Principles of Tendon Transfers
Douglas M. Sammer
INTRODUCTION
A tendon transfer is the re-routing of a functioning muscle-tendon unit (MTU) (Table 80.1) to a new insertion, in order to restore a function that has been lost. Tendon transfers were first developed in the 19th century to restore ambulation in patients with poliomyelitis. During the subsequent World Wars, thousands of soldiers returned home with upper extremity nerve injuries.1 This influx of patients with upper extremity nerve palsies coincided with the development of hand surgery as a surgical specialty. Over the ensuing decades, tendon transfer techniques were adapted and refined for use in the upper extremity by pioneers Bunnell, Boyes, Brand, Burkhalter, Riordan, Zancolli, and others.
Today, the most common indication for a tendon transfer in the upper extremity is a nerve injury that has no potential for recovery.2 This includes irreparable injuries like nerve root avulsions, failed nerve repairs or reconstructions, or nerve injuries that present too late for recovery due to motor end-plate fibrosis. Other common indications include loss of tendon or muscle substance from trauma, tendon rupture (such as in rheumatoid arthritis), and central neurologic deficits (e.g., spinal cord injuries, stroke, and cerebral palsy).3 Although historically important, leprosy, a mycobacterial granulomatous disease that affects the peripheral nerves, is a rare indication for tendon transfer today.4
PRINCIPLES OF TENDON TRANSFER
Over the last century, a number of principles have been established to guide the performance of tendon transfers. Although adhering to these guidelines does not guarantee success, to ignore them inevitably results in failure.
Supple Joints
Often, patients with upper extremity nerve palsies will present with stiff joints. Performing a tendon transfer in this setting will not improve function. Joints must be supple prior to tendon transfer. Hand therapy or surgical release may be required to maximize passive motion in preparation for a tendon transfer. It should be noted that a joint or contracture release should never be performed at the same time as the tendon transfer. The postoperative management of a joint release includes immediate mobilization and prolonged rehabilitation in order to restore passive motion, whereas a tendon transfer must be immobilized for 3 to 4 weeks to allow tendon healing.
Soft Tissue Equilibrium
The soft tissue bed through which a tendon transfer will be routed should reach “equilibrium” prior to performing the transfer.4 This means that it should be free of edema, inflammation, or scar, so that the tendon transfer can glide freely. A tendon transfer that passes through an inflamed or scarred bed will develop adhesions, reducing the effectiveness of the transfer. At times, it is necessary to route the transfer along a non-standard path in order to avoid an area of scar. If the area of scar is extensive and cannot be avoided, it may be necessary to resurface this area with a fasciocutaneous flap prior to performing the tendon transfer.
Adequate Excursion
The donor MTU should have enough excursion, or linear movement, to achieve the desired motion at the target joint. In other words, the excursion of the donor MTU should be equal to or greater than that of the MTU it is replacing. A good rule of thumb is that the extrinsic finger flexors have approximately 70 mm of excursion, the extrinsic finger extensors have approximately 50 mm of excursion, and the extrinsic wrist motors have approximately 30 mm of excursion.5
Unfortunately, it is not always possible to match donor and recipient excursion. In some cases, the tenodesis effect can be employed by the patient to augment the effective excursion of the donor MTU. For example, the flexor carpi radialis (FCR) is often transferred to the extensor digitorum communis (EDC) to restore finger metacarpophalangeal (MCP) extension. However, the FCR only has 30 mm of excursion, whereas the EDC normally has 50 mm of excursion. The excursion of the FCR is therefore inadequate to fully extend the MCP joints. The patient can overcome this lack of excursion via the tenodesis effect, by simultaneously flexing the wrist and extending the fingers. Wrist flexion increases the distance between the origin and insertion of the tendon transfer, resulting in greater effective excursion and full MCP extension.
Appropriate Strength of Donor
The strength of the donor MTU should be matched to that of the MTU whose function is being restored. This means that the donor MTU must be strong enough to achieve the desired movement. A weak donor MTU will not be able to move the target joint through a functional range of motion, particularly if there is any stiffness, or if there is a strong antagonist. The palmaris longus (PL), for example, does not have adequate strength to power wrist extension. On the other hand, an excessively strong donor MTU results in muscle imbalance and abnormal posture. A transfer of the brachioradialis (BR) to the extensor pollicis longus (EPL), for example, would result in an extension contracture or an abnormal position of the thumb at rest.
When considering potential donor MTUs for transfer, it is more practical to compare relative muscle strength than it is to compare absolute muscle strength.2 The strongest donor MTUs are the BR and the flexor carpi ulnaris (FCU), which each have a relative strength of 2 units. The FCR, the wrist extensors, the finger flexors, and the pronator teres (PT) each have a relative strength of 1 unit. The finger extensors are weaker, with a relative strength of 0.5 units each. The weakest donor MTUs are the polmaris longus (PL) and the thumb extensors and abductors, each of which has a relative strength of 0.1 units. Ideally, the relative strength of the donor MTU should match that of the recipient MTU.
It is also important to choose a donor MTU that has not been weakened by injury or denervation. In general, a donor MTU will lose up to one grade of motor strength simply by being transferred.6 In some situations, such as brachial plexus palsy, the availability of donor MTUs may be severely limited. Although it can be tempting to use a donor MTU that has recovered function after initial denervation or injury, this should be avoided if at all possible.
Expendable Donor
It is essential to consider the potential functional deficit that will be created by a tendon transfer. It is of little use to restore one function but lose another equally important function. Fortunately, there is ample redundancy built into the hand and forearm. For example, there are two wrist flexors and three
wrist extensors. The FCR or the FCU can be transferred without losing wrist flexion, and two of the three wrist extensors can be transferred without compromising wrist extension. The PL is completely redundant, and the extensor indicis proprius (EIP) and extensor digiti minimi (EDM) are excellent donors whose harvest results in minimal donor deficit. In addition, each finger has two flexors, the flexor digitorum profundus (FDP) and flexor digitorum superficialis (FDS). The FDS is often used as a donor MTU, and the finger retains flexion via the intact FDP.
wrist extensors. The FCR or the FCU can be transferred without losing wrist flexion, and two of the three wrist extensors can be transferred without compromising wrist extension. The PL is completely redundant, and the extensor indicis proprius (EIP) and extensor digiti minimi (EDM) are excellent donors whose harvest results in minimal donor deficit. In addition, each finger has two flexors, the flexor digitorum profundus (FDP) and flexor digitorum superficialis (FDS). The FDS is often used as a donor MTU, and the finger retains flexion via the intact FDP.
TABLE 80.1 ABBREVIATIONS USED | ||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Straight Line of Pull
A tendon transfer that has a direct path to its insertion is most effective. Any direction change or pulley decreases the force of the transfer. However, there are instances in which a direct line of pull is not ideal. For example, a PT to extensor carpi radialis brevis (ECRB) transfer is commonly performed to restore wrist extension in patients with radial nerve palsy. The transfer is typically performed in an end-to-end fashion, which creates a straight line of pull. However, if there is a possibility of ECRB recovery in the future, the PT is transferred in an end-to-side fashion into the ECRB tendon. Although this results in an indirect line of pull, the end-to-side insertion allows the ECRB to participate in wrist extension if it recovers function in the future.7 In other situations, the required line of pull cannot be achieved without a direction change. For example, opponensplasties are routed from the level of the pisiform toward the abductor pollicis brevis (APB) insertion, a line of pull that produces thumb opposition. In some cases, this line of pull cannot be achieved without routing the tendon transfer around a pulley. Although this direction change weakens the transfer, it is necessary to achieve opposition.
Synergy
The original function of the donor MTU should be synergistic with the function that is being restored.8 A tendon transfer that is synergistic, as opposed to antagonistic, is easier for the patient to learn to use. Synergy refers to certain movements that are typically combined during routine hand use. For example, wrist extension and finger flexion are synergistic for grasping, whereas wrist flexion and finger extension are synergistic. When a wrist flexor is transferred to restore finger extension (FCR to EDC transfer), the patient can learn to use the transfer without much difficulty. On the other hand, if a wrist extensor were to be transferred to the finger extensors, the patient may have difficulty learning to use the tendon transfer in a natural manner. Although a synergistic transfer is ideal, it is not always possible. Furthermore, it should be noted that certain donor MTUs, such as the FDS, are able to adapt to a new function readily, whether that function is synergistic or not.
Single Transfer, Single Function
Finally, a single tendon transfer should only perform a single function. Attempting to restore multiple functions with a single donor MTU will result in loss of strength and motion. The exception to this rule is that a single donor MTU may be used to restore the same movement in multiple digits. For example, it is acceptable to use the FDS or FCR to restore MCP extension for all four fingers. However, the FDS or FCR would be inadequate to restore both wrist and finger extensions.
BIOMECHANICAL CONSIDERATIONS
The moment arm of a tendon transfer affects how much rotation will occur at the joint, and will affect the torque generated. The moment arm is determined by the distance between the joint axis of rotation and the tendon that crosses the joint. A tendon that passes far from the joint axis of rotation or inserts far from the joint will have a large moment arm, whereas a tendon that lies close to the joint axis of rotation and inserts close to the joint will have a small moment arm. A tendon transfer with a large moment arm will generate greater torque, but at the expense of the arc of motion (greater muscle excursion will be required for a given degree of rotation). A tendon transfer with a smaller moment arm will have an increased arc of motion (less muscle excursion is required for a given degree of rotation), but the transfer will not generate as much torque. In many cases, the insertion point of a tendon transfer is determined by the normal insertion of the recipient tendon. However, there are instances in which the surgeon can choose the insertion point of the tendon transfer. Understanding the concept of the moment arm will help the surgeon determine the optimal insertion point, balancing the needs for joint rotation and generation of torque.
Setting the tension of the tendon transfer is the most critical and difficult part of the operation. Ideally, a tendon transfer should be tensioned in such a way as to maximize actin-myosin overlap. Unfortunately, it is impossible to determine this intraoperatively, although research is being conducted into using laser diffraction intraoperatively to determine the optimum tension for a tendon transfer.9,10 The pragmatic solution is that the tendon transfer should be set at a tension as close as possible to the donor MTUs preoperative resting tension. The donor muscle belly is marked at regular intervals before dividing its insertion, and the tendon transfer is tensioned in such a way as to restore the distance between the intervals. On the other hand, many authors recommend tensioning a tendon
transfer substantially tighter than the donor MTUs resting tension. This is because a tendon transfer tends to loosen or stretch out during rehabilitation. However, a tendon transfer that is set too loosely will not tighten postoperatively.
transfer substantially tighter than the donor MTUs resting tension. This is because a tendon transfer tends to loosen or stretch out during rehabilitation. However, a tendon transfer that is set too loosely will not tighten postoperatively.
RADIAL NERVE PALSY
Radial nerve palsy results in loss of wrist extension, finger MCP extension, thumb abduction, thumb extension, and thumb retropulsion. In addition, patients notice a substantial decrease in grip strength due to the inability to stabilize the wrist during grip. Loss of supinator function is compensated by the biceps brachii and by shoulder rotation. From a sensory standpoint, the loss of sensibility is not critical. Furthermore, there is some overlap with the lateral antebrachial cutaneous nerve. Radial nerve palsy can be categorized as high or low. High radial nerve palsy is a nerve injury proximal to the elbow, in which all of the above functions are lost. Low radial nerve palsy, on the other hand, occurs with an injury distal to the elbow, in which only the posterior interosseous nerve (PIN) is injured. The BR remains intact, and wrist extension is preserved because the branch to the extensor carpi radialis longus (ECRL) arises proximal to the take-off of the PIN (innervation to the ECRB is variable). The goals of tendon transfer are restoration of finger MCP extension, thumb extension and radial abduction, and wrist extension in cases of high radial nerve palsy.
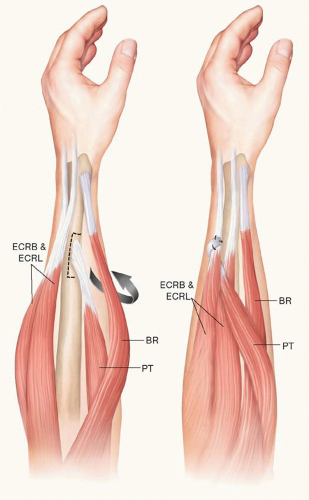
All of the median and ulnar nerve innervated MTUs may be considered potential donors for tendon transfer in patients with radial nerve palsy. Although many different sets of tendon transfers have been described for radial nerve palsy, the PT to ECRB transfer for restoration of wrist extension is nearly universal (Figure 80.1). This transfer results in minimal, if any, donor deficit, because the transferred PT continues to act as a forearm pronator after transfer. Insertion on the ECRB as opposed to the ECRL is preferred, in order to minimize radial deviation of the wrist. This transfer is typically performed in an end-to-end fashion. However, if there is potential for recovery of radial nerve function, the transfer is performed in an end-to-side fashion, allowing the ECRB to contribute to wrist extension should it become reinnervated (Figure 80.1). In fact, the end-to-side PT to ECRB transfer can be used as an “internal splint” to restore wrist extension while the radial nerve is recovering.7,11,12
Finger MCP extension is restored by transfer of the FCR, FCU, or FDS to the EDC. Although the FCU transfer was one of the first described and is still used today (Figure 80.2), the FCR and FDS transfers are preferred over the FCU by many surgeons. This is because transfer of the FCU results in loss of the functionally critical “dart-throwing motion.” In addition, in the wrist without a functioning ECU, transfer of the FCU removes the only remaining ulnar-sided wrist motor, leading to wrist imbalance and radial deviation. The FCR is a good donor for restoration of finger MCP extension. It is expendable (wrist flexion is maintained by the FCU), and its use does not result in loss of the dart-throwing motion or in radial deviation. The primary limitation of the FCR is that its excursion (approximately 33 mm) is inadequate to provide full MCP extension. However, the tenodesis effect (wrist flexion with concomitant MCP extension) can be used to bring the MCP joints into full extension after an FCR to EDC transfer and is easily learned by the patient. The FDS is also a good donor for restoration of finger MCP extension. It has excellent excursion (approximately 70 mm), and flexion of the donor finger is preserved by the remaining intact FDP. The primary disadvantage of the FDS to EDC transfer is that some grip strength is lost. In the patient with a fused wrist who cannot employ the tenodesis effect, the FDS is the preferred donor MTU.
For restoration of thumb extension and radial abduction, the PL or an FDS can be transferred to the EPL (Figure 80.3). The EPL is usually re-routed and allowed to lie in a more radial and volar position. This results in restoration of radial abduction as well as extension, at the expense of retropulsion. Alternatively, the FDS can be transferred to both the EPL and the EIP in order to restore simultaneous thumb and index finger extension, a functionally useful combination of movements.
Over the years, three “standard” sets of tendon transfers have been established for reconstruction of radial nerve palsy: the FCR transfer,12,13,14 the FCU transfer,15,16 and the superficialis transfer.17,18 All three sets of transfers employ the PT to ECRB transfer for restoration of wrist extension. The FCR transfer involves FCR to EDC transfer for MCP extension, and PL to re-routed EPL transfer for thumb extension. The FCU transfer is the same, except the FCU is used in place of the FCR to restore MCP extension. Finally, in the superficialis transfer, the ring FDS is transferred to the EPL and EIP for simultaneous thumb and index extension, and the long FDS is transferred to the remaining digital extensors. The FCR is transferred to the abductor pollicis longus and EPB to restore thumb MCP extension and radial abduction. The author’s preference is to use the FCR transfer in patients with intact wrist flexion and the superficialis transfer in patients who have undergone a wrist arthrodesis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree