5 Principles of internal fixation as applied to the hand and wrist
Synopsis
 Most minimally or nondisplaced fractures can be managed nonoperatively.
Most minimally or nondisplaced fractures can be managed nonoperatively.
 Careful preoperative planning facilitates safe and expeditious surgery.
Careful preoperative planning facilitates safe and expeditious surgery.
 Ligamentotaxis relies on the application of linear traction to indirectly reduce fragments via the intact periosteum and soft tissues.
Ligamentotaxis relies on the application of linear traction to indirectly reduce fragments via the intact periosteum and soft tissues.
 A myriad of fracture fixation options are available; selecting the most appropriate depends on a careful assessment of the fracture and patient related factors.
A myriad of fracture fixation options are available; selecting the most appropriate depends on a careful assessment of the fracture and patient related factors.
 Postoperative care should allow for early mobilization if fixation permits.
Postoperative care should allow for early mobilization if fixation permits.
Introduction
Fracture care was significantly advanced in the 20th century with the introduction of new techniques and instrumentation for internal and external fixation.1 Today’s capable hand surgeon must be well versed in the spectrum of available techniques of fracture fixation to provide optimum care for the myriad of bony injuries that occur within the purview of a hand surgery practice. Fixation of fractures in the hand is notoriously difficult given the relatively small size of the osseous structures and complexity of the surrounding anatomy.2 The aim of this chapter is not to review every possible technique of fracture fixation in the hand, but rather, to present basic concepts and general techniques useful in routine fracture care.
Much of the credit for these advances in fracture management should go to the Arbeitsgemeinschaft fur Osteosynthesefragen (AO) who devised a set of principles (Table 5.1) that, in its modified form, provides the basic tenets that underlie appropriate fracture care.3
Table 5.1 Arbeitsgemeinschaft fur Osteosynthesefragen (AO) principles
| Anatomical fracture reduction |
| Appropriate stability of the fixation construct |
| Preservation of blood supply and soft tissue attachments to fracture fragments |
| Early and safe mobilization |
Patient selection
Host factors
Certain host factors imply an increased susceptibility to wound healing problems or infection. Systemic factors include: diabetes mellitus,4 an immunocompromised state, advanced age, and smoking, amongst many others. Local factors include: skin quality, volume/quality of soft tissues available for closure, type of hardware elected, and tension across the wound. Failure to recognize and address these factors may result in compromised outcomes. Patients with elevated risk for wound problems should be counseled accordingly and managed with alternative strategies where appropriate.
Preoperative imaging
1. Location of fracture (articular, metaphyseal, diaphyseal)
2. Pattern (transverse, oblique, spiral)
5. Angulation (sagittal, coronal, and axial (rotational) planes)
6. Potential deforming forces acting across the fracture site.
Treatment/surgical technique
Fracture reduction
Fracture reduction may be obtained by numerous means. If done in a closed fashion, this reduction is usually in the form of pulling linear traction across the fracture site. This utilizes the phenomenon of ligamentotaxis,5,6 whereby any intact periosteum and/or ligaments help realign attached bony fragments as they are stretched. When open reduction is elected, reduction is obtained usually through a combination of external manipulation and instruments placed within the fracture site. The reduction may be held with reduction forceps or provisional Kirschner wires. The concept of reducing the number of fragments by temporary or final fixation of fragments to other fragments is critical in achieving a satisfactory reduction in the face of comminution. Forceps or wires used for temporary fixation should be carefully thought out so as to not interfere with the planned definitive fixation.
Intraoperative imaging
Fluoroscopy provides a valuable adjunct to many fracture fixation surgeries. A complete review of fluoroscopic physics and principles is beyond the scope of this chapter, but a few points are worth mentioning. For upper extremity surgery, either an image intensifier or a “mini” fluoroscopic unit may be employed. For the vast majority of hand surgery cases a “mini” fluoro provides adequate visualization with greater mobility and less radiation.12–15
The region being examined should always be centered on the detector of the fluoroscopic unit to minimize the distortion from the “parallax” effect. Multiple views are helpful to determine fracture reduction or hardware position in all planes. It may also be helpful to orient the beam directly down a placed K-wire or screw to precisely visualize its placement. Specific knowledge of certain anatomic regions may also be helpful. For instance, in the distal radius, inclining the wrist approximately 20–30° from a true lateral can provide better visualization of the cortex of the lunate facet to evaluate for screw penetration into the radiocarpal joint.16 Live, dynamic fluoroscopy may be useful to examine for stability across a fracture site with controlled motion or in other, select instances.
Fixation options
Absolute versus relative stability
Key concept
Absolute versus relative stability
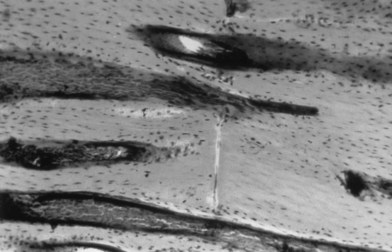
Bone healing following fracture fixation depends on the stability of the fixation technique chosen. With absolute stability, very rigid, internal fixation is utilized. This typically is in the form of lag screws or compression plates. This requires anatomical reduction of fracture fragments and is often the goal with articular fractures and simple diaphyseal fractures. Interfragmentary compression, as discussed below, facilitates healing with this type of fixation. Typically, absolute stability is possible only with simple fracture patterns or with minimally comminuted fractures with relatively large comminuted fragments (i.e., a “butterfly” segment). Primary bone healing with absolute stability is achieved histologically with “cutting cones” (Fig. 5.1) that facilitate direct healing of one fragment to another. No fracture callus is observed.
Interfragmentary compression
Interfragmentary compression is a critical component of fixation when the surgeon attempts to achieve absolute stability.17,18 This compression, when combined with anatomical reduction, leads to microscopic interdigitation of fracture ends, thus minimizing the distance required for cells to travel from one side of the fracture to the other. This may be achieved via a variety of methods discussed below, including lag screws, compression plates, and tension bands. Interfragmentary compression may be detrimental in certain situations. For instance, in highly comminuted fractures, overzealous compression may lead to excessive shortening.
Kirschner wires
Kirschner wires (K-wires) are simple, yet versatile tools to assist with fracture fixation. They may be inserted in either a closed or open fashion and appropriate insertion causes minimal tissue trauma. They may be implemented either as temporary or definitive fixation (Fig. 5.2).19 When used for definitive fixation, relative stability is generally attained and healing occurs with callus formation. Insertion of K-wires may be either directly across a fracture site or in an intramedullary fashion. The main limitation of K-wires is that they do not allow for interfragmentary compression and may loosen over time, leading to implant migration.