CHAPTER 46 Primary otoplasty and reconstruction
Physical evaluation
• Overall size and shape. Evaluate the overall size/shape of the ear: Is it prominent with an otherwise normal size and configuration, or are there abnormalities in addition to the prominence? Excessively large ears, Stahl’s ears, cryptotia, underdeveloped shell-like helical rims, postoperative deformities, cauliflower ears, elongated lobules or earring-related deformities are noted.
• Upper  . Evaluate the upper
. Evaluate the upper  : Is the upper pole prominent, is the antihelix/superior crus of the triangular fossa well formed, and is the helical rim well developed?
: Is the upper pole prominent, is the antihelix/superior crus of the triangular fossa well formed, and is the helical rim well developed?
• Middle  . Evaluate the middle
. Evaluate the middle  : Is the concha overly deep or protruding?
: Is the concha overly deep or protruding?
• Lower  . Evaluate the lower
. Evaluate the lower  (lobule): Is the lobule prominent? It is important to note that even if the lobule is not particularly prominent on initial examination, it may be excessively prominent once the upper
(lobule): Is the lobule prominent? It is important to note that even if the lobule is not particularly prominent on initial examination, it may be excessively prominent once the upper  of the ear has been corrected intraoperatively.
of the ear has been corrected intraoperatively.
• Asymmetry. Asymmetry is noted, mostly because patients and families will always comment on it. In asymmetric cases it is almost always preferable to operate on both ears rather than attempt setting back only the prominent ear to match the less prominent ear.
Technical steps
Standard otoplasty for prominent ears of normal size
• Incision. The incision is made in the retroauricular crease.
• Dissection. No skin is excised except a small triangle from the medial surface of the lobule (not from the retrolobular skin), taking care to preserve enough tissue for a normal earlobe and retrolobular sulcus. The cartilage is exposed on its posterior surface and soft tissue is excised from deep to the concha. In the region of the earlobe, deep dissection is performed under the concha in preparation for lobule repositioning.
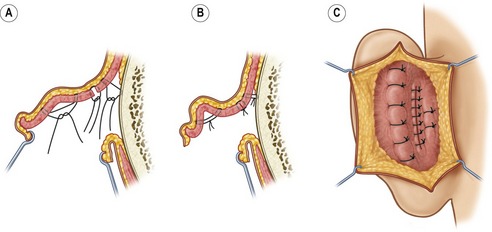
• Correction. (Fig. 46.1). Mustarde concha-scapha and triangular fossa-scapha sutures are placed using 4-0 clear Nylon sutures. The number of sutures depends on how far into the middle  of the ear the antihelical deficiency extends. These sutures are used to create a soft curvature to the antihelix and no attempt is made to correct the prominence at this point. A small crescent of cartilage (3 mm or less at its widest point) is excised from the posterior wall of the concha, at its junction with the conchal floor. The defect is closed primarily using numerous 4-0 Nylon interrupted sutures. A conchal setback is performed using a single 3-0 PDS suture between the concha and the mastoid fascia. This combination of a small conchal resection and a small conchal setback avoids the distortion of a large conchal resection and the unreliability of a large conchal setback. The earlobe is repositioned employing a method similar to that described by Gosain. Two 5-0 PDS sutures are placed which not only approximate the skin where the skin excision was performed, but incorporate a bite of cartilage on the undersurface of the concha (Fig. 46.2). The sutures are tightened until the lobule is slightly over-corrected.
of the ear the antihelical deficiency extends. These sutures are used to create a soft curvature to the antihelix and no attempt is made to correct the prominence at this point. A small crescent of cartilage (3 mm or less at its widest point) is excised from the posterior wall of the concha, at its junction with the conchal floor. The defect is closed primarily using numerous 4-0 Nylon interrupted sutures. A conchal setback is performed using a single 3-0 PDS suture between the concha and the mastoid fascia. This combination of a small conchal resection and a small conchal setback avoids the distortion of a large conchal resection and the unreliability of a large conchal setback. The earlobe is repositioned employing a method similar to that described by Gosain. Two 5-0 PDS sutures are placed which not only approximate the skin where the skin excision was performed, but incorporate a bite of cartilage on the undersurface of the concha (Fig. 46.2). The sutures are tightened until the lobule is slightly over-corrected.
• Endpoint. Otoplasty is all about the endpoint. How do you know how tight to make the Mustarde sutures? How do you know how tight to tie the Furnas conchal-mastoid sutures. How do you know how sharp to make the antihelical fold? The answers to these questions are apparent if the surgeon remembers what the ear is supposed to look like: (1) When viewed from the front, the helical rim should be visible, poking out from behind the antihelix. (2) When viewed from the side, the contours should be round and soft, never sharp. (3) Finally, and most helpful to the surgeon who is sitting behind the patient intraoperatively: When viewed from behind the patient, the contour of the helical rim should be a straight line, not a “C” or a “hockey stick” or any other shape. If there is one lesson to take from this chapter, this is it. The final position of the ear should be over-corrected minimally to allow for some relapse, but not enough to create an unsatisfactory result if no relapse should occur.
• Closure. The skin is approximated using 5-0 plain gut, without excising more skin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree