Chapter 42 Radiation injuries and vesicant burns
![]() Access the complete reference list online at http://www.expertconsult.com
Access the complete reference list online at http://www.expertconsult.com
![]() IN THIS CHAPTER
IN THIS CHAPTER ![]() PowerPoint Presentation Online
PowerPoint Presentation Online
Introduction
Only 4 months after Roentgen reported the discovery of X-rays, Dr John Daniel observed that irradiation of his colleague’s skull caused hair loss. Since this finding was reported in 1896, many biomedical effects of radiation have been described.1 Knowledge of nuclear physics was rapidly amassed in the early part of the 20th century, leading eventually to the Manhattan project and the development of the atomic bomb. The last 50 years has also seen widespread deployment of energy-generating nuclear reactors, and the expanding use of radioactive isotopes in industry, science, and healthcare.2 More recently, major industrial accidents of note at Three Mile Island in Pennsylvania, Chernobyl in the Ukraine and at Goiania, Brazil have resulted in potential or real radiation injuries to hundreds of people. According to the latest NCRP report on radiation exposure to United States citizens, the most significant increase in ionizing radiation exposure, over the last 20 years, has been through medical imaging.3 Health professionals have become more aware of the cumulative effects of radiation. This has become a common topic for debate in regards to ionizing radiation exposure during the treatment of breast cancer patients and children.
Exposure to ionizing radiation can follow one of three patterns:
1 Small-scale accidents, or cumulative exposures, as might occur in a laboratory or from an X-ray device in a hospital setting.
2 Large industrial accidents (such as those mentioned above), stretching the need for treatment beyond available resources.
3 Detonation of a nuclear device in a military conflict where resources are totally overwhelmed or unavailable and associated multiple and combined injuries also exist.
Radiation injuries
Terminology
Damage to biological tissue by ionizing radiation is mediated by energy transference. This can be the result of exposure to electromagnetic radiation (e.g. X-rays and gamma rays) or particulate radiation (e.g. alpha and beta particles or neutrons). The severity of tissue damage is determined by the energy deposited per unit track length, known as linear energy transfer (LET).4 Electromagnetic radiation passes through tissue almost unimpeded by the skin and are called low LET since little energy is left behind. In contrast, neutron exposure has high-LET, resulting in significant energy absorption within the first few centimeters of the body. Alpha and low-energy beta particles do not penetrate the skin, and represent a hazard only when internalized by inhalation, ingestion or absorption through a wound.
The biological effect of ionizing radiation is measured by the radiation absorbed dose (rad). The newer SI unit of absorbed dose is the gray (1 Gy = 100 rads). Not all radiation is equally effective in causing biological damage, although it may cause the same energy deposition in tissue. For example, 1 Gy of neutron radiation will not have the same effect as 1 Gy of gamma or X-radiation. For this reason, a unit of dose equivalence was derived that allows radiations with different LET values to be compared. One such unit is the rem (acronym of roentgen equivalent man). The dose in rem is equal to the dose in rads multiplied by a quality factor (QF).5 The QF takes into account the linear energy transfer and has a different value for different radiations; for X-rays it is 1.0, for neutrons 10. The international unit, now more widely in use, is the sievert (Sv). One sievert equals 100 rem; 1 rem equals 10 mSv. This allows radiations with different LET values to be compared, since 1 Sv of neutron radiation has the same biological effect as 1 Sv of low LET gamma or X-radiation.
Incidence
A significant radiation accident is one in which an individual exceeds at least one of the following criteria:6
• Whole body doses equal to or exceeding 25 rem (0.25 Sv)
• Skin doses equal to or exceeding 600 rem (6 Sv)
• Absorbed dose equal to or greater than 75 rem (0.75 Sv) to other tissues or organs from an external source
• Internal contamination equal to or exceeding one-half the maximum permissible body burden (MPBB) as defined by the International Commission on Radiological Protection (this number is different for each radionuclide)
• Medical misadministrations provided they result in a dose or burden equal to or greater than the criteria already listed above.
Radiation accidents within the United States should be reported to the federally funded Radiation Emergency Assistance Center/Training Site (REAC/TS). This is operated by Oak Ridge Institute for Science and Education (ORISE) at Oak Ridge, Tennessee and can be contacted by calling (865) 576–1005 (website: http://orise.orau.gov/reacts/). A radiological emergency response team of physicians, nurses, health physicists, and support personnel provides consultative assistance on a 24-hour basis and has the capability of providing medical treatment, whenever a radiation accident occurs. REAC/TS also maintains a Radiation Accident Registry System.
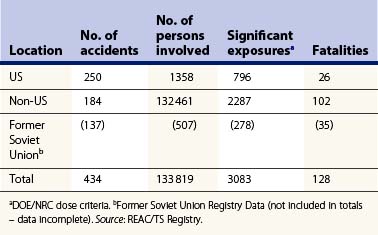
The number of accidents, number of persons involved, as well as the number of fatalities, in the United States and worldwide is shown in Table 42.1. There have been a total of 128 fatalities recorded by the Registry worldwide.6 The majority of the radiation deaths occurred as a result of the Chernobyl accident in 1986 (>40). The classification of radiation accident by device for the period 1944 until June 2010 is shown in Table 42.2.6
Table 42.2 Major radiation accidents worldwide (1944–June 2010): ‘classification by device’
| Radiation devices | 320 |
| Sealed sources | 212 |
| X-ray devices | 83 |
| Accelerators | 25 |
| Radar generators | 1 |
| Radioisotopes | 96 |
| Diagnosis and therapy | 40 |
| Transuranics | 28 |
| Fission products | 11 |
| Tritium | 2 |
| Radium spills | 1 |
| Other | 13 |
| Criticalities | 20 |
| Critical assemblies | 8 |
| Reactors | 6 |
| Chemical operations | 6 |
| Total | 435 |
Source: REAC/TS Registries.
The most devastating radiation injuries and fatalities yet seen, however, resulted from detonation of nuclear weapons at Hiroshima and Nagasaki during World War II. Since 1945, nuclear weapon technology has developed enormously and current strategic thermonuclear warheads dwarf those weapons used in Japan.7 Keep in mind that the bombs dropped on Japan still contained the same energy equivalent to 12–15 thousand tons of TNT (Hiroshima) and 20–25 thousand tons of TNT (Nagasaki).8 The majority of radiation exposure in this case occurred within the first minute of the explosion. There were no deaths attributed to the products left behind by the atomic explosions. As detailed by Kucan in 2004, the majority of radioactive fallout from these weapons were dispersed into the atmosphere, as both were detonated several thousand feet in the air.8
Perhaps a more likely weapon of terrorism will involve the use of a radiological dispersal device (RDD). The term dirty bomb generally refers to conventional explosive packaged with radioactive material that is scattered over a wide area when detonated. It is believed that these devices would probably elicit more harm by public fear and panic than by serious injury.9 Perhaps a greater threat might be the use of radioactive material placed in a public place without use of explosives, as illustrated by the event in Goiania, Brazil where 249 people were affected by radiation when cesium-137 was unwittingly released by scrap metal workers.
More recently, the media has propagated an interest in medical imaging as a source for excessive exposure to ionizing radiation. While most of the literature that explores this issue refers to case-studies, it confirms that exposure at a younger age increases the risk of cancer. Even more important is that this risk is not reduced with time.10 Exposure to radiation through CT imaging is now commonplace, as CT scanners are readily available and provide quick studies. Healthcare personnel should not disregard the cumulative effects of these studies which can approximate levels seen in atomic bomb survivors (30 mSv).11 This issue affects millions of patients on a daily basis and has the potential to increase the cancer risk in thousands of patients yearly.
Pathophysiology
The detonation of a nuclear device over a population center will produce an extremely hot, luminous fireball, which emits intense thermal radiation capable of causing burns and starting fires at considerable distance. This is accompanied by a destructive blast wave moving away from the fireball at supersonic speed and the emission of irradiation, mainly gamma rays and neutrons.12 The result of a combination of thermal and radiation injuries is said to have a synergistic effect on the outcome. Several animal experiments have demonstrated a significant increase in mortality when a standard burn wound model is irradiated, over and above that expected from either injury alone.13,14
Thermal effects
Exact information about the cause of fatalities in a nuclear blast is not available, but from the nuclear attack on Japan, it has been estimated that 50% of deaths were due to burns and some 20–30% were flash burns.15 The clinical picture may range from an erythema of the exposed areas (most commonly face, hands, arms and legs), to a charring of the superficial layers of the skin. Secondary flame burns may be present following the ignition of the victim’s clothing or environment. The physicians at Hiroshima and Nagasaki observed that the ‘flame’ burn wound seemed to heal at first. However, between 1 and 2 weeks later, a serious relapse occurred. Wound infection set in; there was a disorder in granulation tissue formation; a gray, greasy coating would form on the wounds. Thrombocytopenia resulted in spontaneous bleeding both into the wound and elsewhere. Histologically, the normal collection of leukocytes delineating a necrotic area was found to be absent due to agranulocytosis, and gross bacterial invasion was evident;16 both these changes obviously affected the prognosis of these otherwise relatively small injuries.
Radiation effect
Damage to biological tissue by ionizing radiation is mediated by energy transference. The transference of this energy can damage critical parts of the cell directly or indirectly by formation of free radicals (such as the hydroxyl radical). The primary targets are cellular and nuclear membranes and DNA.17
Long-term effects of radiation exposure include the formation of cancer and wound healing deficits. These have been studied in various venues including exposure to tanning beds which have been linked to an increase in melanoma in young women of up to 75%. These changes are thought to be due to a defect in the p53 tumor suppressor pathway. Children are particularly at risk for radiation-induced injuries as they have a proportionally larger amount of replicating cells and will live long enough to see the effects of radiation, which can have upwards of a 30-year latency period.18
Localized injury
In a localized injury a relatively small part of the body is affected without significant systemic effects.19 The skin and subcutaneous tissue alone may be involved following exposure to low-energy radiation. Exposure to high-energy radiation may injure deeper structures.
One of the most closely studied local effects of radiation injury involves the treatment of breast cancer. It is well known that radiation therapy improves postmastectomy outcomes in women with multiple nodal involvement. This outcome comes at a cost as evidenced by increased rates of capsular contracture, soft tissue fibrosis, and an overall poorer aesthetic outcome. Spear et al. reported significantly increased rates of tissue contracture, hyperpigmentation, and asymmetry following all types of reconstruction paired with radiation.20 This local tissue destruction does not abate with time and has changed the face of breast reconstruction to avoid tissue expanders following treatment with radiation.
The acute radiation syndrome
Neurovascular syndrome
An exposure to a dose of 15–30 Gy or greater can cause an immediate total collapse of the vascular system superimposed on the aforementioned syndromes. This may be due to the massive release of mediator substances, nitric oxide abnormalities or destruction of endothelium.13 This syndrome can progress rapidly with variable neurological symptoms, respiratory distress, cardiovascular collapse and death.