I. PRESSURE SORE DIAGNOSIS AND MANAGEMENT
A. Definition: Necrosis and ulceration of tissue from pressure
B. Etiology/mechanism
1. *Tissue ischemia from external pressures exceeding the closing pressure of nutrient capillaries (32 mmHg) for a prolonged duration
2. *Pressures exceeding 70 mmHg for 2 hours result in irreversible ischemia
3. Shear forces can induce tissue ischemia: Vessel stretch leading to thrombosis
4. Friction may cause epidermal injury (e.g., during transfers)
5. Excess moisture especially from incontinence: Skin maceration and increased pressure sore risk
6. Ischemia-reperfusion cycle has being implicated
7. Decreased autonomic control leading to spasm, loss of bladder and bowel control, and excessive sweating
8. Advanced age: Decreased skin tensile strength
9. Malnutrition: Important to supplement calories and vitamins
10. Sensory loss: Inability to experience discomfort or tissue ischemia
C. Epidemiology/biology/natural history
1. Prevalence
a. 15% in general acute care setting
b. 15% in long-term care setting
c. 15% in home care setting
2. Incidence
a. 0.5% to 38% in general care settings
b. 2% to 24% in long-term care settings
c. 0% to 17% in home care settings
3. Over 60% of patients with pressure sores are >70 years of age
4. Other risk factors
a. Cerebrovascular disease
b. History of pressure sore
c. Immobility (debility or paralysis)
d. Poor nutritional status
e. Low BMI
f. End-stage renal disease
g. Small vessel occlusive disease: Diabetes mellitus and smoking
h. Sensory loss
i. Decreased level of consciousness
5. Chronic polymicrobial colonization (count >1 × 105)
a. Staphylococcus aureus and Streptococcus are most common bacteria
b. Decreased growth factor level
c. Increased matrix protease activity
6. Chronic wound: Possibility of malignant degeneration (Marjolin’s ulcer)
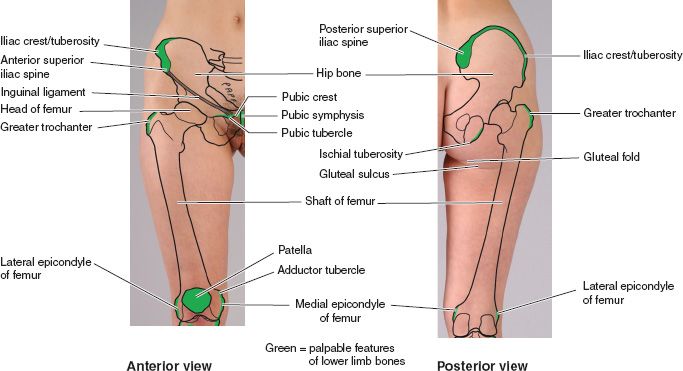
D. Surface anatomy (Fig. 50-1)
1. Depends on patient positioning, which depends on patient’s underlying condition
a. Supine: Sacral and heel sores most common
______________
*Denotes common in-service examination topics
Figure 50-1. Surface projection and palpable features of pelvis and femur which are common locations of pressure ulcers. (From Moore KL, Dalley AF, Agur AM, eds. Clinically Oriented Anatomy. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
b. Seated: Ischial sores most common
c. Overall ischial tuberosities are the most common site (about 30%)
E. Prevention
1. Moisture: Bladder/bowel hygiene, avoiding soilage
2. Spasticity
a. Control of spasticity facilitates proper positioning
b. Baclofen or diazepam treatment
c. Physical Rehabilitative Medicine consult
3. Proper pressure distribution
a. Air fluidized, low air-loss and alternating air cell mattresses (work best with head of bed less than 45 degrees)
b. Proper wheelchair cushions when sitting
4. Pressure relief protocols
a. Reposition patients every 2 hours
b. Patients in wheelchairs should be or should lift themselves for >10 seconds every 10 minutes
F. Diagnosis/work-up
1. Laboratory studies and imaging
a. Complete blood cell (CBC) count with differential
b. Glucose/hemoglobin A1c
c. Albumin/pre-albumin
d. Erythrocyte sedimentation rate (ESR)/C-reactive protein (CRP)
e. MRI
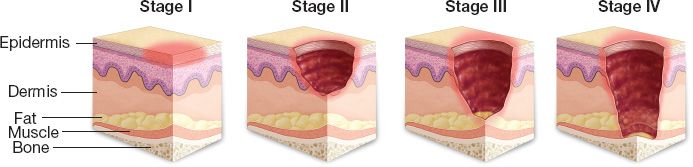
2. *Stages defined by the National Pressure Ulcer Advisory Panel (NPUAP) (Fig. 50-2)
a. Stage I: Nonblanchable erythema present for >1 hour after pressure relief. Skin intact.
b. Stage II: Partial thickness skin loss
c. Stage III: Full thickness skin loss into subcutaneous tissue but not through fascia
d. Stage IV: Through fascia into muscle, bone, tendon, or joint
e. Unstageable: If eschar is present, wound cannot be staged until fully debrided.
3. Muscle is more susceptible to ischemia than skin: Muscle necrosis may have occurred with skin erythema as the only sign
Figure 50-2. The International National Pressure Ulcer Advisory Panel Pressure Ulcer Stages/Categories. Stage I: Non-blanchable erythema. Intact skin with non-blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its color may differ from the surrounding area. The area may be painful, firm, soft, warmer or cooler as compared to adjacent tissue. Stage II: Partial thickness. Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled or serosanginous filled blister. Presents as a shiny or dry shallow ulcer without slough or bruising. Stage III: Full thickness skin loss. Subcutaneous fat may be visible but bone, tendon or muscle are not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling. The depth of a Stage III pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have (adipose) subcutaneous tissue and Stage III ulcers can be shallow. In contrast, areas of significant adiposity can develop extremely deep Stage III pressure ulcers. Stage IV: Full thickness tissue loss. Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present. Often includes undermining and tunneling. The depth of a Stage IV pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have (adipose) subcutaneous tissue and these ulcers can be shallow. Stage IV ulcers can extend into muscle and/or supporting structures (e.g., fascia, tendon or joint capsule) making osteomyelitis or osteitis likely to occur.
4. Nutritional status: Serum albumin <3.5 mg/dL is a risk factor for developing pressure sores
5. Osteomyelitis (OM): Presence of bone infection must be determined. Initial studies include:
a. ESR, CRB, and CBC
b. MRI can identify OM and extent of disease. However, bone biopsy remains the gold standard for diagnosis.
6. Identify contractures and spasticity in paraplegic and quadriplegic patients: Patient may need physical medicine consult
7. Assess bowel/bladder routine and continence
8. Assess motivation and support structure
a. Adherence to pressure relief protocols
b. Adherence to wound care routines
c. Maintenance of adequate nutrition
d. Participation in risk factor modification (e.g., smoking cessation)
G. Treatment overview
1. Goals
a. Avoid invasive infection
b. Contain size of existing wound
c. Avoid new pressure sores
d. Wound closure. Surgical closure is not attainable in all patients (e.g., poor surgical candidates, nonoptimal social circumstances, etc.). Make management plan accordingly.
2. Management
a. Debridement of nonviable tissues
b. Wound care
c. Antibiotic therapy
d. Surgical closure when possible
3. Stage I and II wounds
a. Stage I: Wound dressing to prevent dessication and protect tissue
b. Stage I and II
i. Pressure relief with frequent patient repositioning
ii. Appropriate pressure dispersion
i. Silver sulfadiazine ointment (Silvadene) to prevent bacterial invasion
ii. Impregnated gauze (xeroform and petrolatum gauze) are useful alternatives for sulfa-allergic patients
4. Stage III and IV wounds
a. History and physical
i. Identify the specific etiology of the wound
ii. Identify risk factors present
iii. Assess current wound care regimen
iv. Assess social circumstances (e.g., available help/support)
v. Assess level of activity and mobility
vi. Assess type of bed/wheelchair cushion
vii. Investigate previous surgical and nonsurgical treatments
viii. Assess wound characteristics (stage, size in three dimensions, palpable bone, tissue present in wound bed, presence of bacterial invasion, nature and volume of exudate, and integrity of tissue around the wound)
ix. Assess history of wound and how it has been progressing with current dressing regimen
b. Modify risk factors
i. Treat spasticity when present
ii. Eliminate excess moisture with bladder/bowel regimen or diversion (e.g., Foley catheter/diverting ostomy)
iii. Eliminate pressure (specialty mattresses, cushions, and pressure relief protocols)
iv. Optimize nutritional status
c. Assess for OM
i. CBC, CRP, and ESR (>100 is diagnostic for OM)
ii. MRI (may confirm OM when ESR is 50 to 100, shows extent of disease for surgical and overall treatment planning)
iii. Bone biopsy for culture and pathology is diagnostic standard
d. Surgical debridement
i. Excise devitalized tissue and bone
ii. Resected bone is sent to microbiology and pathology
iii. Wound care regimen initiated
iv. Postdebridement 6-week outpatient IV antibiotic course: Initially broad-spectrum and then tailored when bone culture results available
e. Preparing for wound closure
i. Appropriate wound care regimen
ii. Assessments of the wound to ensure healing is taking place (e.g., there is healthy granulation and wound shrinkage)
iii. Consider becaplermin (Regranex); recombinant PDGF. Improves ability to achieve wound closure. Need 6-week course of treatment after antibiotic course.
f. Definitive closure
i. Use well-vascularized tissue
ii. May allow wound to heal secondarily if reasonably small, healing well and aligns with patient preference
II. WOUND DRESSINGS (STAGE III/IV SORES)
A. Goals
1. Achieve warm, moist, and clean environment for wound healing
a. Desiccated wound needs hydration
b. Wound with excess drainage needs absorbent
c. Wound with necrosis needs debridement
d. Infected wound needs needs antimicrobial
B. Wet-to-moist dressing
1. With normal saline or silver sulfadiazine and mesh gauze
2. In clean wounds: Prevents desiccation for optimal fibroblast and keratinocyte development and epithelial migration
1. Chemical: Enzymatic agents such as collagenase
a. Liquefy devitalized tissue
2. Autolytic: Hydrocolloids inner gel forming absorbent layer keeps wound moist
a. Moisture softens devitalized slough
D. Antiseptic dressings
1. Oxychlorosene, Dakin’s solution, and dilute bleach
a. Applied in wet-to-moist fashion
2. Used in heavily contaminated wounds to decrease bacterial counts
a. Acetic acid thought to be effective in controlling Pseudomonas
3. Several of these agents have detrimental effects on wound healing (e.g., impair fibroblast proliferation). Switch to other dressings when wound is clean
E. Absorbent dressings, i.e. alginates
1. Hydrophilic gels with ability to absorb up to 20 times their weight
2. Have antimicrobial properties
3. Used in excessively exudative wounds
F. Negative pressure wound therapy
1. No guidelines for role in pressure sore management
2. Appropriate for stage III and IV wounds
3. Contraindicated with OM, necrotic tissue, malignancy, and fistulas
III. SOFT TISSUE INFECTIONS (STAGE III/IV SORES)
A. Local infections
1. Cellulitis, a malodorous wound and purulent discharge
2. Can lead to systemic infections with leukocytosis, fever, and sepsis
B. Obtain specimens after debridement for quantitative bacterial counts, culture, and sensitivity
1. Staphylococcus, Streptococcus, Escherichia coli, and Pseudomonas are most common culprits
2. Mixed aerobic/anaerobic infections not uncommon
C. Treat promptly with drainage, irrigation, debridement, and antibiotics guided by cultures
IV. BONE INFECTIONS (OM)
A. Diagnosis
1. Exposed/palpable bone on initial evaluation: OM until proven otherwise
2. Bone biopsy: Gold standard for diagnosis
3. Obtain bone biopsy during initial evaluation with a rongeur if patient is insensate
4. Bone scans: Not specific for diagnosing OM but can rule out OM if negative
5. MRI
a. 98% sensitivity and 88% specificity in diagnosis of OM
b. Can also use to determine extent of disease
c. Enhancement of bone and marrow in T2 signal
B. Treatment
1. Debridement of devitalized and infected bone
2. A 6-week IV antibiotic course tailored to causative organism
3. When resection is impossible (extension to acetabulum and pubic rami)
a. Flap closure is contraindicated
b. Management is chronic suppressive antibiotics and wound dressings indefinitely
V. PREOPERATIVE AND INTRA-OPERATIVE CONSIDERATIONS FOR WOUND CLOSURE
A. Minimize risks of recurrence
1. Recognize that not all patients are candidates for closure
a. Patients who have not optimized conservative measures such as bowel and bladder regimens and contractures
b. Patients with significant medical comorbidities
2. Optimize nutritional status: Serum albumin of ≥3.5 mg/dL
3. Optimize spasticity management
4. Optimize comorbidities management, for example, glycemic control in diabetics
5. No smoking
6. Optimize bladder/bowel regimen (prevent moisture/soilage): Consider urinary and fecal diversion if bladder/bowel regimen cannot be optimized
7. Establish history of adherence to wound care regimen, pressure relief protocols
8. Motivated patient
a. Mood disorders (not uncommon in pressure sore patients) are detrimental to motivation
9. Social support for the postoperative convalescence when restrictive regimens are in place to protect flap
10. Wound must demonstrate capacity to heal after debridement and treatment with systemic antibiotics. If no wound shrinkage after debridement/antibiotics, or if there are signs of invasive infection (increased drainage, malodor, soft tissue infection), Halt plans for closure and reevaluate: CBC, ESR, CRP, bone biopsy, and MRI
11. Postdebridement monitoring should include
a. Weekly ESR and CRP and CBC during antibiotic treatment
b. Evaluate the trend of these test results before embarking on closure to ensure ESR is not elevated or trending up
12. Patient should be off antibiotics for at least 7 days before closure to get an accurate microbiological assessment of intra-op bone cultures
13. Intra-op
a. Excise entire ulcer and bursa, scar tissue, and soft tissue calcifications
b. Send tissue for quantitative counts, culture, and sensitivities
c. Resect devitalized bone until bleeding bone is encountered
d. Send bone to microbiology and pathology
e. Be careful with partial ischiectomy: Overly radical ischiectomy increases risk of ipsilateral of contralateral recurrence and perineal pressure sores
B. Other considerations for wound closure
1. Need bulk to fill dead space and pad underlying bone with muscle, musculocutaneous flaps, or fasciocutaneous flaps
2. *Preserve lower extremity function in ambulatory patients by using perforator flaps rather than myocutaneous flaps
3. Design large flap to prevent tension after closure and place suture line away from direct pressure
4. Do not violate adjacent flap territories to preserve options for recurrence or development of new pressure sores
5. Rotation and V–Y advancement flaps can be re-advanced if recurrence occurs
6. If possible, bring sensate tissue into the wound for protective sensation
7. In OR, pad all pressure points appropriately: Do not give patient new pressure sore
VI. FLAPS AND OTHER PROCEDURES
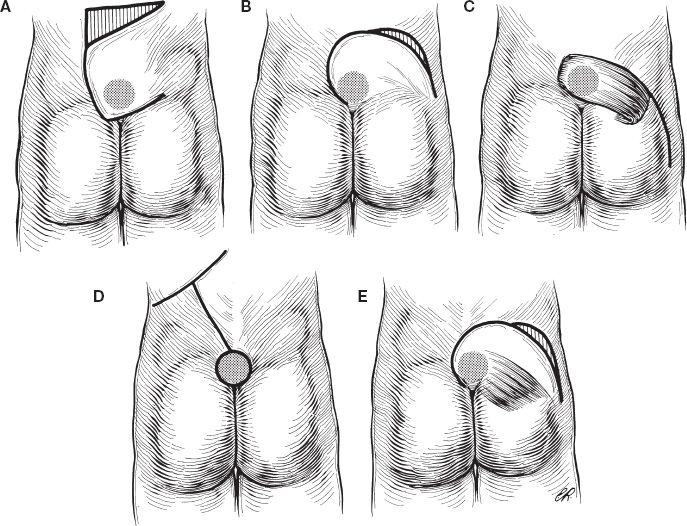
A. Sacral pressure sores (Fig. 50-3)
1. Gluteal flaps (gluteus maximus): Muscle, musculocutaneous flaps, and fasciocutaneous flaps
a. Musculocutaneous and fasciocutaneous flaps can be designed as rotation, V–Y advancement flaps (unilateral or bilateral) and island flaps
b. Mathes type III muscle
c. Blood supply: Superior and gluteal artery off of internal iliac
d. *In ambulatory patients preserve origin and insertion of gluteus maximus
e. Unilateral rotational gluteal musculocutaneous flap
Figure 50-3. Flaps for closure of sacral wounds. A: Transposition cutaneous flap. B: Rotation cutaneous flap. C: Gluteus maximus muscle flap. D: Double cutaneous rotation flap. E: Rotation musculocutaneous flap.
i. Landmarks: Greater trochanter, lateral edge of sacrum, and posterior superior iliac spine (PSIS)
ii. Incision: Arc from sacral wound edge through PSIS through trochanter to ipsilateral ischial tuberosity
iii. Elevate in plane between gluteus maximus and medius detaching muscle from sacral insertion
iv. Preserve inferior/superior gluteal arteries
v. Rotate flap into defect (eliminate dead space)
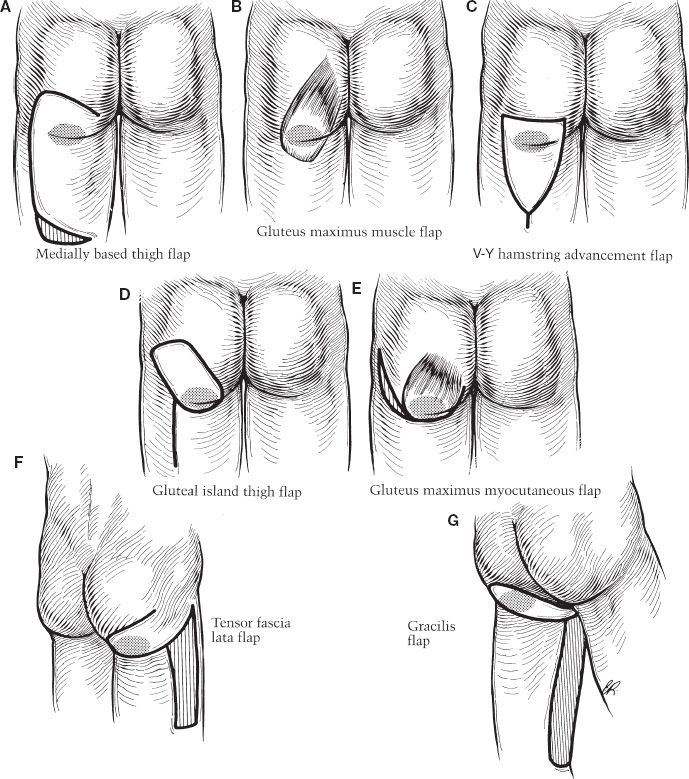
B. Ischial pressure sores (Fig. 50-4)
1. Gluteal flaps (gluteus maximus): Include rotational musculocutaneous and island musculocutaneous flaps
a. Inferior gluteal artery-based rotational musculocutaneous flap
b. Landmarks are PSIS and trochanter
c. Incision: Arc from just superior to the PSIS through trochanter to the ischial wound
d. Divide only insertion of gluteus maximus laterally and inferiorly
e. Elevate at fascial level until mobile enough to rotate into the defect
f. Preserve inferior gluteal artery and sciatic nerve
g. Eliminate dead space
h. *Not appropriate for ambulatory patients
2. Posterior/gluteal thigh flap
a. Fasciocutaneous flap based on descending branch of inferior gluteal artery
b. May be designed as laterally based rotation flap or V–Y advancement flap
c. Rotational posterior gluteal thigh flap
i. Landmarks are ischial tuberosity and greater trochanter
ii. Distal limit is 10 cm above popliteal fossa and width should be approximately 10 cm
Figure 50-4. Flaps for closure of ischial pressure sores. A: Medially-based thigh flap. B: Gluteus maximus muscle flap. C: V-Y hamstring advancement flap. D: Gluteal island thigh flap. E: Gluteus maximus musculocutaneous flap. F: Tensor fascia lata musculocutaneous flap. G: Gracilis musculocutaneous flap.
iii. Incision: Extends from medial aspect of ischial defect inferior to distal limit and then back cut up toward greater trochanter (should not extend more proximal than 10 cm to ischial tuberosity)
iv. Elevate superficial to hamstrings
v. Preserve posterior femoral cutaneous nerve and profunda femoris perforators
vi. Rotate flap into the defect
vii. *May be used in ambulatory patients
C. Trochanteric pressure sores
1. Tensor fascia-lata (TFL) flap: Muscle and musculocutaneous flaps
a. Musculocutaneous flap can be designed as rotation (transposition) or V–Y advancement flaps
b. Muscle only flap will require STSG
c. May need STSG to cover donor defect
d. Mathes type I flap supplied by descending branch of lateral femoral circumflex artery (enters muscle 10 cm inferior to anterior superior iliac spine [ASIS])
i. Pedicle landmarks: A line connecting ASIS to lateral knee
ii. Anterior margin of the flap is 3 cm anterior to pedicle landmark line
iii. Distal extent of flap is junction of proximal two-third and distal one-third of thigh
iv. Incision: Anterior margin of flap through distal limit and back up to trochanteric sore (width should be approximately 10 cm at widest point)
v. Elevate deep to TFL
vi. Transpose into the defect
2. Girdlestone procedure
a. Indicated when there is communication of trochanteric pressure sore with the hip joint
b. This communication may cause pyoarthrosis and is commonly missed
c. Trochanteric pressure sores tend to have small openings with extensive bursas. Thoroughly examine patients to ensure no communication with the joint.
d. Pyarthrosis: Purulent drainage, fever, and signs of sepsis on presentation. Need a high index of suspicion to diagnose.
e. Magnified “coned down” radiographic views of the joint may show OM
f. Arthrogram: May demonstrate communication of pressure sore with the hip joint
g. Treatment: Incision and drainage as indicated, proximal femur resection with antibiotics course followed by flap coverage (to fill the joint space)
h. Operative technique
i. Resect proximal femur
ii. Distally, debride until healthy bone encountered
iii. Proximally, strip all cartilage from acetabulum until cancellous bleeding surface is encountered
iv. Postoperatively: Antispasmodics and abduction pillow to prevent pistoning of femur into the defect
3. Vastus lateralis is the flap most used for coverage after Girdlestone procedure
a. Pedicle is a descending branch of lateral circumflex femoral artery (10 cm distal to greater trochanter)
b. Divide muscle 8 cm proximal to patella
c. Posterior dissection should not cross lateral inter-muscular septum
d. Elevate up to vascular pedicle and transpose
e. May require skin grafting
VII. NONOPERATIVE TREATMENT (STAGE III/IV)
A. For patients with unresectable OM (extension to acetabulum and pubic rami) who are not surgical candidates
B. Goals
1. Prevent invasive infection
2. Prevent wound from enlarging
3. Prevent new wounds
C. For patients with resectable OM who are not surgical candidates
1. Debridement with bone cultures and specimens
2. IV antibiotics and monitoring of CBC, ESR, and CRP
3. Appropriate wound care regimen
4. Pressure relief protocols
5. Appropriate pressure dispersing surfaces
6. Proper bladder/bowel regimen or diversion as appropriate
7. Treatment of spasticity
8. Nutritional optimization
9. Management of co-morbid conditions and long-term follow-up with wound care team
D. For patients with unresectable OM
1. Need all the above
2. Also need chronic suppressive antibiotics monitored by infectious specialists and appropriate wound care regimen
VIII. POSTOPERATIVE CARE (STAGE III/IV WOUND CLOSURES)
A. General considerations
1. Pressure dispersion: for example, air-fluidized mattress
2. Pressure relief protocols
3. Protection of flap from pressure, shear, and friction
4. Optimize nutrition
5. Control spasticity/spasms
6. Bladder and bowel regimen
7. Surgical drains essential
8. Antibiotic treatment if indicated by intra-operative cultures
9. No pressure on the flap/wound bed for 6 weeks
B. Sitting protocol
1. For closed ischial pressure sores
2. *No sitting for 3 to 6 weeks
3. Advance sitting duration over 1 to 2 weeks: Start with 30 minutes twice a day with at least 1 hour in between
4. Advance by 15 minutes a day until 2 hours achieved
5. Evaluate flap after each sitting session for signs of dehiscence or compromise (erythema)
6. Sitting is not resumed until erythema is resolved. Sitting time not increased if erythema persists 30 minutes after a sitting session
7. During each sitting session, the patient must be lifted for >10 seconds every 10 minutes
IX. POSSIBLE COMPLICATIONS (FLAP PROCEDURES)
A. Hematoma
1. May compromise flap viability or be a nidus of infection
2. Evacuate the hematoma
B. Seroma
1. Prevent by filling dead space
2. Place drains or drain percutaneously
C. Infection
1. Reduce risk with perioperative antibiotics
2. If superficial, treat with antibiotics otherwise debridement is required
D. Wound dehiscence
1. Avoid tension with closure
2. Leave sutures in place for 3 weeks
3. If dehiscence is small, manage with wound care otherwise debridement and flap re-advancement
E. Partial flap loss
1. Prevent with proper flap design
2. If small area of flap loss, manage with wound care otherwise debride
F. Recurrence
1. Very high in stage III/IV pressure sores
2. Proper patient selection and proper post-operative management reduce this risk
X. OUTCOMES
A. Recurrence: Range from 5% to 90% in large series
PEARLS
1. Many healed or surgically closed pressure ulcers recur. Recurrence usually occurs within one year.
2. Recurrence of pressure sores is mostly due to inadequate debridement and patient non-adherence to pressure-relief protocols.
3. Outpatient support, patient motivation, and modification of risk factors also significantly influence success in maintaining a closed wound
4. Operative closure is not appropriate for every patient. Surgical candidates need both social and clinical factors optimized for sustained wound closure.
5. Important considerations when making clinical decisions
a. Is there devitalized tissue?
b. Is the amount of devitalized tissue more than could likely be debrided with dressing changes alone?
c. Has the patient had recent improvement in the wound with current dressing regimen?
d. Is the patient stable for the operating room? Has anticoagulation been held?
e. Have all social issues been optimized?
QUESTIONS YOU WILL BE ASKED
1. What are the three stages of wound healing?
Inflammatory, proliferative, and remodeling.
2. Besides pressure and noncompliance, what else should you consider in the differential diagnosis for nonhealing wounds?
Residual infection of soft tissue, untreated OM, and Marjolin’s ulcer.
3. What are several flap options for ischial ulcer closure?
Gluteus rotation advancement flap, V–Y hamstring flap, and inferior gluteal artery-based fasciocutaneous flap from posterior thigh.
4. Which flap is ideal for ischial pressure ulcer in an ambulatory patient and what is the blood supply?
Posterior thigh flap and descending branch of inferior gluteal artery.
5. What is gold standard to diagnose OM?
Bone biopsy.
Recommended Readings
Brown DL, Kasten SJ, Smith DJ Jr. Surgical Management of Pressure Sores. In: Krasner DL, Rodeheaver GT, Sibbald RG (eds): Chronic Wound Care: A Clinical Source Book for Healthcare Professionals, Fourth Edition, HMP Communications; 653–660, 2007.
Levi B, Rees R. Diagnosis and management of pressure ulcers. Clin Plast Surg. 2007;34(4):735–448. PMID: 17967627.
Tchanque-Fossuo CN, Kuzon WM Jr. An evidence-based approach to pressure sores. Plast Reconstr Surg. 2011;127(2):932–939. PMID: 21285799.
< div class='tao-gold-member'>