Chapter 49 Mitigation of burn-induced hypermetabolic and catabolic response during convalescence
![]() Access the complete reference list online at http://www.expertconsult.com
Access the complete reference list online at http://www.expertconsult.com
Background
Advances in burn management and critical-care have greatly improved acute outcomes following severe burn injuries in recent decades. This has led to an increased focus on measures to improve long-term outcomes by enhancing rehabilitation and reintegration of burn survivors back into fulfilling and productive roles in society. Long-term debilitation following severe burns results from a combination of physical and psychological factors, including persistent hypermetabolism and physiological derangements, severe skeletal muscle wasting, deformity, scar contracture, pain and itch, limb amputation, multiple operative interventions over the course of years, and psychological and social factors related to loss, disfigurement, identity, and bereavement. Burn team scientists and clinicians have barely begun to gain knowledge into what the long-term quality of life for these survivors can be.1,2 Rehabilitative challenges for such children are numerous, and the best methods of achieving good outcomes in children with severe burns are still being developed.3
Despite the similarities in treatment of pediatric and adult burns, pediatric injuries present unique challenges, both at the time of acute treatment and throughout rehabilitation. Increased experience and new data, gathered in large part from courageous young survivors, have allowed burn team clinicians and scientists to identify many long-term problems associated with large burns. A major problem during convalescence of the pediatric burn patient is the prolonged hypermetabolic state associated with catabolism and growth delay. Recent gene expression studies have demonstrated that, of the thousands of genes which are altered by a severe burn injury in peripheral blood leukocytes, the expression of 21% of the genes are age-specific.4 Many of these genes play important roles in mitochondrial and immune function. These studies demonstrated that there is a temporal component of the response to burn injury as well, with complete resolution of the genomic response to injury taking up to (and in some cases beyond) 1 year. Although the direct role that these genes play in mediating age-specific manifestations of burn-induced sequelae, on-going studies will improve our ability to personalize treatment in pediatric and adult burn patients.
In response to a severe burn, afferent stimuli are activated causing a hypothalamic thermoregulatory re-set to occur. This results in increased heat production, a faster heart rate and a greater cardiac output, in addition to an exaggerated increase in resting energy expenditure.5 The control and treatment of prolonged postburn hypermetabolism remain an unsolved problem.6 Whereas the cause is still not well understood, catecholamines are the major mediators.7 Catecholamine and cortisol levels can be elevated for up to 1 year post-burn.8 With this elevation in stress hormones, there is a long-lasting increase in resting energy expenditure, glucose production and catabolism. The effect of this hypermetabolic, hypercatabolic state is rapid muscle breakdown.9
The self-catabolism, which is manifested as an increase in protein degradation with a lesser increase in synthesis, persists, despite state-of-the-art nutritional care.10 As a result, the rate of protein degradation continues to exceed that of synthesis. The protein catabolic response to injury leaves patients debilitated for months and severely delays the rehabilitation process. Protein is degraded to provide amino acids for energy as well as building blocks for host defense protein synthesis. Most of the required amino acids are taken from active muscle which serves as a pool for amino acids. The increase in amino acid loss from muscle causes muscle wasting and loss of strength. Severe muscle wasting is closely related to overall morbidity and mortality in the burned patients.
Finally, associated with the prolonged hypermetabolic, hypercatabolic state, there is also reduced bone formation, resulting in severe osteopenia or osteoporosis11 as well as linear growth retardation.12–14 This may partly be caused by the continuous elevation in endogenous glucocorticoids that decrease osteoblasts on the mineralization surface of bone, blocking of osteoclastogenesis leading to low bone turnover and bone loss, and a reduced synthesis of vitamin D from skin from burned patients.15
Mitigation of hypermetabolism
Propranolol
Herndon et al. proposed that beta-blockade would mitigate the catecholamine driven hypermetabolic response.16 Their initial study demonstrated that propranolol, given to decrease severe burn-induced tachycardia, attenuates catabolism of skeletal muscle, reduces resting energy expenditure, and decreases hypermetabolism during the acute hospitalization period in severely burned children.16 This mitigation of the catabolic response is associated with alterations in genes for key proteins, including dynein, heat shock protein 70, and myosin.17 Decreases in free fatty acid availability by inhibition of peripheral lipolysis and reduction of hepatic blood flow through the use of propranolol lead to the reduction of fatty infiltration of the liver.18,19 These studies of short treatment regimens of beta-blockade (2–4 weeks) have been extended up to 2 years. Preliminary analysis demonstrates that reduction in cardiac work is the major benefit noted 6 months following the injury. Long-term improvements in lean body mass, increased bone mineral content, and decreased formation of hypertrophic scar persist as well, indicating that extended treatment of severely burned children with propranolol continues to improve patient recovery. Studies to determine the impact of beta-blockade on muscle strength, cardiopulmonary function, and growth will elucidate whether propranolol in combination with exercise can cause even greater improvements in post-burn recovery.
Mitigation of catabolism
Exercise
Resistance exercise has an established influence on muscle strengthening and muscle protein synthesis. The beneficial effects of resistance training have been well documented in healthy adults, adolescents, and older children.20–24 Ferrando et al. demonstrated in healthy adults that moderate resistance exercise is capable of ameliorating the decreases in skeletal muscle protein synthesis and strength that accompany inactivity.25 The acute stimulatory effects of resistance exercise may last up to 48 h.26
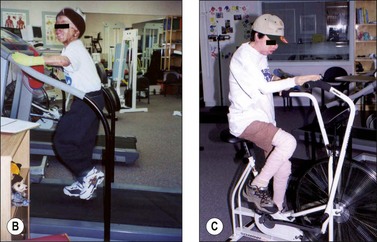
Most of our experience with exercise has been in children and adolescents older than 7 years of age. In burns, resistance exercise alone is also capable of inducing increases in lean mass, muscle strength and aerobic capacity. Suman et al. demonstrated in severely burned children and adolescents that a 12-week exercise program of resistive and aerobic exercise significantly improved lean mass, muscle strength and aerobic capacity relative to standard of care treatment (Fig. 49.1).27,28 We should note that a 12-week exercise program of resistive and aerobic exercise does not reduce REE. However, this is due to the increased lean mass. Furthermore, it should be noted that exercise training in burned children does not further exacerbate REE.27
Exercise and younger children
Because of the difficulties with young children (i.e. under 7 years of age) using the exercise equipment or cooperating in obtaining certain measures, the exercise studies described above were conducted with children ages 7–18. However, as exercise treatment has proven incredibly beneficial, we have now begun a program using music and movement for young children. Movements are chosen to increase strength, flexibility, and endurance. Children enjoy this ‘play,’ and preliminary data indicate the program to be beneficial to overall development and specifically to maintaining or improving joint range of motion beyond standard of care (prescribed occupational–physical therapy exercises).29
Exercise and adults
To our knowledge there is only one published prospective, randomized study involving adults with severe burns and exercise training. One of these studies investigated the efficacy of a 12-week exercise program in producing greater improvement in aerobic capacity in adults with burns relative to the usual care. This randomized, controlled, double-blinded trial had patients completing a 12-week, 36-session, aerobic treadmill exercise program. Some patients were in the work-to-quota (WTQ) program, and intensified their exercise according to preset quotas. Other participants were in the work-to-tolerance (WTT) program and exercised to their tolerance. Participants completed a maximal stress test at baseline and at the 12 weeks to measure physical fitness. The authors reported that the WTT and the WTQ exercise groups both made significant improvements in aerobic capacity from baseline to 12 weeks. However, the control (usual care) group did not. WTT and WTQ participants demonstrated significantly greater improvements in aerobic capacity in comparison to the usual group patients. The WTT and WTQ groups did not differ significantly from each other with regard to their improvements in aerobic capacity. This very well designed study demonstrated that the aerobic capacity of adult burn can be improved with participation in a structured, 12-week exercise program after injury.30
Anabolic agents
Growth hormone
Anabolic agents studied at our institution have included recombinant human growth hormone (rhGH), and oxandrolone, a synthetic testosterone analogue. Both have shown promising results, significantly improving growth and muscle gain following severe burns in children.31 However, a multicentre trial of adult critical-care patients reported increased mortality in patients treated with growth hormone,32 and its use is presently therefore only considered in children.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree