1 Plastic surgery and innovation in medicine
Synopsis
 There is a major difference between research and innovation, though the two are often interrelated.
There is a major difference between research and innovation, though the two are often interrelated.
 Most advances in surgery come from innovation rather than basic research.
Most advances in surgery come from innovation rather than basic research.
 Surgical innovation is one of the defining features of plastic surgery.
Surgical innovation is one of the defining features of plastic surgery.
 Surgical innovation is made safe by defining principles.
Surgical innovation is made safe by defining principles.
 A detailed knowledge of anatomy is a major factor on which these principles are based.
A detailed knowledge of anatomy is a major factor on which these principles are based.
 A balance between out-of-the-box thinking and conservative deliberation is the perfect milieu to effect change yet keep perspective.
A balance between out-of-the-box thinking and conservative deliberation is the perfect milieu to effect change yet keep perspective.
Introduction
We often tell our students that the great thing about plastic surgery is that we are the last real general surgeons. We are not confined to a body area or linked to a disease, unlike almost every other medical specialty. Similarly, while there are some operations that are reasonably standardized, plastic surgery is the one specialty in which this is more the exception than the rule. We often perform operations that we’ve never exactly done before and will likely never do in precisely the same way again. We almost always have completed elements of the surgery before, or we may add elements from another sphere of surgery to create a new approach to a problem. Sometimes this is born of necessity, the challenge of solving a unique problem for which there is no standard or well-accepted solution. Sometimes it is born of the will to do something better, to solve a problem in such a way that is better than the accepted means of dealing with it. When I tell nonmedical people this they are usually shocked and somewhat appalled. To the uninitiated it may seem cavalier, even dangerous. However these innovations are based on principles that we learn in our training and that we come to apply in our practice. That is the magic of plastic surgery. Of course this type of surgical innovation raises ethical issues and it is something with which many institutions are struggling, not merely in the domain of plastic surgery but in the field of surgery in general. Many institutions already have processes and protocols in place to oversee and regulate innovation.1 When is innovation in surgery ethical and when is it not? This has already been the source of much discussion in the literature.2–4 How far can we safely push the envelope? That particular discussion is beyond the scope of this chapter. Suffice it to say that it is important to strike a balance between necessary oversight of research practices and a supportive environment where research can flourish.
Innovation and research
What is the difference between innovation and research? Wikipedia (http://en.wikipedia.org/wiki/Research) defines research as follows: “Research can be defined as the search for knowledge or any systematic investigation to establish facts.” Here (http://en.wikipedia.org/wiki/Innovation) is the definition for innovation: “Innovation is a change in the thought process for doing something or ‘new stuff that is made useful’.”5 It may refer to an incremental emergent or radical and revolutionary change in thinking, products, processes, or organizations. Innovation can come from research but does not necessarily need to. This is true in other fields. For example, innovations in the computer industry are often simple changes introduced to facilitate a task, only to sometimes completely change how things are done. Most of the surgical innovations we see are not the result of research. In fact, not infrequently, an innovation is subsequently subjected to more rigorous study. A surgeon may design a new operation or, for example, a new flap. This may be a variation on an old procedure or sometimes something completely new. As already mentioned, it may have been forced on the surgeon because of the circumstances of the case. There may be no other way to solve the problem. When it works the surgeon decides to design a study to explain why the procedure worked or to describe the blood supply of the flap. Though one could argue that this is not the ideal way to do things, it certainly happens6,7 and is merely a reflection of the dynamic nature of surgical innovation. Innovation may be planned or, in the case of this example and as happens probably more frequently, be made on the fly. Research may be innovative. A researcher may design a novel experiment to probe a theory, an approach to the problem that has not been explored before. This is also innovation and is more commonly how research and innovation are linked. An innovative idea is subjected to the scientific method that research demands. What makes an innovator? It has been said that the characteristics than most major innovators have in common include: (1) the ability to recognize an idea; (2) persistence in developing the strategy; and (3) commitment to the project, and final completion of a response to the problem or problems in question.8
Composite tissue allotransplantation
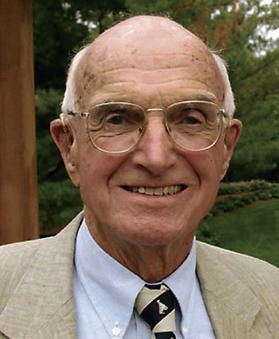
In research we work with models – models of disease, models of a procedure. Animal models provide a means by which we can study the process that we are interested in addressing in our patients. Occasionally, in order to solve a problem, we move to models that are perhaps less relevant to our everyday clinical practice. For example, most people don’t realize that the first kidney transplant was performed by Dr. Joseph Murray, a plastic surgeon at the Peter Bent Brigham Hospital in Boston9 (Fig. 1.1). People are generally intrigued by this snippet of information. What was a plastic surgeon doing transplanting kidneys? How could this be? His practice as a plastic surgeon raised questions in his mind surrounding transplantation. His experience treating burn patients sent back from the war during World War II gave him wide exposure to skin grafting and raised issues of immune rejection that he would later find ways to address. In trying to work out the immunology of skin grafts he moved to a single-organ model, the kidney, in order to answer the question he had originally conceived. This culminated in the first successful kidney transplant performed from one twin to another by Dr. Murray at the Peter Bent Brigham Hospital in Boston in 1954. Having helped develop the specialty of transplantation, he went on to perform the world’s first successful allograft in 1959 and the world’s first cadaveric renal transplant in 1962. Dr. Murray ultimately returned to his roots, the practice of plastic surgery, and was awarded the Nobel Prize in Physiology or Medicine in 1990 for his contribution to the science of transplantation.
Now that wheel has turned full circle and plastic surgery is, once again, in the mainstream of transplant innovation (Ch. 34). Hand and face transplants have become a reality and, though still not in the mainstream of practice, it is likely that composite tissue allotransplantation (CTA) will become more common in the foreseeable future. In fact, even now, some would argue that hand transplantation is the standard of care (see Volume 6, Ch. 38). Face transplantation is sure to follow (see Volume 3, Ch. 20). Furthermore, it is likely that CTA will address those reconstructions that we cannot realistically achieve with conventional reconstructive techniques. This would include transplantation of functioning eyelids, noses, ears, tongue, and other specialized organs. While total nasal reconstruction, as an example, has attained a high level of sophistication, the truth is that elegant nasal reconstructions are achieved by only a small number of expert surgeons utilizing very complex techniques in a series of operations over a period of months or years. The concept of a surgeon being able to transplant a nose in a single stage and achieve an elegant result is very attractive. Obviously many obstacles remain before we will see this in practice. CTA is a perfect example of how an innovative technical advance engenders increased research activity. The barrier to successful transplantation is not a technical one, it is an immunologic one and current interest in CTA has spawned a new wave of research activity in the field of immunology. This demands a collaborative and multidisciplinary approach, something that, again, plastic surgeons do well.
Collaboration
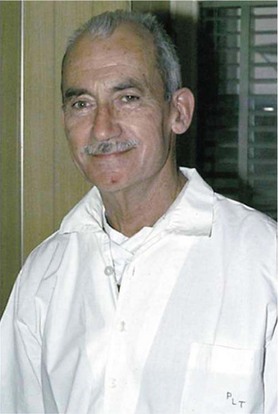
Plastic surgeons cannot lay claim to being the only innovators in medicine. Medicine is full of innovators. Yet it is true that the nature of the plastic surgeon’s work, more than many other specialties, demands innovation. And that is what most plastic surgeons do every day of the week. Because so much of what we do, particularly in reconstructive surgery, is in collaboration with other specialties, innovation in those areas of practice often lead to innovations in our field. Most of the innovations we see are incremental. A surgeon incrementally changes how (s)he practices or how (s)he does a particular operation. Every now and again the innovation is radical. The development of craniofacial surgery is an example of radical innovation. Paul Tessier (Fig. 1.2) was the first to describe a combined intra- and extracranial approach for the correction of hypertelorism,10,11 breaking the previously held taboo of exposing the intracranial environment to the upper aerodigestive tract. Going against the surgical mainstream demands unimaginable courage. It takes pioneers like Dr. Tessier to have the courage of their convictions and push the envelope beyond the general comfort level. Apart from spawning the specialty of craniofacial surgery, Dr. Tessier’s advances led to advances in related fields. One such example is that of skull base surgery. The craniofacial principles developed by Dr. Tessier literally opened up the field of skull base surgery. Tumors that were previously considered inoperable and inaccessible became treatable. That progress led to further innovations. So, continuing with the example of skull base surgery, the radical resections and approaches that were developed in the 1970s and 1980s12,13 created problems such as meningitis and brain abscesses and problems related to delayed wound healing. Smaller defects could be closed with local flaps such as pericranial flaps, or galeafrontalis flaps.14 However larger defects remained a problem until free flaps were used to close these defects.15,16 Then the incidence of all of the complications, the brain abscesses, meningitis, and wound-healing problems, were all dramatically reduced and the surgery became safer. So microvascular surgery made skull base tumor surgery safer.
More recently, in this field we have seen innovations in the surgical approaches to the skull base facilitate the development of endoscopic skull base surgery. Large resections are now feasible through an endoscopic approach. This development has had a large impact on these patients because extensive open approaches with the associated risks of scarring and deformity are no longer necessary. However, with these large endoscopic resections, we are seeing the re-emergence of problems such as meningitis and abscess because of the difficulty in reconstructing these defects endoscopically.17 This has led to the development of new reconstructive techniques and approaches in order to address these complications.18–20
Drivers of innovation
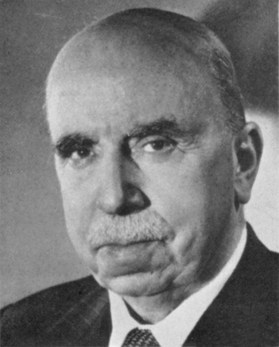
Innovation is also forced in times of upheaval and change. The classic examples are war and natural disasters. More surgical advances are made in wartime than in peacetime. This is because specific problems are seen in unprecedented numbers and demand a solution. In this sort of environment it becomes reasonable to break the rules. One simply has to cope. Out of this generally comes a change in practice. Most of the advances in how we manage major trauma have come from the arena of war. The MASH units of the Korean conflict taught us that initiating treatment early, in the field, saves lives. The ultimate progression of that concept has been the development of robotic surgery, bringing high-level expertise to the field so that skilled intervention can be effected at the earliest possible opportunity. The fact that this can be achieved using robotic technology makes it feasible for a highly skilled surgeon located in some central site to treat multiple injuries in separate locations. The types of injury seen in war also lead to changes in practice. Plastic surgery, as we know it today, was born during the first world war. Sir Harold Gillies (Fig. 1.3) developed techniques for facial reconstruction initially at Aldershot and later at the Queen’s Hospital in Sidcup, Kent, UK. (It later became Queen Mary’s Hospital.) His innovative solutions for some of the injuries he saw led to the development of modern plastic surgery.
During the Second World War the Plastic Surgery Unit at the Queen Victoria Hospital in East Grinstead, UK, headed by Sir Archibald McIndoe (Gillies’ cousin) (Fig. 1.4)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree