This article provides an overview of current therapies for photodamaged facial skin and their efficacy, with particular focus on studies that use the objective, quantitative evaluation methods discussed in the previous article. The role of topically applied agents including prescription drugs and cosmetics is discussed. From this information, a schema for the relative effectiveness of therapeutic modalities in reducing perceived age is presented. This information assists the facial plastic surgeon in evaluating patient expectations and selecting the most effective program.
Key points
- •
Facial restoration uses a wide range of approaches albeit less technically effective than the gold standard of fully ablative laser modalities.
- •
Increasing the uniformity of facial skin coloration is an important treatment goal because it impacts the patient’s perceived age.
- •
Topically applied facial cosmetic products (eg, combinations of skin lightening agents, vitamins, and sunscreens) produce measureable reductions in the characteristics associated with photodamage.
- •
The literature contains many reviews of facial restoration modalities but there is limited information on what the experienced, skilled facial plastic surgeon might achieve with a total treatment package. Of great interest is the magnitude of the reduction in perceived age that could be achieved.
Introduction
Perceived age is the marker for facial skin aging. Treatments to reduce one’s perceived age and restore facial skin condition are highly sought. Surgeons have an armamentarium of methods for managing and optimizing facial skin color, uniformity, texture, and shape in restoring photodamaged skin. This article reviews the effectiveness of various treatment modalities including topicals (eg, cosmetics) in facial skin care. Studies are presented in the context of patient expectations for “decreasing perceived age.” A particular area of concern is dark spots (eg, solar lentigines, hyperpigmentation). Postinflammatory hyperpigmentation can occur with UV exposure and resultant epidermal inflammation, generation of reactive oxygen species, and stimulation of melanocytes. Solar lentigines (liver spots, age spots, actinic lentigines) are hyperpigmented spots caused by chronic UV exposure eventually becoming visible on the skin surface. Because of their association with increased age, individuals seek treatments including laser resurfacing, chemical peels, dermabrasion, and topical agents.
Treatments are designed to interact with the affected areas so as to change their characteristics or to “restore” the skin to a chronically earlier state at least temporarily and to prevent further damage. They may increase the levels of types I and II collagen or reorganize the collagen fibrils to decrease the severity of lines, reduce chronic inflammation, and smooth the surface (ie, reduce the observable features of photoaging, including wrinkling, dyschromia, dryness, rough surface texture, folds, and keratosis).
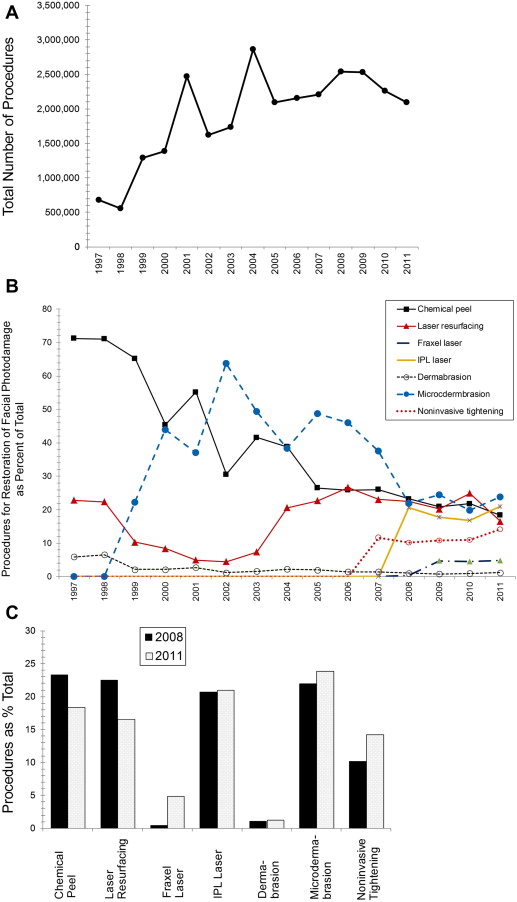
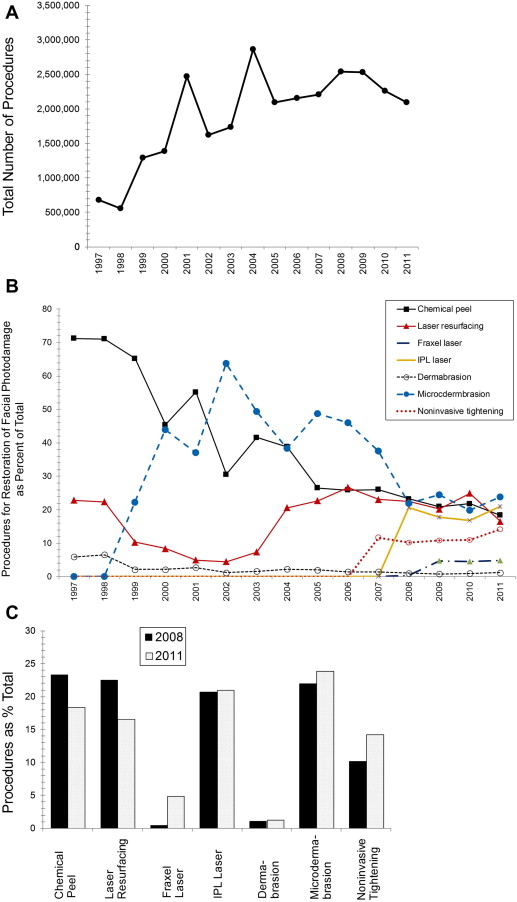
Current trends in the treatment of photodamage have been published annually by the American Society for Aesthetic Plastic Surgery since 1997. A total of 22,700 surveys were mailed in 2011 and the 1015 respondents included 384 dermatologists, 211 otolaryngologists, and 420 plastic surgeons. The procedures for photodamaged skin are chemical peels; laser resurfacing (ablative or nonablative); fraxel laser; intense pulsed light (IPL) laser; dermabrasion; microdermabrasion; and noninvasive tightening. Injections and fillers (ie, botulinum toxin, collagen, fat, hyaluronic acid, calcium hydroxylapatite, poly- l -lactic acid, and polymethyl methacrylate) have been excluded for the purposes of this discussion.
The total number of the procedures discussed here has increased since 1997 ( Fig. 1 A). The percentage of chemical peels decreased considerably between 1997 and 2005 and continues to decline (see Fig. 1 B). Laser resurfacing accounted for 23% in 1997, decreased to 4.5% in 2002, then increased to 23% in 2004, where levels currently remain. Dermabrasion was at 6.5% initially, but now accounts for about 1%. In contrast, microdermabrasion rose sharply from 0% in 1998 to 22% in 1999 to 44% in 2000, peaking at 64% in 2002 before declining to 23% in 2011. Between 2008 and 2011, the percent of chemical peels, laser resurfacing, IPL laser, and microdermabrasion were comparable (see Fig. 1 B,C). Between 2008 and 2011, the nonablative laser procedures increased to comparable levels as ablative procedures in 2001 ( Table 1 ).
| 2008 | 2009 | 2010 | 2011 | |
|---|---|---|---|---|
| Ablative | 18% | 27% | 36% | 51% |
| Nonablative | 82% | 73% | 64% | 49% |
This article provides an overview of the current therapies for photodamaged facial skin and their efficacy, particularly the studies using the objective, quantitative evaluation methods discussed in the previous article. The role of topical treatments and cosmetics is discussed because they are not reported by the American Society for Aesthetic Plastic Surgery. A schema showing the relative effectiveness of various modalities in decreasing perceived age is presented.
Introduction
Perceived age is the marker for facial skin aging. Treatments to reduce one’s perceived age and restore facial skin condition are highly sought. Surgeons have an armamentarium of methods for managing and optimizing facial skin color, uniformity, texture, and shape in restoring photodamaged skin. This article reviews the effectiveness of various treatment modalities including topicals (eg, cosmetics) in facial skin care. Studies are presented in the context of patient expectations for “decreasing perceived age.” A particular area of concern is dark spots (eg, solar lentigines, hyperpigmentation). Postinflammatory hyperpigmentation can occur with UV exposure and resultant epidermal inflammation, generation of reactive oxygen species, and stimulation of melanocytes. Solar lentigines (liver spots, age spots, actinic lentigines) are hyperpigmented spots caused by chronic UV exposure eventually becoming visible on the skin surface. Because of their association with increased age, individuals seek treatments including laser resurfacing, chemical peels, dermabrasion, and topical agents.
Treatments are designed to interact with the affected areas so as to change their characteristics or to “restore” the skin to a chronically earlier state at least temporarily and to prevent further damage. They may increase the levels of types I and II collagen or reorganize the collagen fibrils to decrease the severity of lines, reduce chronic inflammation, and smooth the surface (ie, reduce the observable features of photoaging, including wrinkling, dyschromia, dryness, rough surface texture, folds, and keratosis).
Current trends in the treatment of photodamage have been published annually by the American Society for Aesthetic Plastic Surgery since 1997. A total of 22,700 surveys were mailed in 2011 and the 1015 respondents included 384 dermatologists, 211 otolaryngologists, and 420 plastic surgeons. The procedures for photodamaged skin are chemical peels; laser resurfacing (ablative or nonablative); fraxel laser; intense pulsed light (IPL) laser; dermabrasion; microdermabrasion; and noninvasive tightening. Injections and fillers (ie, botulinum toxin, collagen, fat, hyaluronic acid, calcium hydroxylapatite, poly- l -lactic acid, and polymethyl methacrylate) have been excluded for the purposes of this discussion.
The total number of the procedures discussed here has increased since 1997 ( Fig. 1 A). The percentage of chemical peels decreased considerably between 1997 and 2005 and continues to decline (see Fig. 1 B). Laser resurfacing accounted for 23% in 1997, decreased to 4.5% in 2002, then increased to 23% in 2004, where levels currently remain. Dermabrasion was at 6.5% initially, but now accounts for about 1%. In contrast, microdermabrasion rose sharply from 0% in 1998 to 22% in 1999 to 44% in 2000, peaking at 64% in 2002 before declining to 23% in 2011. Between 2008 and 2011, the percent of chemical peels, laser resurfacing, IPL laser, and microdermabrasion were comparable (see Fig. 1 B,C). Between 2008 and 2011, the nonablative laser procedures increased to comparable levels as ablative procedures in 2001 ( Table 1 ).
| 2008 | 2009 | 2010 | 2011 | |
|---|---|---|---|---|
| Ablative | 18% | 27% | 36% | 51% |
| Nonablative | 82% | 73% | 64% | 49% |
This article provides an overview of the current therapies for photodamaged facial skin and their efficacy, particularly the studies using the objective, quantitative evaluation methods discussed in the previous article. The role of topical treatments and cosmetics is discussed because they are not reported by the American Society for Aesthetic Plastic Surgery. A schema showing the relative effectiveness of various modalities in decreasing perceived age is presented.
Literature review: treatments to restore facial skin
There are a considerable number of reviews on therapeutic modalities for photoaged skin. For example, in 2009, an entire issue of Facial Plastic Surgery (volume 25, issue 2) was devoted to the topic of rejuvenation. Table 2 lists several reviews and briefly describes the information provided in each. Next, the various modalities are discussed with the goal of addressing these questions: How effective are the treatments relative to each other? How much improvement can a consumer/patient expect against the goal of reducing perceived age? Can the treatment “tools” be combined to optimize outcomes? How much improvement could a patient potentially achieve on her or his own with commercially available facial skin care products?
| Category | Specific Modalities | Comments |
|---|---|---|
| Resurfacing, general | Fully ablative treatments Fractional lasers Nonablative lasers Dermabrasion Chemical peels Microdermabrasion Topicals | Covers mode of interaction with skin and targets of laser energy, penetration depth, histologic effects, qualifications of practitioners, risks and side effects, types of ablative lasers Includes sample photographs Reports results from investigations |
| Laser resurfacing | Ablative lasers | Provides a comprehensive, step-by-step review of procedures for the clinician, including patient assessment, preparation, postsurgery wound care, complications Emphasizes technique and asserts that skill in doing the procedure produces significant results |
| Laser resurfacing | Ablative CO 2 lasers Ablative Er:YAG lasers Combined CO 2 /Er:YAG Nonablative lasers | Reviews different types of lasers and mode of action, detailed description of settings and procedures, discusses efficacy |
| Laser resurfacing | Ablative lasers Nonablative lasers Fractional ablative lasers | History, types of lasers, histology, patient characteristics for specific modalities, extent of improvement, complications (eg, scarring), management after procedures, shows examples |
| Laser resurfacing | Fractional thermolysis | Reviews conditions, such as acne scars, fine wrinkles, dyschromia, melisma, hyperpigmentation, telangiectatic matting, residual hemangiomas, poikiloderma of Civatte, nevus of Ota Compares with fractional ablative treatment |
| Laser resurfacing | Fractional ablative | Discusses complications vs fully ablative methods |
| Laser resurfacing | Fractional ablative Fractional nonablative | Discusses history and uses for both Reports clinical findings and histology for multiple applications Comprehensive review of laser types, wavelengths, brands |
| Laser resurfacing | Nonablative fractional laser | Discusses mode of action and use on Asian subjects with Fitzpatrick types III, IV |
| Laser resurfacing | Nonablative | Provides an algorithm for treatment using nonablative methods |
| Chemical peels | Glycolic acid Trichloroacetic acid Phenol Resorscinol α-Hydroxy acid β-Hydroxy acid | Reviews superficial, midlevel and deep peels, mechanisms, histology, frequency, agents used for each level, preprocedural and postprocedural care, side effects, application strategies |
| Chemical peels | α-Hydroxy acid Trichloroacetic acid Baker-Gordon solution Phenol-Croton oil | Reviews history, patient selection criteria, skin classification scales, pretreatment and posttreatment, peel depth, peel agents, complications Compares with laser resurfacing Discusses application technique |
| Chemical peels | Glycolic acid Jessner solution Pyruvic acid Resorcinol Salicylic acid Trichloroacetic acid Phenol | Discusses variables that impact penetration of peel agent, comprehensive list of peel agents, patient characteristics impacting selection of agent Describes visual appearance postapplication and interpretation of depth Comprehensive advantages and disadvantages for each agent |
| Microdermabrasion | Crystals as agent | Describes equipment and operating premise Reviews current literature, describes the findings, comments on the quality of published literature Discusses safety |
| Postinflammatory hyperpigmentation | Chemical peels Laser treatment Hydroquinone Mequinol Retinoids Azelaic acid Kojic acid Arbutin Niacinamide N -acetylglucosamine Ascorbic acid (vitamin C) Licorice extract Soy Camouflage | Discusses epidemiology, etiology, visual characteristics, diagnosis, treatment with a variety of modalities and topical agents, adverse effects Presents clinical studies regarding outcomes of treatment Provides treatment algorithm |
| Photoprotection and topical agents | Hormone therapy Sunscreens Antioxidants Cell regulators Vitamins Retinoic acid | Provides comprehensive discussion of the mechanisms of photodamage, genes and metabolic pathways Effects of hormones Comprehensive list of sunscreen actives Detailed discussion of objective quantitative methods to measure changes, biomechanical assessment of elastic properties, measurement of skin barrier function |
| Photoprotection and topical agents | Sunscreens Retinoids Antioxidants: vitamin C, vitamin E, Idebenone α-Hydroxy acids | Discusses mechanisms of photoaging and the effects of each treatment on the skin biology Reviews literature and discusses results |
| Vitamins | Retinoids Carotenoids Vitamins C, E, B 3 , D, K | Review of the mechanisms of effect of UV radiation Comprehensive review of the literature for the effects of vitamins and discussion of the mechanisms of action |
| Over-the-counter skin care products | Retinol, retinaldehyde, retinyl palmitate α-Hydroxy acids Ascorbic acid (vitamin C) Vitamin E Niacinamide (B 3 ) α-Lipoid acid N -acetylglucosamine Resveratrol Flavenoids, soy isoflavones Grape seed extract Coffea arabica | Discusses general effects and potential mechanisms for photodamaged skin Reviews results of studies on effectiveness Comments on the need for more rigorous and additional studies on over-the-counter products |
| Individual and combined treatments | Injectables, side variety Chemical peels Ablative laser Nonablative laser | Comprehensive chart with methods, time to observable effect, mechanism of action, indications for use, benefits, adverse effects, length of time effects last (before repeat treatment is needed) Suggests combination of treatments |
For example, the effects of facial restoration procedures on perceived age were objectively determined from images of 75 patients. Naive judges (198) evaluated before and after (6 months posttreatment) photographs presented individually but not in pairs. The mean decrease in perceived age was 6 years, with a range of 0.8 to 14.2. Reductions were 4.6 years for facelift; 2.5 for laser resurfacing; and 2 years each for fat injection, eyelid surgery, and forehead lift.
Therapeutic Modalities: Mechanism of Effects
Facial restoration procedures typically alter structures in the dermis, epidermis, and stratum corneum (SC) and vary by depth of effect. Fully ablative lasers (eg, CO 2 , erbium:YAG [Er:YAG]) remove the entire epidermis, the papillary dermis, and part of the reticular dermis depending on energy settings and thermal effects. Removal of the epidermis and part of the dermis promotes collagen formation. Damage to the epidermis (eg, ablation and removal of the SC) produces inflammation whereby the fibroblasts are induced to produce collagen 1 and 4 and stimulates formation of keratinocytes. Fractional ablative lasers apply energy in a grid pattern thereby preserving much of the epidermis and SC and destroying tissue in columnar patterns into the dermis. In nonablative laser resurfacing, columns of thermal energy are directed into the dermis thereby using heat to create epidermal and dermal damage to levels of 300 to 400 μm. The technique of dermabrasion penetrates into the dermis thereby stimulating collagen formation. In contrast, microdermabrasion is a more superficial technique and removes only the SC. Depending on the technique and type of microdermabrasion, selective removal of the SC may occur. Partial SC loss enhances the penetration of topical agents and microdermabrasion may be performed for this purpose.
Prevention: Photoprotection
Daily application of sun-protective agents (ie, UVA and UVB filters) reduced type I procollagen, increased extracellular matrix proteins, and prevented increases in the thickness of the SC and stratum granulosum. The facial skin of females living in higher UV regions had significantly longer wrinkles, more wrinkles, more and larger hyperpigmented spots, more yellow coloration, and rougher surface texture by quantitative imaging and analysis than those with lower UV levels. Regular, daily sunscreen use leads to reduced UV exposure, although the effects on facial skin characteristics have not yet been reported. Protection of additional UV damage is an essential treatment component.
Laser Resurfacing
Ablative laser resurfacing
Ablative CO 2 lasers and ablative Er:YAG lasers are considered to be highly effective, “best in class” treatments for photodamage. Examples of the results are discussed next.
Female subjects (n = 67) with periorbital rhytides were treated one time with a high-energy pulsed CO 2 laser (3 mm; fluence, 500 mJ/cm 2 ; 7-mW power) and evaluated at 1, 3, and 6 months. Paired comparison evaluation of high-resolution photographs for severity (10-point scale: 1–3 mild, 4–6 moderate, 7–9 severe) showed significant improvement at 6 months. The extent of improvement was directly related to the pretreatment severity.
Subjects (n = 47) with periorbital, perioral, or glabella rhytides were treated once with a CO 2 laser with flashscanner (3-mm spot size; 7.5 W; 0.2-second pulse duration or 6-mm spot at 18–20 W). Pretreatment and posttreatment (mean, 9.7 weeks; range, 1–24) photographs were viewed together by five judges and evaluated for wrinkle improvement (0 = none, 1 = less than 25% improvement, 2 = 25%–50% improvement, 3 = 50%–75% improvement, 4 = greater than 75% improvement) and interpreted as none (0), poor (0.1–1), fair (1.1–2), good (2.1–3), and excellent (3.1–4). Mean scores after 1 month were 3.3 for periorbital, 3.1 for perioral, and 3.1 for glabella, indicating excellent improvement. Erythema was judged as none (0); mild (1); moderate (2); or severe (3). The highest mean erythema score was 1.27 at 4 to 12 weeks postsurgery and 0.9 at 12 to 24 weeks, indicating that visible redness lasted for up to 6 months.
The effects of treatment with ablative CO 2 lasers (pulse, 800 μs; fluence, 3.5–6.5 J/cm 2 ; 250–450 mJ pulse energy) and Er:YAG (300 μs; 5–8 J/cm 2 ; 1–1.5 J per pulse) were compared using a split face design in females (n = 21) with periorbital or perioral rhytides. A panel of five physicians evaluated pretreatment and posttreatment photographs on a five-point scale (1 = poor improvement, 2 = fair, 3 = good, 4 = excellent, 5 = complete resolution of wrinkles). The improvement was significantly greater for the CO 2 laser versus the Er:YAG treatment. The occurrence of erythema was significantly lower for the Er:YAG side, as was the incidence of hyperpigmentation.
Ablative laser CO 2 resurfacing was compared with dermabrasion for perioral wrinkles with a split-face design (n = 20) using high-quality photographs, biophysical measures of skin color, hydration, and mechanical properties and patient assessment. Masked evaluation of photographs by 10 plastic surgeons indicated that the laser treatment had a significantly higher erythema score at 1 month and a small but significantly greater improvement in perioral wrinkles at 6 months. Sixty-five percent of subjects believed the laser treatment to be more effective.
Fractional laser resurfacing
Subjects with moderate to severe photodamage were treated two to three times with ablative fractional therapy (10,600 nm; 30-W power; 500-μm pitch; 1000–1500 μs; forced cold air). Photographs were evaluated 6 months after treatment for dyschromia, texture, and laxity using the grading scale of Alexiades-Armenakas. Significant improvement was found for multiple characteristics of photoaging (ie, dyschromia [grade 1.5 after vs 3.2 before]; texture [grade 1.7 from 3.3]; laxity [grade 1.5 from 3.1]; and overall outcome [1.5 from 3.3]).
Two ablative fractional lasers (CO 2 and Er:YAG) were compared using a paired-comparison split-face design among 28 patients with mild to moderate periorbital wrinkles as judged with the Fitzpatrick Wrinkle Scale. Both treatments produced a significant reduction in wrinkle score (4.8 before vs 4.3 after for CO 2 ; 4.6 before vs 4.3 after for Er:YAG), although the differences were small and the variability among the population seemed to be high. Wrinkle depth by optical profilometry was significantly reduced for both (2 mm before and 1.64 mm after for CO 2 ; 2 mm before and 1.6 mm after for Er:YAG). Interestingly, the variability was lower for the Er:YAG laser. The treatments were comparable and the investigators concluded that multiple treatments are probably needed thereby countering the benefit of reduced down time (vs conventional ablative therapy).
Compared with conventional ablative therapy, ablative fractional lasers are considered to be somewhat less effective for facial skin restoration but have fewer potential complications (eg, scarring, hypopigmentation, and higher recovery times). In reviewing the literature, there appear to be no reports directly comparing the two methods.
Nonablative laser treatment
Nonablative laser treatments can generally target specific issues, such as hyperpigmentation of telangiectasia or diffuse redness. They can also operate in the infrared wavelength region. Nonablative lasers are considered to be less effective than laser resurfacing for correction of photoaging. However, a recent review indicated that there were no reports comparing the two methods.
An Er:YAG laser in the thermal mode with 2.1 or 3.1 J/cm 2 and parallel air cooling was used to treat photodamaged skin (wrinkles) or scars in the periorbital or perioral regions. The two treatments were 2 months apart with follow-up over 12 months. Good improvement was seen by 19% subjects with wrinkles and 31% reported no improvement. Of the subjects with scars, 50% reported good improvement and 100% had some improvement.
The effects of six mini-peels at 2-week intervals using an Er:YAG 2940-nm laser in the thermal mode (series of short pulses with energies of 2–3 J/cm 2 of 200–250 millisecond duration) were evaluated among six females. The subjects reported an improvement in skin tightening, periorbital wrinkles, and appearance but the magnitude had decreased after 3 months, indicating the need for repeated treatments.
Nine patients with periorbital wrinkles were treated three times (at 3-week intervals) with a nonablative 1450-nm diode laser (4-mm spot size; 14–18 J/cm 2 ; cooling). Pairs of pretreatment and posttreatment images were evaluated by 25 dermatologists and the posttreatment appearance was found to be superior ( P <.05). Two physicians rated the posttreatment images higher. Seven subjects reported mild and two indicated moderate improvement. Note that the perceived outcomes differed for physicians versus patients.
IPL treatment
Treatment with an Er:YAG laser (micropeel) at 3.8 J/cm 2 and 15 μm per pass was compared with an IPL laser at 30 J/cm 2 with a 2.4- and 4-millisecond pulse (10-second delay, no cooling) in a split-face design among 10 patients. Images collected with standard photography (VISIA) showed an improvement in dyschromia after one treatment for IPL and no change for the Er:YAG laser. No change in wrinkles was seen, perhaps because of the relatively low energy settings.
Korean subjects were treated with IPL in the range of 530 to 950 nm at 15.5 to 17.5 J/cm 2 (5 pulses, 20-second duration) three times at 4-week intervals. Patient self-assessment showed that mottled pigmentation improved in 26.3% and slightly improved in 57.9%, skin tone improved in 15.8% and slightly improved in 57.9%, number of lesions improved in 31.6% and slightly improved in 36.8%, and lightening of lesions improved in 31.6% and slightly improved in 52.6%. For skin elasticity, wrinkles, and skin rejuvenation, at least some improvement was observed by 57.9%, 47.4%, and 63.2%, respectively. Melanin index and skin lightness by objective measurement were significantly reduced and skin elasticity was increased ( P <.05).
A set of bipolar radiofrequency-based optical devices (IPL, infrared light, diode laser) was used to treat one side of the face at four 3-week intervals in Asian subjects. Significant decreases were found for fine wrinkles and dyschromia from global assessment of photographs and instrumental measurement of melanin indices. Skin elasticity (objective assessment) increased with treatment and histology showed thicker collagen and more fine elastic fibers.
The effects of a long-pulse pulsed dye laser (595 nm; spot 7 mm; compression, 9–12 J/cm 2 ; duration 1.5 milliseconds for lentigines; 10–12 J/cm 2 and 20-millisecon duration, stacked methods for wrinkles) and IPL (fluence, 27–49 J/cm 2 ; duration 20 millisecond) were compared among 10 Asian females in a split-face design. The improvement in lentigines was significantly greater for the long-pulse pulsed dye laser (81%) than the IPL (62.3%), as measured by evaluation of clinical photographs. The devices were comparable for the effects on wrinkles.
Home use nonablative laser
An over-the-counter home use 1410-nm midinfrared nonablative laser (12–15 mJ/μb) was evaluated among 124 subjects with periorbital wrinkles who had not had any type of facial resurfacing procedures for 2 years. Treatments were daily for 4 weeks and twice weekly for 12 weeks, with evaluations at weeks 4, 12, 16, 20, and 28. Wrinkles were evaluated in live subjects or from high-resolution digital images using the 0 to 9 category Fitzpatrick Wrinkle Scale (scores: 1–3 fine wrinkles, mild elastosis to 7–9 fine/deep wrinkles, severe elastosis). The mean score reduction was 0.8 at 4 weeks and 1 at 8 weeks. The magnitude of the improvement could not be fully assessed because of the lack of a control group.
Microdermabrasion
Tissue removal with microdermabrasion was examined and differences were observed as a function of technique. Specifically, (1) complete SC removal occurred with the mobile tip application procedure; (2) epidermal blistering and an intact SC with stationary application at 30 kPa (3 seconds) vacuum pressure; and (3) removal of the SC and much of the viable epidermis with the stationary procedure at 45 kPa.
This result confirms the experience of practitioners (i.e, that a resurfacing method may produce different effects or degrees of improvement based on operator technique). The finding may explain, in part, why microdermabrasion and light chemical peels are considered to produce a relatively small change in photoaged skin by physicians and patients.
Treatment of photodamaged facial skin (n = 17) with serial (eight at 1-week intervals) microdermabrasion significantly improved skin coloration as judged by experts (plastic surgeons) and patients on a 0 to 5 scale. Improvement in wrinkles was seen only by patients.
Six serial weekly microdermabrasion treatments (n = 16) significantly improved fine wrinkles, dullness, hyperpigmentation, blotchiness, milia, and pore size as judged by physicians on 0 (none) to 9 (severe) grading scales. The lack of a control group limits the ability to determine the magnitude of the effects. Microdermabrasion is intended to remove the entire SC. Because treatment occurred at weekly intervals, it is unlikely that full restoration of the SC could occur before the next treatment and removal of any SC that had formed.
Chemical Peels
Over time, the types of facial skin restoration procedures have changed. The percentage of chemical peels has decreased because of development of laser resurfacing approaches, although some facial plastic surgeons believe the chemical peel continues to be an important tool. Superficial chemical peels interact with and remove the SC only (ie, very superficial peels) and part of the epidermis. Chemical peels of medium depth remove the epidermis and have effects into the reticular (upper part) of the dermis. Mixtures of glycolic acid (70%) and trichloroacetic acid (35%) applied sequentially are considered to be effective because the glycolic prepared the skin to permit more uniform penetration of the trichloroacetic acid. This combination peel reduced fine wrinkles but not deeper wrinkles. Deep peels remove the SC, viable epidermis, reticular dermis, and part of the papillary dermis. The effectiveness of a given peel depends on preparation of the skin in advance. For example, topical application of retinoic acid before the peel (eg, 4 weeks) facilitates penetration of the peel agent.
Five superficial peels (30% glycolic, 2-week intervals) were compared with single midlevel peel (35% trichloroacetic acid) in a split-face design using quantitative objective measurements of skin condition and actinic damage. Image analysis showed significantly greater improvement in wrinkles with the trichloroacetic acid but patients were more satisfied with the serial superficial peels. Both treatments increased skin elasticity and hydration.
Topical Treatments
Definitions and regulations
Topically applied agents (ie, topicals) are widely defined in this section as being put on the skin surface. They are typically in the form of lotions, gels, creams, or ointments designed to be rubbed into the skin. They may include prescription drugs; over-the-counter products; cosmetics (including colorants); and “cosmeceuticals.” Drugs are regulated by agencies, such as the Food and Drug Administration (FDA), and undergo a rigorous process to demonstrate safety and effectiveness. In general, cosmetics are developed, evaluated, and marketed by the skin care industry. In the United States, cosmetics are regulated by the FDA’s Center for Food Safety and Applied Nutrition and must comply with safety and labeling guidelines. Cosmetic products are not allowed to make drug claims. Interestingly, most of the skin research is conducted by the skin care industry, as opposed to academic medical institutions. The term “cosmeceutical” may be used to describe a topical product but cosmeceuticals are not recognized or regulated by the FDA. The term “cosmeceutical” was originally considered to describe something with the following characteristics : (1) scientifically designed and intended for external application; (2) produces a useful, desired result; (3) has desirable aesthetic properties; and (4) meets rigid chemical, physical, and medical standards. The following sections include topicals that are prescription, cosmetic, or cosmeceutical.
Prescription topicals
Topical tretinoin (all- trans -retinoic acid, the acid form of vitamin A) is effective for the mitigation of mild to severe photodamage at levels of 0.02% and higher as demonstrated in multiple randomized controlled trials. The clinical effects are caused by an increase in new collagen, restoration of normal elastic components, normalization of melanocyte structure, increased thickness of the epidermis and stratum granulosum, and increased denseness of the SC. Because skin irritation (eg, erythema, stinging, burning, dryness) is a noted side effect, doses must be titrated to determine tolerable levels.
Hydroquinone, a tyrosinase inhibitor, has been used extensively for hyperpigmentation at prescription levels of 3% to 10% and over-the-counter at 2%. In 2001, the European Union banned the use of hydroquinone, as did authorities in Japan. In 2006, the US FDA proposed to remove hydroquinone from the generally recognized as safe list and require new drug applications for use. This proposal was based on newer reports describing carcinogenic and mutagenic effects. At the request of the FDA, the National Toxicity Program is conducting specific studies to address the safety concerns.
Deoxyarbutin, a synthetic derivative of naturally occurring arbutin, has been synthesized and incorporated into a variety of formula matrices. Deoxyarbutin was less cytotoxic/cytostatic than hydroquinone in human melanocyte culture systems while effectively inhibiting tyrosinase activity and melanin content to a greater extent. Skin lightening, following the development of postinflammatory hyperpigmentation caused by wounding, was demonstrated in a human xenograft model. Treatment of UV-induced pigmentation (tanning, human subjects) with deoxyarbutin led to significantly greater skin lightening that was reversible when treatment was discontinued. In contrast, hydroquinone initially lightened the skin but darkening occurred with additional treatment, presumably caused by irritation and the resulting postinflammatory hyperpigmentation. Two other skin lightening agents, kojic acid and native arbutin, were ineffective in this model. There are currently very few published human trials of deoxyarbutin and evaluation of its effectiveness for solar lentigines and postinflammatory hyperpigmentation are warranted. An extensive human safety assessment indicated that deoxyarbutin does not seem to pose the risks identified for hydroquinone and some believe it to be the most effective skin lightening compound.
Two skin care systems for hyperpigmentation were evaluated in parallel groups of females with at least mild photodamage over 12 weeks. Products were SkinMedica Hyperpigmentation System (SkinMedica, Inc., Carlsbad, CA, USA) (n = 17) with cleanser, 4% microentrapped hydroquinone with retinol and antioxidants, sunscreen of SPF 30 and tri-retinol at 1.5%; and Obagi Nu-Derm System (Obagi Medical Products, Inc., Long Beach, CA, USA) with cleanser, toner, clear hydroquinone at 4%, exfoliant, blender hydroquinone at 4%, sunscreen of SPF 35 and tretinoin at 0.025% (n = 18).
Relative to the starting condition, both systems resulted in significant reduction of hyperpigmentation, global photoaging, sallowness, and scores of “marked improvement” and “almost cleared” as judged by physicians. There was no change in fine wrinkles. Burning-stinging scores were higher at Week 8 for the Obagi system and peeling was higher at Week 12 for the SkinMedica system. The subject evaluations paralleled the physician assessment. No other differences between the systems were noted.
Nonprescription topical treatments: cosmetics
Antioxidants: vitamin C
Topical daily application vitamin C (10% ascorbic acid and 7% tetrahexyldecyl ascorbate in an anhydrous polysilicone vehicle) was compared with the vehicle in a split-face study among 10 subjects with moderate photodamage for 12 weeks. Significant improvements in wrinkles were noted for the treatment in the periorbital, perioral, and cheek regions relative to baseline and for the placebo in the periorbital sites. Overall, the vitamin C treatment produced a directional improvement in wrinkles versus the vehicle ( P = .08). The treatments did not impact skin pigmentation. Four of 10 subjects judged the treatment side to be improved.
Vitamins and mixtures
Topical application of 2% niacinamide significantly reduced the percent area of hyperpigmentation after 4 and 8 weeks of treatment relative to baseline and the vehicle control in a split-face trial. Relative to a vehicle control, the use of 5% niacinamide for 12 weeks led to significant reductions in percent area of hyperpigmentation (image analysis), red blotchiness (expert evaluation), total wrinkle line length (image analysis), and yellow skin color (analysis of b* channel images), and increases in skin elasticity (biomechanical measures) and elastic recovery. A combination of 5% niacinamide (vitamin B 3 ) and 1% N -undecylenol phenylalanine, shown in vitro to reduce melanin production by melanocytes, was compared with niacinamide alone and vehicle among groups of Asian (Japanese) and white subjects with photodamage in a split-face design. The combination treatment reduced the percent area of hyperpigmentated spots to a greater extent than niacinamide alone or the vehicle in both groups after 8 weeks. A lotion containing 4% niacinamide, 0.5% panthenol (provitamin B 5 ), and 0.5% tocopherol acetate (vitamin E acetate) was compared with a moisturizer vehicle among 207 women aged 30 to 60 years from India (baseline skin lightness greater than 51 from the L scale of a standardized color image) over 10 weeks. These features of photoaging were reduced: percent area of hyperpigmented spots; percent area of melanin-specific spots (measured using spectrophotometric intracutaneous analysis); fine lines/wrinkles (expert visual assessment); and skin texture (expert assessment). Skin lightness (L value) and evenness of skin tone both increased with treatment. Importantly, the use of moisturizer (ie, a cosmetic) without sunscreen also reduces the features associated with photodamaged facial skin.
Prescription versus cosmetics
Tretinoin at 0.02% (Renova; Ortho Dermalogics, Los Angeles, CA, USA) and an SPF 30 moisturizing sunscreen (Neutrogena Healthy Defense Daily Moisturizer SPF; Neutrogena Corporation, Los Angeles, CA, USA) both applied daily were compared with a cosmetic regimen for 8 weeks among 197 females (40–65 years, parallel groups) with moderate to moderately severe periorbital wrinkles. A subset of 25 subjects from each group continued treatment for another 16 weeks. The cosmetics were three commercially available products each containing niacinamide (vitamin B 3 ), palmitoyl-lysine-threonine and palmitoyl-lysine-threonine-threonine-lysine-serine and carnosine. Product 1: daytime lotion with additional ingredients for SPF 30, vitamin C, and vitamin E (Olay Professional Pro-X Age Repair Lotion SPF 30, Procter & Gamble Company, Cincinnati, OH, USA). Product 2: a night cream with the four ingredients (Olay Professional Pro-X Wrinkle Smoothing Cream, Procter & Gamble Company, Cincinnati, OH, USA). Product 3: a wrinkle treatment with the four components plus retinyl propionate (Olay Professional Pro-X Deep Wrinkle Treatment, Procter & Gamble Company, Cincinnati, OH, USA) twice a day. After 8 weeks, the appearance of fine lines and wrinkles was judged by experts to be improved for both treatments. A higher number of subjects on the cosmetic regimen had a minimum positive grade of +1 and more had improvements two grades or greater. By image analysis, the cosmetic group had a significantly greater reduction in periorbital wrinkle area fraction. Both groups had improvements in deep wrinkles. The subject assessments of eye lines and wrinkles, overall skin feel, and overall appearance were larger for the cosmetics. The SC barrier integrity was poorer for the tretinoin group, measured as transepidermal water loss (TEWL), compared with baseline and unchanged for the cosmetics. For the 25 subjects per group who continued, there were no treatment differences at Weeks 16 and 24.
Combinations: Skin Resurfacing and Topical Treatments
The effects of topical vitamin C applied after fraxel laser treatment of photodamage were evaluated among 44 Korean women. Subjects received two treatments 4 weeks apart with power of 26 to 27 W, duration of 500 to 800 μs, and spacings of 400 to 650 μm. One group applied a vitamin C–containing treatment three times daily. Both groups used SPF 30 sunscreen and moisturizer use was permitted. Measures of SC barrier integrity differed significantly for the two groups (ie, increases in TEWL were lower [less compromise] and pH changes higher for the vitamin C group). At posttreatment week 4, TEWL had not returned to prelaser treatment values indicating ongoing restoration of epidermal barrier function. The conclusion was that vitamin C assisted in skin recovery but it was not clear whether these effects could be attributed to difference in moisturizer or vehicle effects between the groups.
IPL treatment alone was compared with IPL treatment in combination with injected treatments (ie, vitamin C, hyaluronic acid [low molecular weight], and β-glucan) and the combination was found to produce more positive results. One hundred women (56.3 years median) were divided into two groups (matched for age, skin type, and photodamage) and treated as follows. Treatment 1 (n = 40) consisted of seven sessions of IPL of three to four passes at 550-nm cutoff at 2-week intervals. Treatment 2 (n = 60) consisted of with IPL (same settings) seven times at 2-week intervals and low-intensity diode light (623 nm and 40 mW/cm 2 ) nine times (alternating weeks of IPL) and 10 to 15 injections into the superficial and deep dermis. Patients and physicians (from photographs) rated satisfaction on a 0 (none) to 5 (excellent) scale. The patients scored the combination treatment significantly higher for positive results than the IPL treatment along. The physicians judged the combination significantly higher for facial skin texture and firmness ( Table 3 ). No differences were observed between the treatments for hyperpigmentation and telangiectasia by physicians but both received a high percent of positive results.






