene blue in urethra
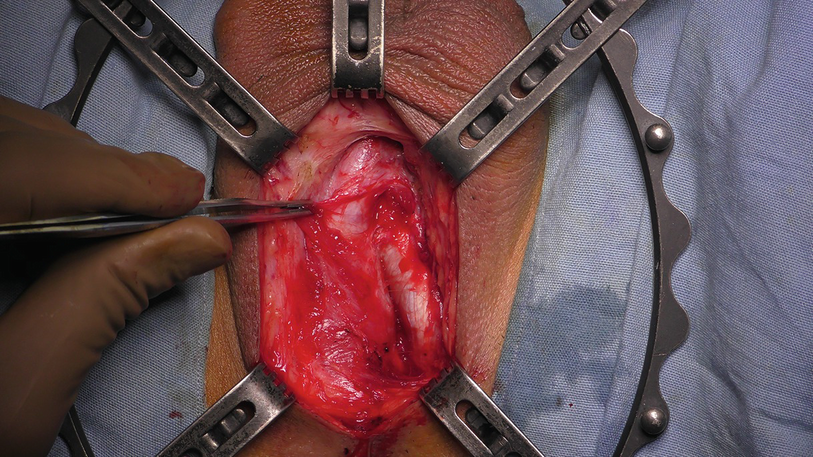
Incising bulbocavernosus muscle
One side dissection of bulbospongiosus muscle
17.3.1.3 Penile Invagination
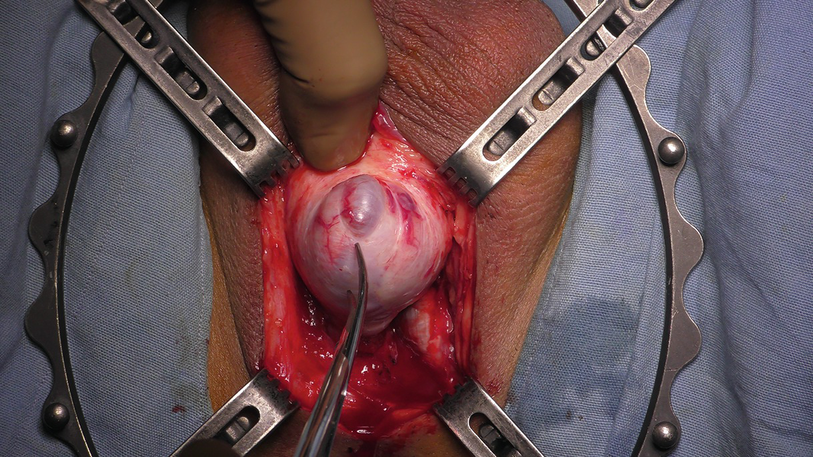
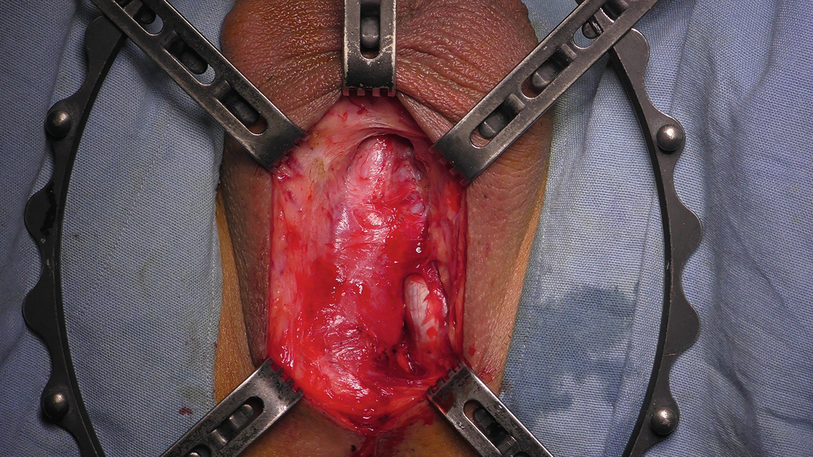
Penile Invagination
17.3.1.4 Urethral Dissection
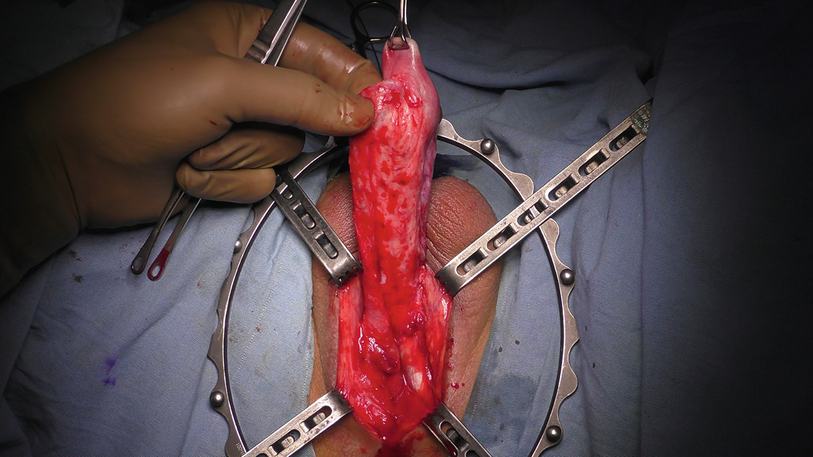
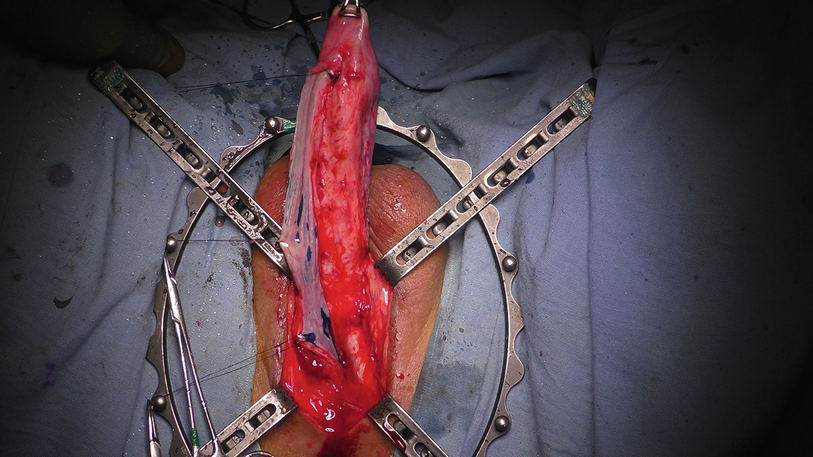
One sided dissection of anterior urethra
17.3.1.5 Urethral Incision

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree