2 Nonsurgical skin care and rejuvenation
Determining skin type
Fitzpatrick skin phototype
Dr. Thomas B Fitzpatrick first introduced his approach to categorizing skin type, now known as the Fitzpatrick skin phototype (SPT) system, in 1975 in order to evaluate a patient’s response to ultraviolet (UV) exposure in preparation for treating psoriasis with light.1 In this system, patients are assigned a skin type based on their reported ability to tan or burn. A minimum erythema dose (MED) is identified for each skin type, which the practitioner then uses as a guide for selecting doses of UV therapy for various skin conditions. Of note, this skin-typing system has evolved into a method for characterizing a patient’s skin color. Currently, dermatologists may assign an SPT to a patient based on a clinical assessment of skin color and not necessarily after questions regarding the patient’s history of sun tanning or burning (Table 2.1). The Fitzpatrick SPT system originally included skin types I–IV and categorized only white skin. Naturally dark pigmented skin is typically labeled as SPT IV–VI. When category V was first added, it was used to describe all skin of color (brown or dark-brown skin). The SPT VI designation was later added to classify further skin of color.2 The correct use of the Fitzpatrick SPT is not an indicator of a patient’s ethnicity or interpretation of an individual’s skin color and complexion, but a measure of the skin’s potential to burn or to tan.
Table 2.1 The Fitzpatrick skin phototypes
| Skin type | Typical features/appearance | Reaction to sun exposure/tanning tendency |
|---|---|---|
| Type I | Very fair/pale skin; blond or red hair; light-colored eyes; freckles common | Always burns, never tans |
| Type II | Fair-skinned; light eyes; light hair | Burns easily, occasionally tans |
| Type III | Medium/darker white/fair skin; eye and hair color vary | Sometimes burns, gradually tans |
| Type IV | Mediterranean Caucasian skin (olive to light brown); medium to heavily pigmented | Burns minimally, tans easily |
| Type V | Middle Eastern skin; rarely sun-sensitive | Rarely burns, tans always |
| Type VI | Dark brown/black skin, rarely sun-sensitive | Never burns, always tans darkly |
Although the Fitzpatrick SPT is widely accepted and used in dermatology, the system does not fully address certain issues related to individuals with darker skin types. For instance, some authors have questioned the potential to predict a patient’s MED based on reported ability to tan and burn. In fact, a poor correlation was observed between SPT, as obtained by self-reported tanning history, and MED in a study involving white patients. This study did reveal a better correlation between MED and skin complexion traits such as eye and hair color, freckling tendency, and number of moles.3 A poor correlation between SPT, based on self-reported tanning history, and MED has also been found in various studies in Asian and Arab skin.4–7 The authors of these studies have suggested that the SPT system is not applicable to nonwhite patients or the full range of ethnic backgrounds.
Another issue with the SPT system pertains to the correlation of visually assessed skin color with MED. Many dermatologists assign a Fitzpatrick SPT to a patient based on a clinical assessment of skin color, and rarely question a patient on skin-tanning history. Further, some authors have contended that SPT (as determined by observed skin color) does not correlate with the MED in ethnic skin. Specifically, they have suggested that, in skin of color, the constitutive pigment does not correlate with MED, as implied by the current conventional application of SPT.8
For example, patients of African descent are typically labeled as having Fitzpatrick SPT V (brown) or VI (dark brown). However, it has been discovered through questioning that some of these patients have reported that they do frequently burn. If categorized based on self-reported tanning history, a subset of such patients likely would be classified as having SPT III or IV. In a study that compared skin pigmentation as measured by diffuse reflectance spectroscopy of MEDs, investigators found that epidermal pigmentation was not an accurate predictor of skin sensitivity to UVB radiation.9 These data illustrate some of the limitations of the SPT, which was originally designed to assess lighter skin types. Although the Fitzpatrick SPT remains in wide use, several other systems have been created in an attempt to depict skin type more accurately.
Baumann skin-typing system
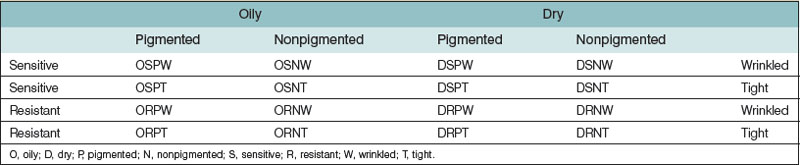
The author has developed the Baumann skin-typing system (BSTS) in order to recognize a wider range of cutaneous variables. Four skin parameters are assessed: (1) oily versus dry; (2) sensitive versus resistant; (3) pigmented versus nonpigmented; and (4) wrinkled versus tight (unwrinkled). These four spectra are not mutually exclusive; therefore, assessing the skin using all four parameters yields 16 potential skin-type permutations (Table 2.2).
The BSTS provides specific guidance to identify the most suitable skin products for individuals, and also to help standardize the discussion of skin care science. The BST is easily determined by a scientifically validated questionnaire known as the Baumann skin type indicator (BSTI), which is used to identify baseline skin type10 (questionnaire available at no charge at www.skintypesolutions.com). Doctors and aestheticians can use this information to help identify the products and procedures most suitable for their patients. The remainder of this chapter will discuss skin care science following the format of the BSTS.
Skin aging
The manifestation of cutaneous aging is a result of the complex interplay between intrinsic and extrinsic factors. Intrinsic aging is attributed to individual heredity and the natural effects of the passage of time and, as such, is considered inevitable and beyond voluntary control. Extrinsic aging occurs as the result of exogenous insults, such as exposure to UV radiation, cigarette smoke, other pollution, as well as poor nutrition, and, by definition, can be avoided. Premature skin aging is evidence of extrinsic aging. In fact, 80% of facial aging is attributed to solar exposure alone.11
At a cellular level, UV exposure leads to skin damage through numerous mechanisms, including sunburn cell formation, thymine dimer development, collagenase production, and engendering an inflammatory response. These lead to photoaging, photocarcinogenesis, and photoimmunosuppression.12 Interestingly, a recent paper suggests that the photoaging and melanogenesis provoked by UV exposure are linked to telomere-based DNA damage signaling that may represent a cancer avoidance protective response.13 Telomeres, specialized chromosomal components, shorten with age; telomeric loss or erosion has thus become an important measure of cellular aging, a veritable internal aging clock.14 The enzyme telomerase, which stabilizes or lengthens telomeres, is expressed in about 90% of all tumors but absent in many somatic tissues.15 One of the few regenerative tissues to express telomerase, however, is the epidermis.16 Telomerase is believed to act against excessive telomere loss in human epidermis throughout the lifelong regeneration process.17 Interestingly, exposure to UV radiation, due to its deleterious effect on DNA and its acceleration of telomere shortening, can be characterized as influential in intrinsic as well as extrinsic aging. Signaling through p53 after telomere disruption is also typically observed in skin aging and photodamage.18 Currently, there are no skin care products available that target telomerase.
At the macroscopic level, the development of rhytides, caused by alterations in the dermal layer of skin, is the most prominent manifestation of cutaneous aging. Because few skin care product ingredients can sufficiently penetrate the dermis to ameliorate deep wrinkles, the prevention of rhytides is the focus of dermatologic antiaging skin care.19 Specifically, dermatologists aim to slow the degradation of or replenish the three main dermal constituents (collagen, elastin, and hyaluronic acid), all of which are known to decline with age. Reducing inflammation is key here, as inflammation can contribute to the breakdown of these structural components of the skin. Skin inflammation itself can result from the formation of free radicals, which can act directly on growth factor and cytokine receptors in keratinocytes and dermal cells.
While the exact mechanisms of growth factors and cytokines in skin aging have not been fully understood, it has been established that they function together in a complex interplay involving several types of growth factors and cytokines.20 Better understood, however, is the influence of free radicals on the aging process. The activation of the mitogen-activated protein kinase pathways induced by free radicals has been shown to result in collagenase synthesis, paving the way for collagen degradation.21 Using antioxidants to inhibit this pathway is believed to prevent photoaging by thwarting collagenase production. In a study on human skin, Kang et al. demonstrated that pretreatment with the antioxidants genistein and N-acetyl cysteine hindered the UV induction of the cJun-driven enzyme collagenase.22 Vitamins C and E, ferulic acid, coenzyme Q10, green tea, pycnogenol, silymarin, and idebenone are among the various antioxidants featured in multiple skin care products.
Dry skin
The relative lack of moisture in the SC is indicative of xerosis, or dry skin, which is characterized by cracks and fissures when the level of water, the primary plasticizer of the skin, is low.23 Water content in the SC must be at least 10% in order for the skin to appear and feel normal.24 The elevation in transepidermal water loss (TEWL) that progresses to xerosis occurs when a defect in the permeability barrier permits the loss of excess water to the atmosphere. The etiology of the barrier perturbation itself is generally multifactorial and includes variables such as harsh detergents, acetone, and other contactants, as well as frequent bathing (Box 2.1).
Underlying disease is not the root cause of the majority of dry-skin complaints. Most patients simply lack the ability to cope with environmental elements that adversely affect the water-binding capacity of the SC (see Box 2.1 for environmental factors that can cause dry skin). Dry skin is more likely to occur during the fall and winter months due to lower humidity as well as excessive bathing in hot water. The condition also increases with age, as skin tends to become less oily. Indeed, xerosis has been referred to as “winter itch” because it is at its worst during that season. The areas of the body most often affected are those with comparatively few sebaceous glands, such as the arms, legs, and torso.
Clinical signs
Initial clinical signs of xerosis include a dull gray-white color and increased topographical skin markings.25 With increased dryness, TEWL spurs a degradation in the cohesiveness between the corneocytes, while resulting in an abnormal retention of desmosomes. The loss of cohesiveness in entire sheets of corneocytes manifests in scaling, flaking, and an overall rough cutaneous texture. The resultant appearance of the skin is dull because a rough surface is less able to refract light than a smooth surface. The skin is then less pliable with stretching and bending; diminished elasticity can then yield visible cracks and fissures.
Basic skin care formulations
Cleansers
Bar surfactants
Soap (alkyl carboxylate), the primary surfactant in most cleansing bars, is usually produced by saponification, involving a reaction of a triglyceride oil/fat with an alkali. Vegetable oils (e.g., palm oil, palm oil derivatives, rice bran oil, ground nut oil, and castor oil combined with coconut oil or palm kernel oil) are typical.26 Nonvegetable ingredients in soap typically come from animal fat (e.g., tallow). Despite their effectiveness as cleansers, soaps can irritate the skin, causing erythema, xerosis, and pruritus, especially in cold weather.27 Newer classes of soaps (i.e., superfatted soaps, transparent soaps, and combination bars) have been developed to provoke less irritancy.
Superfatted soaps
Superfatting is intended to enhance the mildness, moisturization, lather, mush value, and wear rate of a soap.28–30 This is achieved through incomplete saponification (neutralization) by leaving unreacted fatty acids or oils in the soap or by adding fatty alcohols, fatty acids, or esters during production.
Transparent soaps
Manufacturing with a high level of humectants intended to solubilize the soap renders a transparent, clear appearance. Transparent soaps contain high levels of active soap and an alkaline pH, qualities that typically cause irritancy. These products are usually mild, however, due to the presence of the humectant glycerin and low levels of fatty acids.31
Combination bars
Combination bars (combars) combine natural soaps with milder synthetic surfactants. The pH of these products is in the high range (9.0–9.5), but the synthetic surfactants seem to inhibit irritancy, leaving these products less likely to cause irritation as compared to average soaps.32
Synthetic detergent bars
Unlike soaps, synthetic detergent bars (syndet bars) are created through esterification, ethoxylation, and sulfonation of oils, fats, or petroleum products, and are formulated in the neutral-pH range. Alkyl glyceryl ether sulfonate, alpha olefin sulfonates, betaines, sulfosuccinates, sodium cocoyl monoglyceride sulfate, and sodium cocoyl isethionate are among the synthetic surfactants used in such bars.33 The most commonly used synthetic surfactant is sodium cocoyl isethionate, which confers mildness on these products.
Liquid surfactants
Anionic and amphoteric surfactants are often combined in liquid cleansers. Soaps (salts of fatty acids) and synthetic surfactants such as alkyl ether sulfate, alkyl acyl isethionates, alkyl phosphates, alkyl sulfosuccinates, and alkyl sulfonates are the anionic surfactants regularly used in these products. The common amphoteric or zwitterionic surfactants used are cocoamido propyl betaine and cocoamphoacetate. Nonionic surfactants (e.g., alkyl polyglucoside) and amino acid-based surfactants (e.g., acyl glycinates, alkyl glutamates, and sarcosinates) are increasingly used as the main surfactants in liquid cleansers because they enhance mildness. Most liquid cleansers have a pH in the neutral to acidic range; however, the products that contain soap (alkyl carboxylate) as the chief active ingredient usually have an alkaline pH (Box 2.2).
Box 2.2
• For patients with dry skin, suggest a nonfoaming cleanser such as a cleansing milk, oil, or cream.
• Surfactants in foaming cleansers strip necessary lipids from the skin, leaving the skin with an inability to hold on to water.
• Unpublished marketing studies show that most patients prefer the stripping foaming cleansers because they “feel cleaner,” so it is crucial to educate patients with dry skin to avoid these.
Moisturizers
Moisturizers increase water content in the SC by preventing water evaporation (TEWL) from the skin with the use of occlusive ingredients or by increasing the integrity of the skin barrier. The primary method of increasing the integrity of the skin barrier is delivering fatty acids, ceramides, and cholesterol to the skin and controlling the calcium gradient. Assisting the skin to hold on to water is another moisturization approach, achieved by increasing levels of NMF, glycerol (glycerin), and other humectants such as hyaluronic acid. Enhancing the ability of the epidermis to absorb important components for the circulation, such as glycerol and water through aquaporin channels, also augments skin hydration (Box 2.3).
Box 2.3
• The best moisturizers contain both humectants and occlusives.
• One of the best humectant ingredients is glycerin because of its ability to transverse aquaporin channels and absorb into the dermis.
• Oils that contain antioxidants and/or linoleic acid are the best occlusives.
• Examples include safflower oil, sunflower oil, olive oil, walnut oil, peanut oil, and grape seed oil.
Occlusives
Typically oily substances that can dissolve fats, and therefore widely used in skin care cosmetics, occlusives coat the SC to inhibit TEWL and provide an emollient effect. Two of the best occlusive ingredients are petrolatum and mineral oil. Petrolatum, a purified mixture of hydrocarbons derived from petroleum (crude oil) and used as a skin care product since 1872, exhibits a water vapor loss resistance 170 times that of olive oil.34 The hydrocarbon molecules present in petrolatum prevent oxidation, yielding a long shelf-life for this occlusive, considered the gold standard to which other ingredients are compared.35 However, although also known for being noncomedogenic, petrolatum has a greasy feeling that may render it cosmetically unacceptable to patients.36 Mineral oil, or liquid petrolatum, is derived from the distillation of petroleum in the production of gasoline; cosmetic-grade mineral oil has been available for over 100 years and is one of the most frequently used oils in skin care products.37 In 2004, a randomized double-blind controlled trial of 34 patients with mild-to-moderate xerosis demonstrated that mineral oil and extra-virgin coconut oil were equally efficacious and safe as moisturizers, with surface lipid levels and skin hydration significantly improved in both groups.38 However, an earlier epidemiologic review of the relationship between mineral oil exposure and cancer that revealed several associations has spawned some myths about this agent.39 The cases of cancer that occurred resulted from prolonged exposure to industrial-grade mineral oil. Cosmetic-grade mineral oil has never been linked to cancer. Also, unlike the industrial grade, cosmetic-grade mineral oil is noncomedogenic. Significantly, occlusive agents are effective only while present on the skin; TEWL returns to the previous level once occlusives are removed.
Occlusives are typically combined with humectant ingredients in moisturizers. Other commonly used occlusive ingredients include lanolin, paraffin, squalene, dimethicone, propylene glycol, beeswax, soybean oil, grapeseed oil,40 and other “natural” oils that have become increasingly popular, such as sunflower seed, evening primrose, olive oil, and jojoba oils.41–45
Lanolin
Derived from the sebaceous secretions of sheep, lanolin is a complex natural product that cannot be synthesized; its composition is very different than human sebum.46 Nevertheless, like SC lipids, lanolin contains cholesterol, an essential component of SC lipids, and, significantly, both lanolin and SC lipids can coexist as solids and liquids at physiologic temperatures. The concern over allergic reactions to lanolin has led to the development of ultrapure medical-grade lanolin products, which have been demonstrated as effective in treating dry skin and healing superficial wounds.47–49
Humectants
Humectants are water-soluble materials with high water absorption capabilities. In low-humidity conditions, however, humectants can attract water from the deeper epidermis and dermis, thereby exacerbating xerosis.50 Therefore, humectants are effective as intended when combined with occlusive ingredients. In cosmetic moisturizers, humectant ingredients prevent product evaporation and thickening, thereby prolonging product shelf-life. Humectants can also alter the appearance of the skin; that is, by drawing water into the skin, a slight swelling of the SC results, rendering the perception of smoother skin with fewer wrinkles. Consequently, several moisturizers are marketed as “antiwrinkle creams” even though they confer no long-term antiwrinkling benefit. Commonly used humectants include glycerin, urea, sorbitol, sodium hyaluronate, propylene glycol, alpha hydroxy acids (AHAs), and sugars. Urea, which has been included in hand creams since the 1940s,51 is a component of the NMF and also exhibits a mild antipruritic effect.52 It is important to note that hyaluronic acid, a humectant, does not penetrate into the dermis when applied topically.
Glycerin
A potent humectant, glycerin (glycerol) displays a hygroscopic ability comparable to that of NMF,53 which allows the SC to retain a high water content even in a dry environment. Glycerol levels have been shown to correlate with SC hydration levels, suggesting a significant role in skin hydration for this humectant.54 In a 5-year study comparing two high-glycerin moisturizers with 16 other popular moisturizers in 394 patients with severely dry skin, the high-glycerin products were found to be superior because they rapidly restored normal hydration to dry skin and helped to prevent the return to dryness for a longer period than other products, even those containing petrolatum.55 Glycerin induces an expansion of the SC due to increased thickness of the corneocytes and creates expanded spaces between layers of corneocytes.56 Therefore, it appears that glycerin generates a reservoir of moisture-holding ability that leaves the skin more resistant to drying. It is worth noting that, while glycerol can be obtained from topical preparations, it can also be transported from the circulation into the epidermis through aquaporin channels. Normal SC hydration requires endogenous glycerol according to recent studies.57 The potential importance of endogenous glycerol for normal SC hydration has been shown by two different studies by Hara et al. Knockout mice, which lack the aquaporin-3 (AQP-3) water channel, cannot transport glycerol from the circulation into the epidermis and they exhibit abnormal SC hydration and decreased SC glycerol levels.58 The topical application of glycerol remedies this defect in mice.59
Emollients
By filling the spaces between desquamating corneocytes and providing increased cohesion, resulting in a flattening of the curled edges of the individual corneocytes, emollients yield a smooth surface, and are added to cosmetics to soften and smooth the skin.32,60 Many emollients act as humectants and occlusive moisturizers as well. Lanolin, mineral oil, and petrolatum are occlusive ingredients that also impart an emollient effect. Several natural ingredients also confer such benefits.
Oatmeal
Wild oats (Avena sativa) have been used for over 2000 years in traditional folk medicine, especially as a poultice or soak. For decades in the West, colloidal oat grain suspensions have been used as adjuvant therapy for atopic dermatitis.61 Colloidal oatmeal has replaced rolled oats and oatmeal in skin care products, and has exhibited moisturizing and anti-inflammatory properties.60 Further, oatmeal is one of the few botanically derived products labeled by the Food and Drug Administration (FDA) as an effective skin protectant.
Shea butter
Used widely in cosmetic formulations as a moisturizer, particularly as an emollient, shea butter (Butyrospermum parkii) is a natural fat derived from the African shea or karite tree that has been shown to manifest anti-inflammatory activity.62 Shea butter is found in various skin and hair care products, especially high-end skin products, and is touted for delivering rich emollient benefits. It is also believed to confer benefits as an adjuvant moisturizer in the treatment of atopic dermatitis, dry skin, acne, scars, and striae alba.
Other ingredients
Vitamins C and E, coffeeberry, green tea, and coenzyme Q10 are among the antioxidant ingredients often found in moisturizers. These are popular ingredients because antioxidants are believed to neutralize the free radicals that assault the skin and other organs and thereby contribute to cutaneous aging. Niacinamide and soy, which are key depigmenting agents, are also popular additives in cosmetic moisturizers. Glycyl-l-histidyl-l-lysine-Cu2+ (GHK-Cu), a copper tripeptide complex, is also found in many moisturizers. GHK-Cu complex has been used for many years to enhance wound healing and it has also been demonstrated to augment collagen synthesis.63,64
Hydroxy acids
Alpha hydroxy acids
AHAs, a group of water-soluble, naturally occurring compounds so named because they contain a hydroxy group in the alpha position, function as humectants as well as exfoliants. This versatile family includes glycolic acid (derived from sugar cane), lactic acid (from sour milk), citric acid (from citrus fruits), malic acid (from apples), tartaric acid (from grapes), and phytic acid (from rice).65 Glycolic acid and lactic acids are the most commonly used AHAs, were the first to reach the market, and will be the only ones discussed here. Topical preparations containing AHAs have long been known to influence epidermal keratinization,66 and the use of hydroxy acids in skin care dates back to ancient Egypt and Cleopatra, who was believed to have applied sour milk to her face to foster youthfulness.
The cosmetic effects of hydroxy acids include normalization of SC exfoliation, leading to enhanced plasticization and fewer dry scales on the skin surface. AHAs and beta hydroxy acid (BHA) degrade the desmosomes and allow desquamation to proceed. They also affect corneocyte cohesion at the basement levels of the SC,67 where they alter pH and promote desquamation. Applying AHAs and BHA in high concentrations results in the detachment of keratinocytes and epidermolysis. Application of AHAs and BHA at lower concentrations degrades intercorneocyte cohesion directly above the granular layer, which accelerates desquamation and SC thinning. A thinner SC is more flexible and compact, and better reflects light, giving the skin a more luminous and youthful appearance.68 However, a thinner SC can confer some disadvantages, as exfoliants have been shown to reduce the MED of the skin.69 Although one study indicated that glycolic acid delivered a photoprotective effect,70 subsequent studies have suggested that increased photosensitivity is associated with the application of AHAs.71,72 The FDA now requires that AHA products include a label warning that sun protection should accompany their use.
Lactic acid
Lactic acid, first used in 1943 for the treatment of ichthyosis,73 is a popular AHA found in several at-home products as well as prescription moisturizers, and is usually not used as an in-office peel. It is unique insofar as it is an AHA as well as a component of the NMF, which plays an important role in hydration. Studies of the activity of buffered 12% ammonium lactate lotion (LacHydrin) have documented the moisturizing ability of lactic acid.74 One study using 5% and 12% lactic acid resulted in increases in skin firmness and thickness and enhanced texture and hydration in the epidermis, but not dermis.75 Lactic acid (particularly the l-isomer) has been shown in vitro and in vivo to augment ceramide synthesis by keratinocytes.76 In fact, application of the l-isomer of lactic acid to keratinocytes also increased the ratio of ceramide-1-linoleate to ceramide-1-oleate, which is significant because a lower ceramide-1-linoleate to ceramide-1-oleate ratio is seen in atopic dermatitis and acne.77,78 In addition, lactic acid imparts antiaging benefits, as implied by a double-blind vehicle-controlled study finding that an 8% l-lactic acid formula performed better than vehicle in treating photoaged skin, with statistically significant improvements in skin roughness, mottled hyperpigmentation, and sallowness.79
Glycolic acid
Popularly known as “the lunchtime peel” because it can be completed quickly, effectively, and discreetly within a lunch hour without obvious visible signs, glycolic acid is the AHA most commonly used in chemical peels in the offices of dermatologists and aestheticians. In 1996, Ditre et al. demonstrated that applying AHAs led to a 25% increase in skin thickness, increased acid mucopolysaccharides in the dermis, improved the quality of the elastic fibers, and increased collagen density, as determined histologically.80 Such findings imply that AHAs reverse some of the histological signs of aging. Such data were buttressed by Moon et al., who reported that mice treated with glycolic acid exhibited a significant reduction in wrinkle score and an increase in collagen production, which typically decreases with age.81 Increased collagen production after treatment with AHAs has been demonstrated in vivo and in vitro using fibroblast cultures. Glycolic acid treatments increased collagen synthesis as well as fibroblast proliferation in vitro in one study.82 To prevent burning, glycolic acid, unlike many other peels, must be neutralized after use. Therefore, glycolic acid should not be used on large areas of the body, but, rather, in small areas on which application can be quickly applied and neutralized.
Beta hydroxy acid
The only BHA, salicylic acid, is a chemical exfoliant derived from willow bark, wintergreen leaves, and sweet birch, though it is also available in synthetic form.83 Although labeled a BHA because the aromatic carboxylic acid has a hydroxy group in the beta position, the carbons of aromatic compounds are traditionally given Arabic numerals (1, 2, etc.) rather than the Greek letter designations typical for the nonaromatic structures. Salicylic acid was likely labeled a BHA at the time the peels were introduced for marketing purposes and to benefit from the popularity of AHAs. Although BHA is a newer category of chemical peels, salicylic acid has a long and versatile history of effectiveness in skin care. As a chemical peel, salicylic acid is available in over-the-counter home products (usually in 0.5–2% concentrations and often labeled as “acne washes,” and suitable for treating acne, rosacea, photoaging, and hyperpigmentation) and in those used in the office (usually 20–30% concentration). It is also a component in various in-office peels using a combination of ingredients, such as the Jessner’s Peel, the PCA peel by Physician’s Choice, and the Pigment Plus Peel by Biomedic.
Most cosmetic dermatologists use preparations of 20% or 30% salicylic acid for in-office peels, which have been demonstrated to fade pigment spots, decrease surface roughness, and reduce fine lines,84 comparable to AHA peels. In the early 1990s, satisfactory results were seen using 50% salicylic acid on the hands and forearms of patients with actinically induced pigmentary alterations.85 These effects are likely a result of enhanced exfoliation and an accelerated cell cycle, as observed with AHAs. Unlike AHAs, however, BHA influences the arachidonic acid cascade and, consequently, displays anti-inflammatory activity, which may allow salicylic acid peels to be effective while causing less irritation than AHA peels. The anti-inflammatory properties of salicylic acid render it very useful in a peel for patients with acne and rosacea. BHC can also be combined with other acne treatments to accelerate the resolution of comedones and papules. In addition, salicylic acid is lipophilic, which enables it to impart a stronger comedolytic effect than AHA peels as well as penetrate the sebaceous material in the hair follicle and exfoliate the pores.
Of note, salicylic acid peels can exert a whitening effect in patients with darker skin types. A study of 24 Asian women treated with biweekly facial peeling with 30% salicylic acid in absolute ethanol for 3 months exhibited some pigmentary lightening.86 Postinflammatory hyperpigmentation can also result from BHA peels. Unlike AHAs, BHA does not need to be neutralized and the frost is visible once the peel is complete.
Sensitive skin
Sensitive skin has been historically difficult to fully characterize. Yokota et al. as well as Pons-Guiraud offered their input on this convoluted issue by offering classification systems within the past decade; however, few agree on a typing system for sensitive skin.87,88 Within the BSTS framework, sensitive skin is classified into four types based on clinical manifestations: type 1 (developing open and closed comedones and pimples; known as the acne type or S1 type), type 2 (facial flushing due to heat, spicy food, emotion or vasodilation of any cause; known as the flushing rosacea type or the S2 type), type 3 (burning, itching, or stinging of any cause; the S3 type), and type 4 (susceptible to developing contact dermatitis and irritant dermatitis and often associated with impaired skin barrier; the S4 type) (Table 2.3). It is important to note that patients can suffer from combinations of sensitive skin subtypes. For example, an individual may burn and sting and develop acne due to the use of particular skin care products. This person would be designated as an S1S3 sensitive skin type. The remainder of the sensitive skin discussion will focus on acne, rosacea, and the main class of topical treatments.
Table 2.3 Baumann sensitive skin classification
| Type 1 | Pimples and comedones |
| Type 2 | Flushing |
| Type 3 | Burning and stinging or itching |
| Type 4 | Impaired barrier, contact and irritant dermatitis |
Acne
Acne vulgaris, characterized by open or closed comedones as well as papules and pustules, is a multifactorial process involving the pilosebaceous unit. This most commonly reported skin disorder affects more than 17 million people annually in the US alone,89 and 75–95% of all teens are affected.90 Most patients outside this age range are adult women, who usually exhibit a hormonal aspect to their acne. Approximately 12% of women are affected by acne until the age of 44 compared to only 3% of men up to the same age.91 Acne caused by exposure to cosmetics was dubbed “acne cosmetica” by Kligman and Mills in 1972.92 In all cases, early and individually tailored treatment is required to achieve a satisfactory resolution and cosmetic appearance for the patient (Box 2.4).
Coconut oil and isopropyl myristate are among the numerous ingredients in skin care and hair care products that can exacerbate acne (Box 2.5). Some of the more comedogenic products include blushes, lipstick, and other color cosmetics that contain drug and cosmetic red dyes, which are derived from coal tar. In addition, sunscreen ingredients have been known to provoke acneiform eruptions.93 Another class of treatments, anti-inflammatories, will be discussed after the following section on another typical sensitive skin presentation, rosacea.
Rosacea
Known to afflict millions after the age of 30, rosacea is a chronic cutaneous disorder presenting as central facial erythema, telangiectasia, papules, pustules, flushing, and facial redness. It is often confused with acne. Rosacea is more common in fair-skinned than dark-skinned individuals. Risk factors for developing this condition include photodamage, a tendency toward facial flushing, and genetic predisposition. Aggravating factors include sunlight, heat, alcohol consumption, and spicy food (Box 2.6).
Box 2.6
• Rosacea treatment should combine in-office intense pulsed light treatments with an at-home regimen containing an anti-inflammatory cleanser, moisturizer, and sunscreen.
• A topical antibiotic such as metronidazole or an anti-inflammatory such as azelaic acid is added at night.
• Green tea and caffeine combinations are commonly used in serum and cream preparations.
• Avoidance of alcohol and spicy food should be stressed if these are triggers.
The precise causal pathways of rosacea remain unknown. Several etiologic factors have been implicated, including genetic predisposition, Demodex folliculorum mites, Helicobacter pylori infection, vascular lability, response to chemical and ingested agents, and psychogenic factors. This discussion will be limited to factors related to inflammatory pathways. While the digestive tract bacteria debate over H. pylori remains controversial, it has been suggested that intestinal inflammation and bacteria may induce hypersensitization of facial sensory neurons via the plasma kallikrein-kinin pathway and production of bradykinin, a well-known vasodilator.94,95 Further, matrix metalloproteinase-9 (MMP-9), also known as gelatinase, has been implicated in the pathophysiology of rosacea as elevated levels of MMP-9 have been noted in patients with ocular rosacea.96 An etiologic theory based on vascular response may be explained by a combination of factors such as the superficiality of cutaneous vasculature on the face,97 greater blood flow of facial skin,98 and vascular dysregulation via humoral and neural mechanisms causing vasodilatation.99–101 A recent study of rosacea patients revealed the presence of vascular endothelial growth factor (VEGF) receptors on vascular endothelium in addition to the expression of both VEGF and VEGF receptors on inflammatory cells.102 The investigators suggested that VEGF “receptor-ligand binding” may play a role in rosacea etiology. Topical antiangiogenic growth factors will likely be a target of future rosacea therapy research.103
In another recent study, investigators observed that individuals with rosacea express abnormally high levels of the proteins cathelicidin and SC tryptic enzyme (also called kallikrein 5), and showed that when both proteins are present in excess, aberrant enzymatic processing occurs and yields high levels of abnormal cathelicidin, which is proinflammatory, and clinically results in the erythema, inflammation, and vascular dilatation and growth characteristic of rosacea.104 Notably, increased cathelicidins in the case of psoriasis and decreased levels in the case of atopic dermatitis have been implicated in the pathophysiologic pathways of those conditions.105 Currently, approaches to modify cathelicidin production are under development. In the meantime, anti-inflammatories are a mainstay in multimodal rosacea therapy. (Table 2.4 provides a wider range of rosacea treatment modalities than can be covered in this chapter.) Just as there is variability in the type of sensitive skin that patients may exhibit, there is a wide range of anti-inflammatory treatments available to treat the symptom common to all types of sensitive skin.
Table 2.4 Rosacea treatment modalities
| Topical treatments |
| Antibiotics |
| Anti-inflammatories |
| Immunomodulators |
| Sulfur products |
Oral antibiotics
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|