Raynaud Phenomenon: Introduction
|
Epidemiology
Studies of the epidemiology of Raynaud phenomenon are biased by underreporting (most patients with primary Raynaud never seek medical attention) and studies done by investigators interested in the secondary forms of the disorder. Surveys indicate that Raynaud phenomenon affects up to 10% of the general population.1,2 Primary Raynaud phenomenon is estimated to be approximately twice as common as secondary Raynaud.3 Symptoms most often first develop in the teenage years, and most series show a female predominance of the disorder (female–male = 4:1). Increases in the frequency and severity of attacks during menses suggest that female sex hormones may be involved in the pathogenesis.4 Differences in seasonal skin temperatures, marital status, alcohol use, age, and smoking between women and men have also been suggested to contribute to the sex differences.5,6 Familial aggregation has been identified in a number of studies and suggests the contribution of genetic factors.7 Other associations reported in epidemiologic studies include living in a cold climate, occupation, cardiovascular disease, low body–mass index, and use of vibratory tools.
Etiology and Pathogenesis
The pathophysiology of the vasospasm is complex and only partially understood. Studies show significant reductions of peripheral blood flow throughout all phases of central body cooling and rewarming, suggesting impairments of central thermoregulatory control mechanisms.8 Additional features which likely contribute to the development of Raynaud phenomenon include local defects of digital blood vessels causing abnormal vascular reactivity or reduced blood flow; an imbalance of locally produced vasoconstrictors or vasodilators; hyperreactivity of the sympathetic nervous system; and abnormal properties of the blood that compromise distal perfusion.
The gross histology of digital arteries in patients with primary Raynaud phenomenon is normal. Structural abnormalities of the digital microvasculature are frequently seen in patients with secondary forms of Raynaud phenomenon, particularly in the connective tissue diseases. Studies show a range of pathology, including intimal hyperplasia, narrowing or total occlusion of arteries, or thrombi. In most patients with systemic sclerosis, there exists evidence of activation and damage of the endothelium, fibrinolysis, and platelet activation.9 Autoantibodies and microvascular damage appear to be independent predictive factors for the progression of Raynaud phenomenon to systemic sclerosis.10
Microcirculatory flow studies with laser Doppler in patients with scleroderma have shown marked reductions in blood flow and hand temperature during an attack, with prominent abnormalities during rewarming—findings that suggest a failure of the arteriovenous anastomoses to open.11
Serotonin is also incriminated as an important mediator in the induction of ischemic attacks of Raynaud phenomenon. Patients have an increased sensitivity to intra-arterial infusions of serotonin, and S2-serotonergic antagonists relieve but do not prevent the induction of attacks.
The evidence of direct central sympathetic nervous system hyperactivity is strongest in vibration-induced injury. The use of a vibration tool in one hand produces vasospasm in the other hand, and vasospasm can be inhibited by proximal nerve blockade.12 In general, most studies of the sympathetic nervous system in patients with primary or other secondary forms of Raynaud phenomenon have failed to detect evidence of sympathetic hyperactivity. The results of microelectrode studies of skin sympathetic nervous activity during cold pressor tests are normal, and plasma levels of catecholamines are not increased in the venous drainage of the hands of patients with Raynaud phenomenon.
Consistent abnormalities in plasma fibrinogen, cold agglutinins, platelets, or cryoglobulins have not been demonstrated in primary Raynaud phenomenon, but are important in certain secondary cases, particularly scleroderma. Levels of von Willebrand’s factor and soluble thrombomodulin, thromboxane B2 and β-thromboglobulin, and tissue plasminogen activator inhibitor-1 are increased in patients with scleroderma, when compared to levels in patients with primary Raynaud phenomenon.9
Genetic studies with microsatellite markers of extended families affected with primary Raynaud phenomenon have identified several potential candidate genes.13
Clinical Findings
A careful history and physical examination are important in the evaluation of a patient with suspected Raynaud phenomenon.
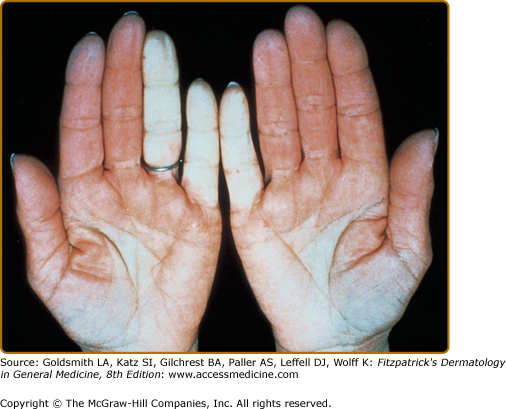
The history is important to elicit a clear description of the attacks and to screen for evidence of signs and symptoms suggestive of a secondary cause. Patients complain of episodic attacks of well-demarcated, white or blue digits induced by exposure to cold and sometimes by emotional stimuli (Fig. 170-1). Often only a portion of the digit is affected, and the thumbs are typically spared. A classic tricolor change of pallor, cyanosis, and hyperemia described in most textbooks is rarely volunteered by patients; most describe only blanching of the digits accompanied by numbness. During the attacks, one or more fingers or toes may be numb and be described as “dead.” On rewarming, the digits may become bright red, and throbbing pain may occur. When pain is a prominent symptom in the ischemic phase, a secondary cause should be suspected. Attacks persist for minutes to hours. The fingers and toes are most commonly involved; however, the attacks may involve the nose, earlobes, or nipples.
A careful review of systems is important to screen for symptoms of connective tissue disease (arthralgias, arthritis, dysphagia, heartburn, rash, photosensitivity, telangiectases, calcinosis, muscle weakness, shortness of breath, or sicca), a drug-related etiology, symptoms of obstructive arterial diseases (intermittent claudication), and exposure to vibratory tools or continuous finger trauma.
Attacks of Raynaud phenomenon, presumably stress induced, are commonly witnessed during the course of the history or physical examination. There is well-demarcated blanching or cyanosis of the digits extending from the tip to various levels of the digit (see Fig. 170-1). The skin distal to the line of ischemia is cold and pale, while the proximal skin is pink and warmer. On rewarming, blanched digits may become cyanotic, because of the low blood flow and deoxygenation, and then bright red, because of reactive hyperemia. Persistent ischemic discoloration of digits suggests a secondary cause.
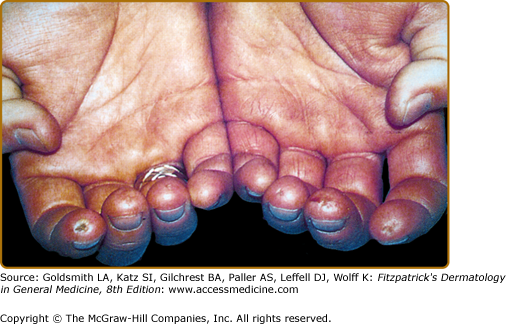
The digits should be carefully examined for trophic or ischemic changes, which are signs of prolonged or severe attacks of Raynaud phenomenon. The skin may become atrophic, thin, and tight (sclerodactyly) and hair loss may occur over the dorsal surfaces. The nails may become brittle and deformed. Ulcerations, which can be extremely painful, particularly at night, may develop on the finger pads or around the nail bed. The ulcers heal slowly, leave characteristic small, pitted scars (Fig. 170-2), and may become infected. Gangrene of the distal aspects of the digit is rare.
The physical examination should pay attention to all pulses, and blood pressure should be obtained in both arms. Allen’s test is useful to assess arterial and capillary function of the hands. Abnormal filling implies structural disease of the microcirculation and raises the suspicion of a secondary form of Raynaud phenomenon. In this test, the radial and ulnar arteries are simultaneously compressed by the examiner’s thumbs, while the patient opens and closes the fist to induce blanching of the palm. Selective arterial filling is judged by the rate of color return as pressure is sequentially released from the radial and ulnar arteries. Vascular obstruction from the thoracic outlet syndrome should be assessed by the Adson maneuver, which tests for diminution in the radial pulse with exaggerated movements of the neck and shoulder. A careful neurologic examination should be performed to detect evidence of sympathetic hyperactivity, abnormal reflexes, muscular weakness or atrophy, or compression of the median nerve within the carpal tunnel. Skin changes, such as telangiectases, calcium deposits, changes in skin texture, rashes, or purpura, provide valuable clues to the presence of a connective tissue or hyperviscosity disorder.
Laboratory Tests
In all patients, a complete blood count, erythrocyte sedimentation rate, urinalysis, and antinuclear antibody test should be obtained. Additional laboratory studies should be directed by findings elicited by the history and physical examination. In patients with abnormal antinuclear antibody levels, tests for antibodies to specific nuclear antigens, such as Sm antigen or topoisomerase or centromere antigens, are helpful to detect early systemic lupus erythematosus or scleroderma (see Chapters 155 and 157). A routine chest radiograph should be obtained to look for a cervical rib or evidence of interstitial lung disease.
Special Tests
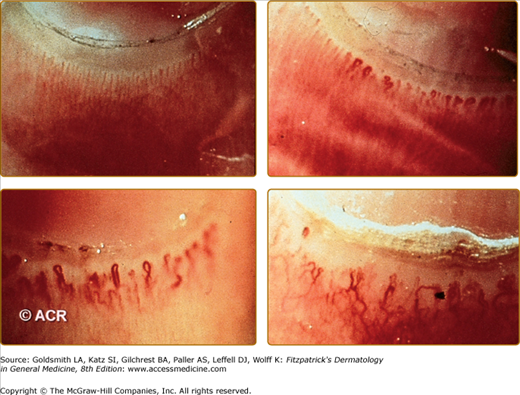
Nail fold capillary microscopy is considered to be a useful procedure to distinguish primary from secondary Raynaud phenomenon.14 Although mild capillary abnormalities may be observed in patients with primary Raynaud phenomenon, patients with connective tissue diseases may have enlarged, deformed capillary loops surrounded by avascular areas (Fig. 170-3).15 Serial studies reveal progressive decreases in the total number of nail fold capillary loops in secondary, but not primary, forms of Raynaud phenomenon.16 The patency of small arteries can be assessed by laser Doppler perfusion imaging.17,18 Digital subtraction arteriography should be reserved for selected patients with prolonged, severe ischemia for whom arterial reconstruction is a consideration.
Differential Diagnosis
Raynaud phenomenon is subdivided into primary (idiopathic) and secondary forms based on whether an underlying cause or disease association can be identified.
Primary Raynaud phenomenon is a disorder in which known causes of attacks of peripheral vasospasm cannot be found. Criteria for the diagnosis of primary Raynaud phenomenon have been developed by Allen and Brown19 and LeRoy and Medsger20 (Table 170-1).