Reconstruction of nasal tip and columella defects is demanding area with a range of reconstructive options, varying in complexity depending on requirements from simple skin grafting to multiple stage reconstruction with regional flaps. A framework is suggested to aid the reader in choice of reconstruction by classifying the defect based on size and the requirements of one to three layer (full thickness) reconstruction.
Tip reconstruction
Tip defects are common, bearing a potential for considerable aesthetic and functional deformity. Of the 850 nasal defects treated in the authors’ department, 325 involved the nasal tip, of which 70 were through-and-through defects. Because of its unique individual characteristics, reconstruction of the nasal tip is a challenging endeavor. The range of reconstructive options varies in complexity from simple grafting to 3- or 4-stage reconstruction with regional flaps. To sculpture a structure that simulates the nasal tip while allowing normal nasal function, the reconstructive surgeon is impelled to turn to current rhinoplasty knowledge and expertise. This expertise involves the application of both functional and aesthetic nasal analysis and modern rhinoplasty techniques to the reconstructive problem. Indeed, nowhere is the line between nasal reconstruction and rhinoplasty so blurred than in rehabilitation of defects of the nasal tip.
Tip Anatomy
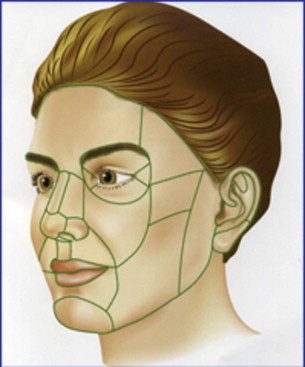
The nasal tip is a biconvex structure. It is unique in that it is the only nasal subunit that shares a common border with all remaining subunits of the nose (columella, dorsum, ala, soft triangle, sidewall) ( Fig. 1 ).
The shape and position of the nasal tip is determined both by the structure and position of the alar cartilages and by its skin, soft-tissue covering. Differences in skin characteristics, even within the nasal tip, can be appreciated. The majority of the nasal tip lies within a thicker skin zone, richly populated with sebaceous glands. The lower portion of the infratip lobule and soft triangle (separate subunit but juxtaposition to the tip subunit) lie within a zone with skin that is thinner, smooth, nonsebaceous, and adherent to the underlying cartilage. Obviously, as the replaced alar cartilage must mimic normalcy, the choice of skin covering must fit the preexisting state.
In frontal view, the nasal tip unit consists of 2 halves or subunits. In profile, one may discern the supratip and infratip lobule. The lower lateral cartilage (LLC) largely determines these transitions from one area to another and thus contributes to the development of the double break, tip defining point, and supratip break point ( Fig. 2 ). The transition of the medial crus to the intermediate crus forms an angle, which translates as a double break. This point is the most anterior point of the columella in profile and determines the transition from columella to infratip region. The highest point of the domal segment corresponds to the tip-defining point on each side. This pair of tip defining points is usually manifested externally by light reflexes. The supratip lobule ranges from the tip-defining point to the supratip break point. As the cephalic edge of the lateral crus slopes posterior it meets the dorsal septum producing the supratip breakpoint. This landmark defines the junction of the nasal dorsal and tip subunit. The transition from ala to nasal tip may best be assessed in basal view and is marked as the deepest point in this concave area ( Fig. 3 ).
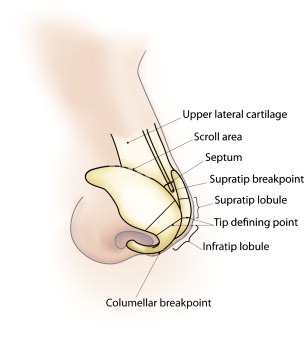
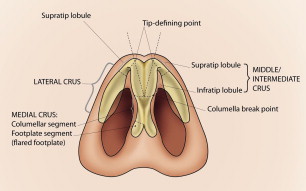
It may be clear that the shape of the cartilages translate as surface characteristics with, in general, gently flowing hills and valleys. The transition in shape from convex to concave does represent the borders of the nasal tip subunit. The delineation of the boundaries on the nose between concave and convex surfaces, which results in differences in light reflection and shadowing, may be clear or sometimes less defined. However, they present opportunities to hide the reconstructive scars in areas where a transition is expected, making them less readily apparent to the eye.
Placing the scar in the previously mentioned areas might imply enlargement of the defect. Indeed, given the advantage of scar camouflaging one may go so far that if 25% to 50% or more of the nasal subunit is involved, the excision of the remaining subunit is considered. For example, smaller defects limited to one-half of the nasal tip may be converted to a hemi-tip unit defect. The unaffected other half remains, and can be used as a template to mirror exactly the reconstruction. The vertical midline scar naturally divides the tip into an equal left and right half. For more extended tip defects, the whole nasal tip may be resurfaced. It must be stressed that if the transitions of the subunit are not clear, the aesthetic sense helps to delineate a further resection so that the size of the tip remains in harmony with the remaining nasal dimensions. Defects of the nasal (hemi or total) tip unit dictate more extensive reconstruction with the forehead flap. This point is subsequently discussed in more detail.
Tip Dynamics
In reconstruction of the nasal tip, a basic understanding of tip dynamics is helpful to appreciate the changes that occur by resections and of the steps one should follow in reconstructing the changes in nasal tip shape, position, and function. For example, skin-only resection may lead to loss of tip projection. Similar to external rhinoplasty, the skin has been lifted off the alar cartilages and thus one of the minor tip support mechanisms (skin-cartilage attachment) is damaged. Specifically in large resections, when part or all of the alar cartilage is missing, the reconstructed LLC must bear the weight of the whole reconstruction and withstand the retractile forces that will inevitably accompany healing and scar formation. It follows that, similar to reprojecting the nasal tip in rhinoplasty, the reconstructed cartilage tip complex must have a strong base and lateral components that ensure adequate nasal function. An overview of cartilage reconstruction follows.
Reconstructive Options
In reconstruction of the nasal tip, the authors aim for optimal aesthetic outcome (shape, position, scar, contour) with preservation of the nasal airway. The reconstructive plan will have to take into account tumor characteristics and patients’ wishes.
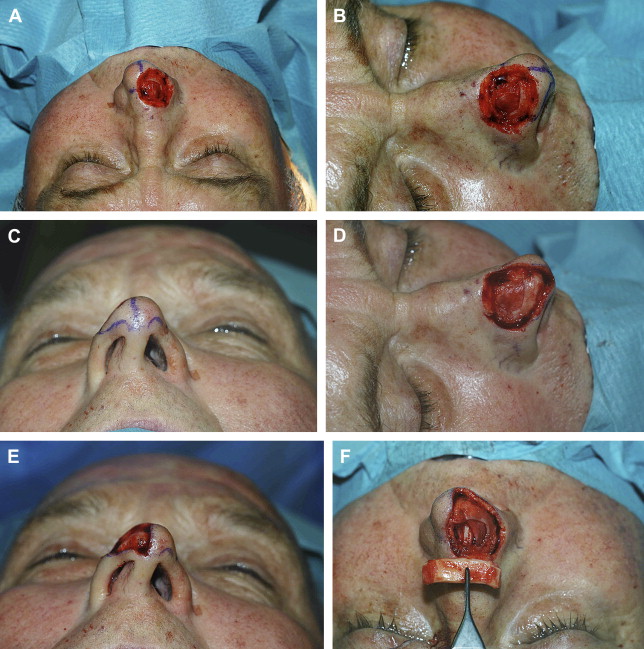
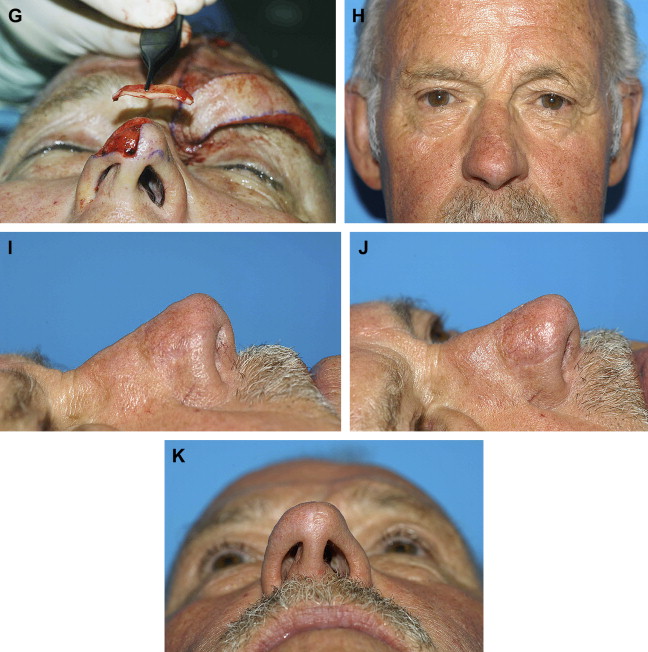
Cartilaginous framework for tip reconstruction
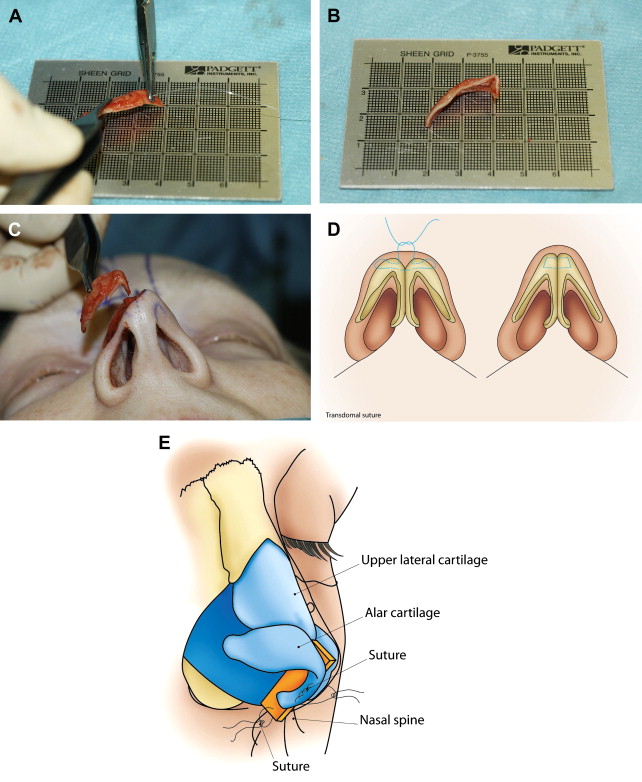
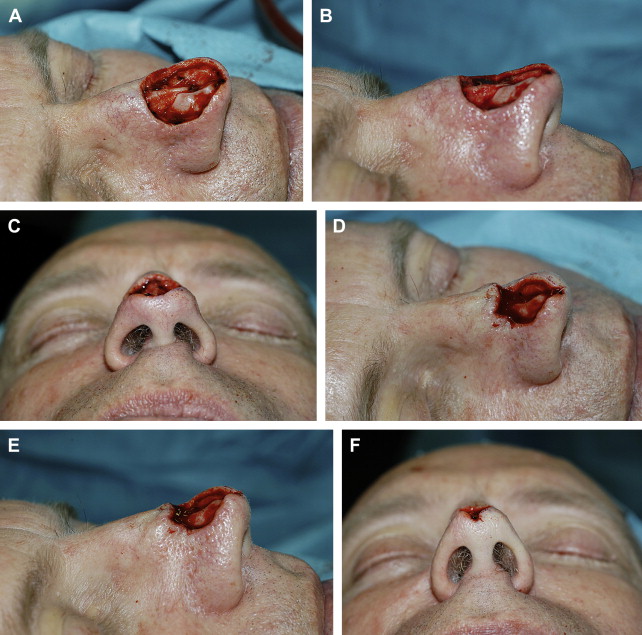
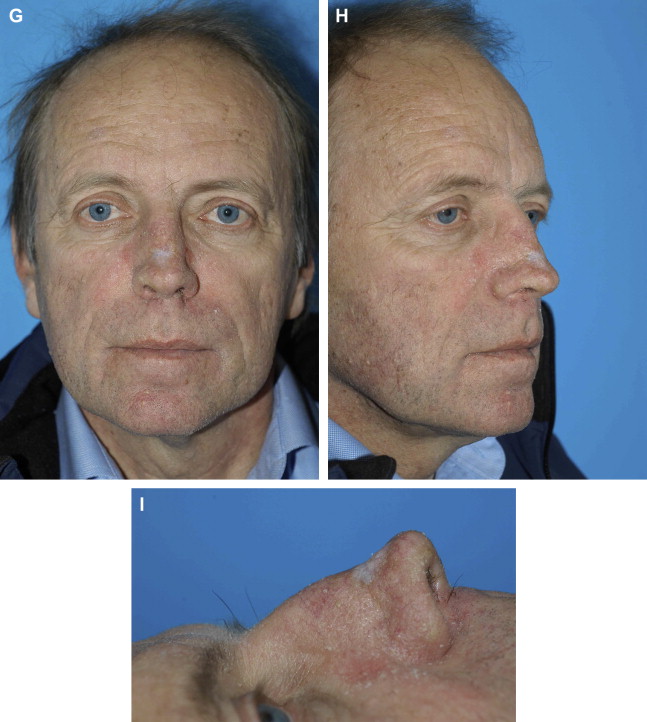
The review of the anatomy and tip dynamics aims to help the reader appreciate the importance of the interaction between the reconstructed cartilaginous framework and external appearance of the nose. The authors have come to appreciate how even small changes in the reconstructed cartilaginous framework impact the tip shape and position. The small loss of tip projection after skin-only excision, even with an intact underlying alar cartilage, can be compensated for by small tip grafting. As in rhinoplasty, grafts that contact the skin must be made to blend in to the remaining cartilage structure smoothly. Covering of tip grafts with perichondrium is considered. If the alar cartilage is damaged or missing it must be reconstituted. Ear cartilage harvested from the cymba concha is well suited because it has a preformed curvature. The Mustarde principle of suture shaping ear cartilage in combination with scoring is applicable to bend or straighten the neo-alar cartilage ( Fig. 4 A–C). This principle uses suture techniques from rhinoplasty, such as transdomal suturing, to mold the cartilaginous free grafts (see Fig. 4 D). Septal cartilage is ideal to extend the length of these ear cartilages more laterally, which gives support even onto the piriform aperture to preserve nasal valve function. Septal cartilage can be used to support the nasal tip in the columella region as a strut (see Fig. 4 E) or even septal extension graft, the latter offering maximum support.
To reposition and gain further support, the neo-alar is also fixed to the contralateral alar cartilage with interdomal sutures, which controls the width of the nasal tip. Essentially any of the tools used in rhinoplasty may be used depending on the experience of the surgeon.
At this stage it is important to make an assessment of the contractile forces on the lower two-thirds that will be exerted during the healing phase. To further support the free alar rim, alar rim grafts may come into play. Similarly, the soft triangle may need cartilaginous support. Spreader grafts or butterfly grafts are added so as to maintain nasal airway. For example, a butterfly graft beautifully repositions the recreated alar cartilages more laterally and opens up the external nasal valve.
Grafts in the alar-sill region that extend laterally from the neo-alar to the septal spine may be the final link in recreating a cartilage ringlike structure from the columella, tip, lateral wall, and sill, which may offer maximum control over position, shape, and function. One may also appreciate that apparent tip position is also related to the height and shape of the nasal dorsum.
To get an aesthetically balanced outcome, an overprotected nasal dorsum may be lowered to compensate for loss of tip projection while harmonizing with the recreated nasal tip. When the cartilaginous dorsum is lowered and the upper laterals become detached from the dorsal septal edge, spreader grafts may be needed.
Apart from aesthetic goals, the authors work hard to maintain function or even correct it at the time of reconstruction. Any septal deviation or preexistent valve abnormality may become a potential problem, even after a well-executed reconstruction, if not corrected or compensated for. Moreover, the authors have come to realize that functional problems after nasal reconstruction are not easy to deal with. Because of the different anatomy and scarring, the rhinoplasty techniques applied are less effective.
The application of the reconstruction options presented here must be based on a clear appreciation of the preoperative situation. This appreciation includes evaluation of the patients’ airway and possibly pre-excision, 4-view photograph documentation. Preoperative aesthetic analysis may suggest the reconstructive possibilities and needs. For example, nasal-tip rotation or nasal-dorsal reduction create a relative excess of the skin soft-tissue envelope and help to diminish the size of the defect, which may then allow for a simpler reconstruction. The precise reconstitution of the cartilaginous framework cannot be overstated because this directly relates to the final results.
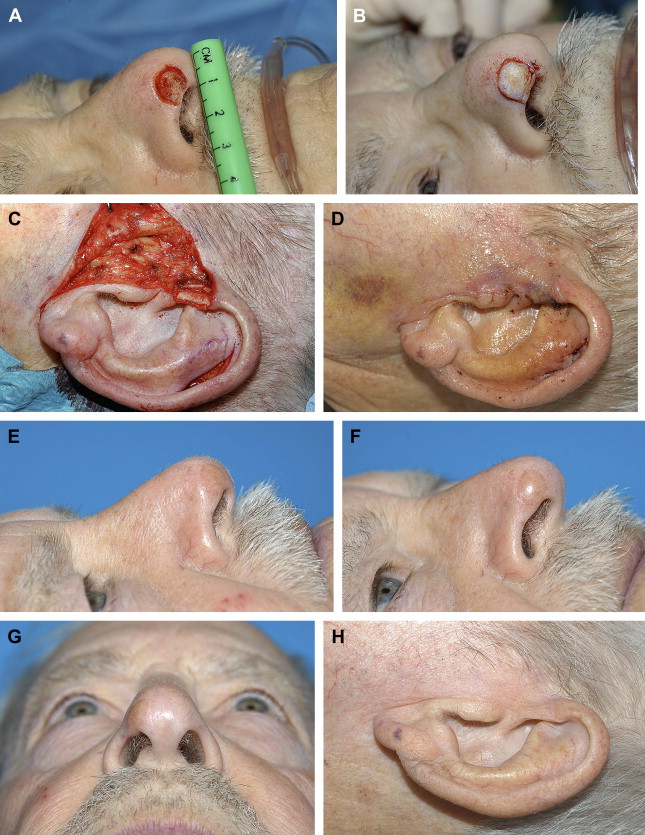
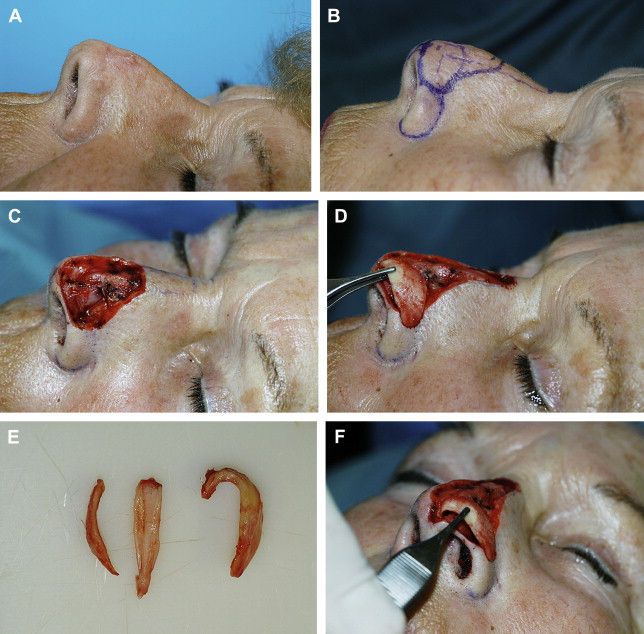
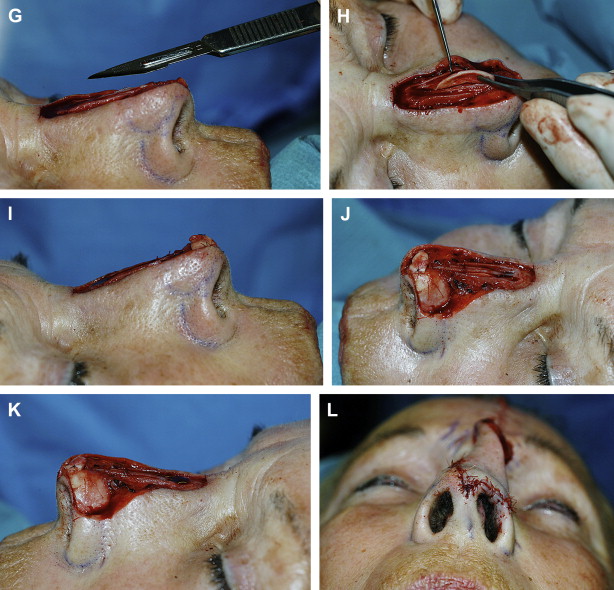
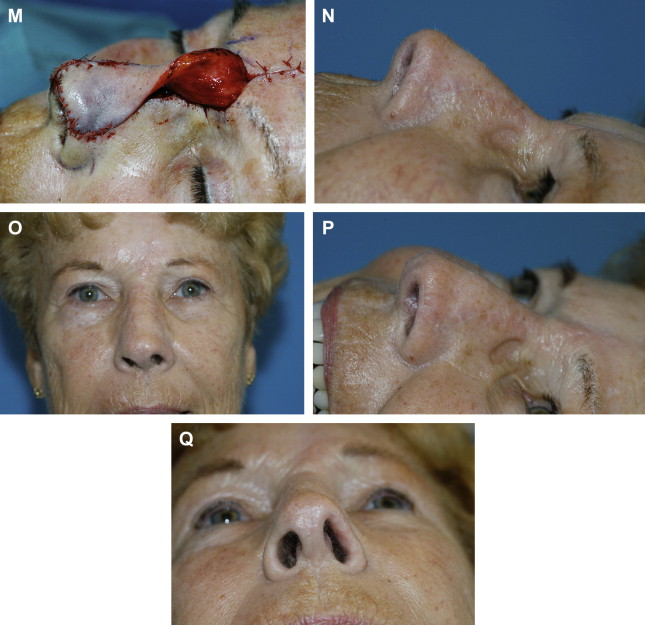
An example is given of a reconstructed alar cartilage, including tip grafting and dorsal reduction, with the application of spreader grafts ( Fig. 5 ), and another case with cartilage butterfly-type reconstruction ( Fig. 6 ).
Nasal lining reconstruction
In through-and-through defects, 3 different layers are missing. The 3 components include lining, cartilage framework, and skin covering. If the different layers are reconstructed separately, each can be manipulated, shaped, and placed to contribute to the best possible outcome. Nasal-tip defects with inner lining defects often result from inferior and lateral extensions of the tumor onto the infratip lobule and the adjacent soft triangle, thereby reaching and growing over the nostril margin into the nose. Alternatively, lateral impingent of the tumor deep into the alar subunit may also result in nasal cavity involvement. Direct deep extension into the vestibule of isolated nasal-tip lesions is unusual because of the barrier afforded by the lower lateral cartilages and their perichondrium.
The considered lining options follow a logical reconstructive ladder from simple to more intricate. Small defects can be left to heal by secondary intention. Primary closure may, although infrequently, be an option. Caution must be exercised not to significantly diminish the internal diameter of the nasal airway.
Skin grafts can be applied onto the defect wound edges, which in a subsequent stage will serve as lining. After 2 or 3 months, when the wound edges have been skin covered and healed, the previous graft can be developed from superior to inferior and hinged into the lining deficit. Skin grafts can also be applied to the undersurface of skin flaps used for skin covering in the first stage of the reconstruction. There is a slight risk of graft failure. A second, intermediate stage is used for placement of cartilage grafts. The simplicity of this is alluring, but one has to be exact with the cartilage shape and position because at the third stage pedicle division is performed precluding further cartilage reshaping.
Skin-cartilage composite grafts offer 2 layers for reconstruction, but they are difficult to shape while placing the skin part of the graft exactly in the lining defect. However, in defects of less then 1 cm that involve the free border of the columella, soft triangle, and tip, they have an outstanding record. Ideally, some remaining lining will enhance vascular growth and increase the chance of survival.
Flaps have the advantage of carrying blood supply to support primary cartilage grafting. However, these flaps must be thin and supple to follow the desired contour and not impinge on the nasal airway. For clarity, the authors conceptualize flaps for lining by categorizing them according to donor site rather than flap type or tissue movement. Thus the possible donor sites include
Septum (ipsilateral or contralateral)
Lateral nasal wall (inside or outside)
Adjacent facial units (melolabial fold, forehead)
Of the septal flaps, only the ipsilateral anterior-based septal flap offers enough tissue and reach to be of value for tip reconstruction ( Fig. 7 ). The inside of the lateral nasal wall may yield tissue often moved caudally as bipedicled mucosal flaps or more rarely as an anteriorly pedicled inferior turbinate flap. The outside of the lateral nasal wall offers ample tissue to be developed from superior to inferior and hinged into the lining defect. A major advantage is that the inside of the nose is not taken apart. These thicker flaps are sturdy and thin spontaneously over time.
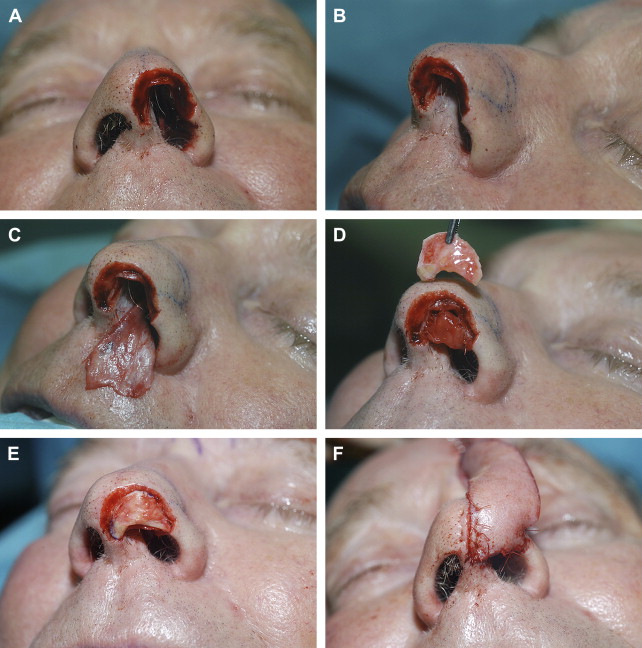
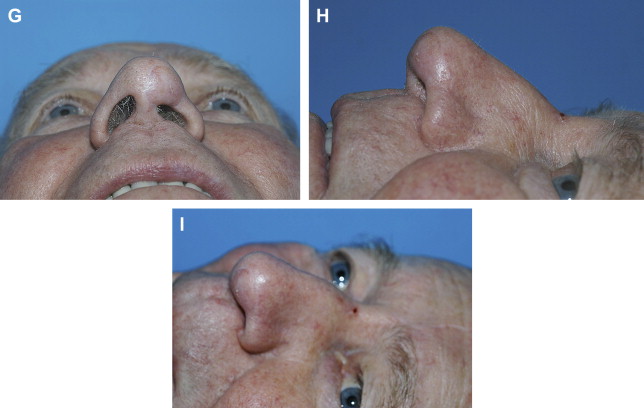
For tip defects, the forehead flap may be folded inward as lining. In an intermediate stage, the bulky flap is incised caudally, divided, and thinned aggressively. Cartilage can be added at that stage. The pedicle is divided at the final stage ( Fig. 8 ).
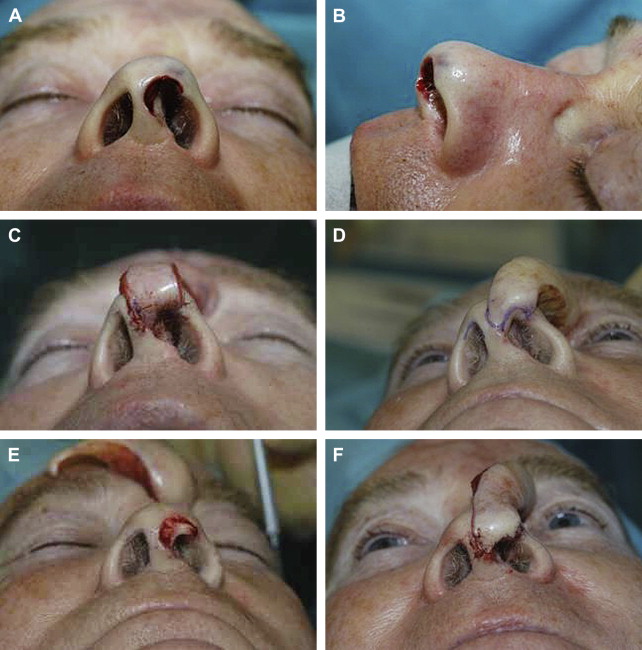
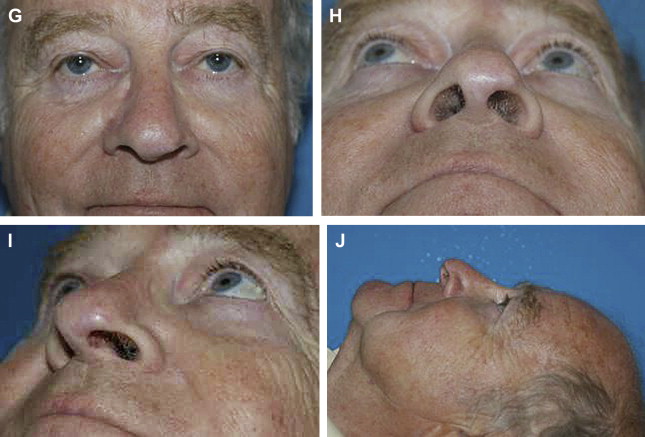
The authors suggest that tip-cartilage reconstitution is so demanding that a 3-layer, 3-stage reconstruction yields the best possibilities for an aesthetic shape. The precise cartilage grafting done at the first stage can be improved upon at 3 weeks during the intermediate stage. The forehead flap left pedicled superiorly can be lifted completely out of the wound bed and thinned as necessary. Cartilage can be shaped, refined, and added if needed.
Of course, the exact choice of reconstruction of the defect depends upon patient and defect factors. Patient factors, such as diabetes or smoking, make the fragile vestibular and septal flaps more prone to fail. Sometimes multiple lining options are used to compliment each other.
Skin resurfacing
Nasal-tip defects may be classified according to the location, size, and depth of the defect. As cartilage framework and lining reconstruction have already been discussed, the focus turns specifically to skin covering. Again, adherence to a general reconstructive ladder listing the multiple options available from simple to more intricate is suggested (second intention healing, primary closure, skin grafts and local/regional flaps).
The choice and application of these techniques logically parallels the defect size. Thus, defects are subdivided into small (1 cm or less), moderate (1.0 to 1.5 cm), and large defects (greater than 1.5 cm). Again, there are no distinct cutoffs between the 3 categories, but these distinctions are not arbitrary.
The authors’ preferred options in reconstruction of the nasal tip are free skin/composite grafting and regional flaps (the forehead flap). For smaller defects (<1 cm), skin grafting (including composite skin-fat and skin-cartilage grafts) as well as local flaps are commonly used. Full-thickness skin grafts are taken from the melolabial fold or forehead region. These areas provide the best match in color, texture, thickness, and sebaceous glands. Local flaps are developed in the middle and upper nasal vault, if the defect is slightly larger (1.0 to 1.5 cm) or when patients present with recipient sites that are not ideal (patients with diabetes or who smoke), indeed local or regional flaps are good alternatives to skin grafts. In larger defects (>1.5 cm), the subunit principle is often applied and a forehead-flap reconstruction is executed.
Small skin defects (≤1 cm)
Secondary intention healing
Because of its simplicity and the possible excellent results, secondary intention healing has to be considered in any defect. Secondary intention wounds heal by the process of filling in the defect with granulation tissue, re-epithelialization, and scar maturation. The best possible results are related to shape, depth, and size of the defect. Small superficial wounds in concave areas in fair patients with thin skin can do extremely well. The nasal tip, however, is mostly convex, largely covered with a thicker often sebaceous quality of the skin, which does not favor secondary intention healing. However, to demonstrate the possibilities of second intention healing, a rare case is presented ( Fig. 9 ).
Primary closure
Primary linear closure is a rare possibility only in lax abundant skin. If the skin covering is thick and sebaceous it is also immobile and unaesthetic scars must be anticipated. In the supratip-dorsum junction a horizontal closure may be acceptable. Lateral dog-ear excision and tip rotation are logical sequelae. This scar will come to lie in relaxed skin tension lines (RSTLs) and in the aesthetic subunit boundaries. A vertical midline with dog-ears projected superior and inferior is a variation. On any other part of the tip a linear closure, even if following the RSTL, must be discouraged. Closure tension will flatten and even indent the natural convex surface of the nasal tip. The scar will be perceived readily as an interruption of the smooth, convex contour of the nasal tip. If simplicity is sought rather then aesthetics, the defect may be partly closed by superior and inferior dog-ear excision and horizontal skin advancement. A skin graft may cover the remainder of the defect. Alternatively, the excised dog-ears can be applied.
Skin grafts
When secondary intention healing or primary closure is not suitable, skin/composite grafts are the next option, having distinct advantages over local flaps in most cases.
Skin/composite grafts are quick to perform and multiple donor sites are available. The aim is to reproduce the color/texture match with maximal contour. Full-thickness skin grafts (FTSGs) have been used but may unfortunately lack volume, which can produce quite obvious contour defects on the convex nasal tip. Alternatives include skin/perichondrial, skin/fat, and skin/cartilage composite grafts. The ideal donor site will depend on what portion of the nasal tip is deficient.
Full-thickness skin grafts
The use of FTSGs in nasal-tip reconstruction is well established. This option continues to be an excellent choice for several reasons. It is a simple single-stage technique. Survival rates range from 70% to 90% and depend on recipient site factors, patient factors, and technique. The recipient site should ideally be well vascularized (subcutaneous tissue, fascia) with a lack of infection. Patient health factors that adversely affect graft survival include diabetes mellitus, smoking, and malnutrition. Technique factors, such as antibiotic prophylaxis; careful handling of the graft; strict hemostasis while avoiding too much cautery; antibiotic/saline irrigation of graft and recipient site before placement; sutures that eliminate shear between the graft and recipient site (but risk bleeding); and a soft, not overly pressured bolster (often with Steri-Strips only [3M, St Paul, Minnesota]), help reduce graft failure.
FTSGs involve a specific set of challenges. Typically, the skin of the convex nasal tip is thick and sebaceous. What then is the ideal donor site and graft type to reduce the often patchwork postoperative appearance caused by color mismatch and contour defects?
Various donor sites for FTSGs are available, such as the preauricular and postauricular regions, conchal bowl, melolabial, forehead, and supraclavicular region. The forehead and melolabial fold possibly represent the most closely matched site for nasal-tip reconstruction in terms of surface characteristics and sebaceous glad population. The donor-site scar can be well hidden in the melolabial crease or forehead rhytids with minimal aesthetic compromise.
Composite skin grafts
are of the follwing 3 types:
Skin-fat composites grafts
Classical teaching suggests that skin grafts must be defatted to enhance blood vessel growth and survival. But thinner skin grafts are associated with contour deficits. The question arises whether it is possible to retain subcutaneous fat while aiming for an enhanced contoured reconstruction. In Fig. 10 , the authors present a case of tip reconstruction using a composite skin-fat graft to effect optimal tip contour.

The complete survival rate of these skin/fat composite grafts are in the range of approximately 80%. But even if the superficial parts do not seem to survive completely, the overall postoperative result show good contour. A degree of hypopigmentation and some loss of sebaceous glands may accompany these grafts. Dermabrasion may reduce some of the color mismatch or contour discrepancy. Given the possibilities and minimal risks involved, skin-fat composite grafts are an excellent option for deep nasal-tip defects less than 1 cm in diameter.
Perichondrial cutaneous composite grafts
Perichondrial cutaneous composite grafts (PCCGs) are composite grafts (usually harvested from the conchal bowl) consisting of skin and a thin perichondrial layer. Its use is based on the theory that if one maintains the perichondrial plexus in a skin perichondrial composite it may allow for quicker revascularization of the graft, lower graft failure rates, and less retraction. Indeed, clinical studies suggest tendency of improved graft take. The conchal bowl donor site is easily managed by second intention healing.
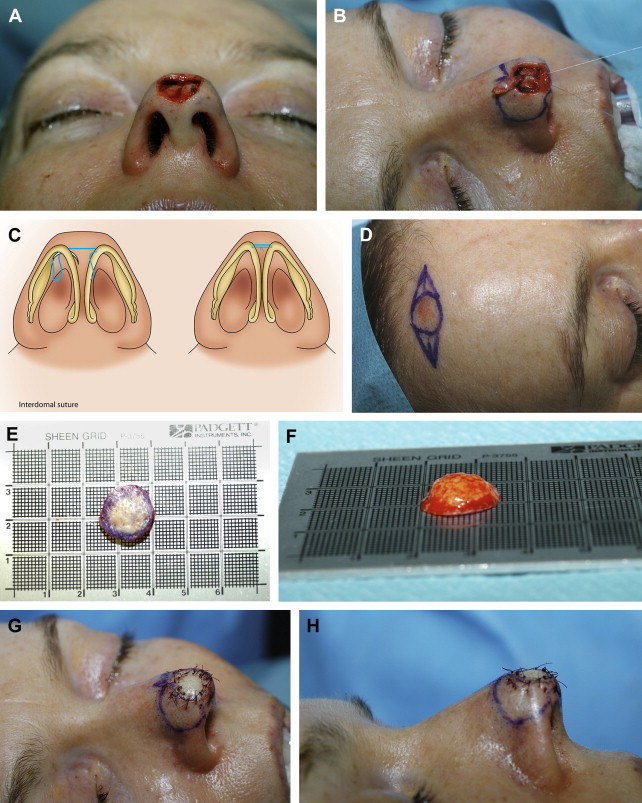
Skin/Cartilage composite grafts
Composite chondrocutaneous grafts are an excellent alternative to other grafts in specific circumstances.
They contain skin and cartilage usually harvested from the helical root. The benefit of including cartilage is the inherent shape and support. These characteristics can be used in reconstructing rims that otherwise are complex to reproduce. Skin/cartilage composite grafts do, however, have an increased metabolic demand and most authors agree that they have a somewhat higher failure rate than FTSG or PCCGs. However, much depends on patient selection. Skin/cartilage composite grafts are not used in patients who smoke or have diabetes, and the authors limit their size to a maximum of 1 cm. Ideally, some inner lining remains to increase the graft’s vascular support. Thus, for nasal reconstruction the indication for skin cartilage grafts are partial defects of the columella, soft triangle, and alar rim where one requires not only replacement of skin but also a definite shape. In Fig. 11 , the authors present a case where a soft-triangle defect is reconstructed with a chondrocutaneous graft.