(1)
University of Florida, College of Medicine, Gainesville, FL, USA
(2)
Private Practice:, Orlando, FL, USA
7.1 Anti-Infective Medications
A. Antibiotics
Side effects (SE) listed are either most common or serious
Penicillins (PCNs)
Binds and inactivates bacterial enzymes (PCN-binding proteins) involved in peptidoglycan synthesis → inhibits bacterial cell wall synthesis
Contains β-lactam ring; drug excretion via kidneys; specific types of PCNs:
PCNs with β-lactamase inhibitor: amoxicillin and clavulanate (Augmentin)
Penicillinase-resistant PCNs: dicloxacillin, methicillin, oxacillin
Spectrum: gram-positive (GP) bacteria and spirochetes
Treats: erysipeloid, anthrax, strep/staph infections, cat/dog/human bites
SE: morbilliform eruption, angiodema, anaphylaxis, hemolytic anemia, interstitial nephritis, acute generalized exanthematous pustulosis (AGEP), toxic epidermal necrolysis (TEN)
Contraindication (CI): hypersensitivity to any β-lactam antibiotic; pregnancy category B
Cephalosporins
Contains β-lactam ring with same mechanism as PCNs; 10% cross-reactivity w/ PCNs
Spectrum of bacterial coverage based upon generation of cephalosporin:
1st generation: GP > gram-negative (GN); 2nd generation: GP = GN; 3rd generation: GP < GN; 4th generation: GP, GN (little activity against β-lactamase)
Adverse effects: AGEP, morbilliform eruption (serum sickness associated w/ cefaclor)
CI: same as with PCNs; pregnancy category B
Minocycline treatment of choice for CARP (confluent and reticulated papillomatosis of Gougerot-Carteaud)
Tetracyclines (TCNs)
Binds bacterial ribosomal unit (30s) → blocks bacterial protein synthesis
Spectrum: GP/GN bacteria, Chlamydia, Mycoplasma, rickettsia, spirochetes (syphilis, Lyme disease), certain mycobacteria (leprosy); different types of TCNs:
Doxycycline: excreted in GI tract, so can use in renal failure patients; photosensitivity
Tetracycline: most common to cause fixed drug eruption and may cause onycholysis, contraindicated in patients < 9 y/o due to brown discoloration of gingival third of teeth; photosensitivity
Minocycline: side effect includes blue-black pigmentation of skin/teeth (green-gray discoloration of mid-portion of teeth), drug-induced LE, autoimmune hepatitis
Demeclocycline: most phototoxic (then doxycycline)
↓ Absorption with Fe/Ca2+; pregnancy category D
Macrolides
Binds bacterial ribosomal unit (50s) → blocks protein synthesis; alternative for PCN-allergic patients; spectrum: GP/GN bacteria, spirochetes, atypical mycobacteria
Adverse effects: cholestatic hepatitis (estolate form of erythromycin), nausea, diarrhea
Inhibits cytochrome p450: ↑ levels of p450 substrates like cyclosporine, anticonvulsants, warfarin, digoxin, benzodiazepines, HMG-CoA reductase inhibitors, theophylline (latter combination can cause cardiac arrhythmias); erythromycin + lovastatin → rhabdomyolysis; clarithromycin + CCBs → bradycardia, hypotension
Pregnancy category C (clarithromycin), category B (erythromycin, azithromycin)
Fluoroquinolones (FQs)
Inhibits bacterial DNA gyrase; spectrum: GN bacteria, strep/staph, certain mycobacteria
Adverse effects: tendon rupture, cartilage damage in joints, ↑ LFTs, nephrotoxicity
Contraindication: pregnancy and children (due to deposition of drug in cartilage)
↓ Absorption with antacids, iron, sucralfate; inhibits CYP1A2 so ↑ levels of following drugs taken concomitantly: warfarin, aminophylline, theophylline; may also ↑ levels of procainamide; if taken with cyclosporine may increase renal toxicity
Pregnancy category C
Clindamycin
Binds bacterial ribosomal unit (50s) → blocks protein synthesis
Spectrum: GP and anaerobic bacteria
SE: pseudomembranous colitis (oral form); pregnancy category B
Only drug bactericidal to M. leprae
Rifampin (Rifampicin)
Inhibits RNA synthesis by inhibiting DNA-dependent RNA polymerase
Spectrum: mycobacteria (tuberculosis and leprosy)
SE: orange-red discoloration of urine/tears, ↓ OCP efficacy; pregnancy category C
Aminoglycosides
Binds bacterial ribosomal unit (30s) → blocks protein synthesis; used mainly in topical form
Spectrum: aerobic GN bacteria; SE (oral): ototoxicity, nephrotoxicity; pregnancy category D
Sulfonamides
Sulfamethoxazole and sulfasalazine; interferes with bacterial folic acid synthesis (needed for nucleic acid synthesis) by inhibiting dihydropteroate synthetase
Spectrum: GP/GN bacteria, Chlamydia, Nocardia
SE: hemolytic anemia (especially if G6PD deficient), nephrotoxicity, hepatotoxicity, TEN, Stevens-Johnson syndrome (SJS), AGEP, photosensitivity
Contraindication: hypersensitivity to medication, pregnancy (3rd trimester)
Pregnancy category C (D in third trimester)
Dapsone
Antibacterial and anti-inflammatory (mainly toward neutrophils by inhibition of myeloperoxidase); sulfone family (related to sulfonamides); spectrum: mycobacteria
Treats: leprosy, dermatitis herpetiformis, autoimmune blistering diseases, erythema elevatum diutinum, pyoderma gangrenosum
SE: hemolytic anemia (esp if G6PD deficient), cholestatic jaundice, methemoglobinemia, agranulocytosis (2-12 weeks after continuous treatment), motor peripheral neuropathy, acute psychosis, dapsone hypersensitivity syndrome, photosensitivity
Pregnancy category C
Vancomycin
Inhibits bacterial cell wall synthesis; only given intravenously; spectrum: GP bacteria
SE: red man syndrome, anaphylaxis, TEN, ototoxicity, phlebitis at IV site
Pregnancy category B
Metronidazole (Flagyl)
Forms toxic metabolites in bacteria, which inhibit nucleic acid synthesis
Spectrum includes anaerobes and protozoaSE: hypersensitivity, glossitis, disulfiram-like reaction (with alcohol) pregnancy category B
Pregnancy category C
Clofazimine (Lamprene)
Unclear mechanism; used for leprosy, erythema nodosum leprosum, DLE; category C
Linezolid
Inhibits protein synthesis but unique in that blocks initiation of protein production in bacteria
Reserve antibiotic used for serious infections caused by gram positive bacteria that are resistant to other antibiotics
SE (long term use): bone marrow suppression and thrombocytopenia
Pregnancy category C
B. Antifungals
Table 7-1:
Oral Antifungal Drugs
Name | Mechanism of Action | Characteristics |
|---|---|---|
TRIAZOLES | ||
Itraconazole (Sporanox) | Blocks ergosterol synthesis by inhibiting 14α-demethylase | Fungistatic, lipophilic, needs acidic milieu for absorption SE: ↑ LFTs, ↓ WBC, ↑ TG, nephrotoxicity, CHF worsening Tx: dimorphic fungi, aspergillosis, candidiasis, superficial dermatophytes, onychomycosis, sporotrichosis |
Voriconazole | Inhibits cyt p450 (↑ levels of digoxin, cyclosporine, etc) Category C | SE: visual disturbances |
Fluconazole | Inhibits cyt p450 (↑ levels of digoxin, cyclosporine, etc) Category C | Fungistatic, crosses blood-brain barrier Tx: candidiasis, pityriasis versicolor (PV), cryptococcosis, histoplasmosis, superficial dermatophytes, coccidioidomycosis |
IMIDAZOLES | ||
Ketoconazole | Inhibits 14α-demethylase Category C | Fungistatic, lipophilic, needs acidic milieu for absorption, ↑ absorption with food, inhibits cytochrome p450 SE: fulminant hepatitis (rare), ↑ LFTs (15%), gynecomastia Tx: dermatophytes, candidiasis, dimorphic fungi, PV |
ALLYLAMINES | ||
Terbinafine (Lamisil) | Inhibits squalene epoxidase (1st step of ergosterol synthesis) Category B | Fungicidal, biotransformed in liver, does NOT inhibit cyt p450 SE: nausea, metallic taste, liver damage, drug-induced LE Tx: onychomycosis, tinea corporis, tinea pedis |
POLYENES | ||
Amphotericin B | Binds ergosterol and forms membrane pores Category B | SE: acute reaction after infusion (fever, chills, nausea, tachypnea), nephrotoxicity, agranulocytosis, seizures, arrhythmias |
OTHERS | ||
Caspofungin | Inhibits synthesis of glucan (fungal cell wall) Category C | IV administration Tx: candidiasis and aspergillosis |
Griseofulvin | Disrupts microtubule function (metaphase arrest) Category C | Fungistatic, ↑ absorption w/ fatty meal, induces cytochrome p450 (may ↓ warfarin level), resistance seen in T. rubrum SE: headache, paresthesias, photosensitivity, drug-induced LE, worsens acute intermittent porphyria Tx: dermatophytes (NOT yeast or bacteria) |
C. Antivirals (Table 7.2)
Table 7-2:
Oral Antiviral Drugs
Name | Mechanism of action | Spectrum, category | Miscellaneous |
|---|---|---|---|
Acyclovir | Phosphorylated by viral thymidine kinase to acyclovir monophosphate, which blocks viral DNA polymerase → stops viral DNA synthesis | Herpes simplex virus (HSV), varicella-zoster virus (VZV) Pregnancy category B | SE: IV infusion associated with reversible obstructive nephropathy, rarely may see severe CNS changes (ie. seizures) |
Valacyclovir | Prodrug of acyclovir, same mechanism of action (viral thymidine kinase-dependent activity) | HSV, VZV, cytomegalovirus (CMV) Category B | Better bioavailability than acyclovir SE: TTP/HUS* seen in advanced HIV disease and transplant patients taking high doses |
Penciclovir | Phosphorylated by viral thymidine kinase (similar mechanism to acyclovir) | HSV, VZV | Low bioavailability so typically used in topical form |
Famciclovir | Prodrug of penciclovir with same mechanism as above | HSV, VZV Category B | Better bioavailability than penciclovir |
Gancyclovir | Phosphorylated by viral thymidine kinase; same mechanism as above | CMV (retinitis and CMV prophylaxis in transplant pts) Category C | Better activity against CMV than acyclovir; ↓ oral bioavailability SE: neutropenia, bone marrow suppression, mucositis, thrombocytopenia, seizures hepatic dysfunction |
Foscarnet | Noncompetitive inhibition of viral DNA polymerases; analogue of pyrophosphate Does not require phosphorylation so active against acyclovir-resistant viruses | CMV (retinitis), resistant HSV, resistant VZV Category C | Only IV form; active against infections resistant to acyclovir, famciclovir, ganciclovir SE: penile ulcerations or erosions, nephrotoxicity |
Cidofovir | Nucleoside analogue, inhibits viral DNA polymerase, independent of thymidine kinase activation | CMV Category C | IV only; active against infections resistant to ganciclovir/foscarnet SE: renal proteinuria, renal toxicity, ↑ creatinine |
Amantadine, Rimantadine | Inhibit uncoating of viral DNA within infected host cells (prevents replication) | Influenza A/C, rubella Category C | SE: anticholinergic symptoms, ataxia and photosensitivity |
*TTP: thrombotic thrombocytopenic purpura*HUS: hemolytic uremic syndrome
Table 7-3:
Antiretroviral Drugs
Name | Mechanism of Action | Characteristics |
|---|---|---|
Nucleoside/nucleotide reverse transcriptase inhibitors | ||
Zidovudine (AZT) | Thymidine analog, inhibits HIV reverse transcriptase (RT) | SE: melanonychia, mucocutaneous pigmentation, bone marrow suppression, lipodystrophy Pregnancy category C |
Didanosine (ddI) | Pyrimidine analog, similar to AZT | SE: pancreatitis, optic neuritis, peripheral neuropathy, lactic acidosis; category B |
Abacavir (ABC) | Nucleoside RT inhibitor | SE: hypersensitivity reaction (can be fatal upon rechallenge) Category C |
Tenofovir | Nucleotide analogue, inhibits RT | Peripheral wasting, cushingoid appearance Category B |
Protease inhibitors | ||
Indinavir, Ritonavir, Lopinavir | Block HIV-1 protease enzymes | SE: lipodystrophy (buffalo hump), gynecomastia, periungual pyogenic granulomas, paronychia, hepatotoxicity |
D. Anti-Parasitic Drugs
Table 7-4:
Anti-Parasite Drugs
Name | Mechanism of Action | Comment |
|---|---|---|
Pyrethrin | Natural extract of chrysanthemum; neurotoxic to lice (not ovicidal) | Contraindicated (CI) if allergy to chrysanthemums |
Permethrin | Synthetic pyrethrin; disables nerve cell Na + transport channels in parasites → resulting in paralysis | Pediculicidal and ovicidal 2 strengths: 1% (OTC), 5% (Rx) CI: allergy to chrysanthemums |
Lindane | Chlorinated hydrocarbon; blocks neural transmission by interfering with GABA→ respiratory/muscular paralysis in parasites | Used for scabies, pubic lice, head lice, and body lice SE: ICD, CNS symptoms (ie. seizures) |
Malathion | Organophosphate cholinesterase inhibitor | Flammable; used in scabies, head lice |
Ivermectin | Blocks glutamate-gated chloride channels → paralysis of parasite | Used for strongyloidiasis, onchocerciasis, Norwegian scabies |
Crotamiton | Scabicide; unknown mechanism | SE: contact dermatitis |
Precipitated sulfur (6%) | Unclear mechanism of action | Scabies in pregnant women and infants < 2 years of age |
Thiabendazole, Albendazole | Inhibits fumarate reductase (helminth-specific enzyme) | Used in cutaneous larva migransSE: dizziness, drowsiness, jaundice |
Na + stibogluconate, meglumine antimoniate | Pentavalent antimonial; unclear mechanism | Treatment for leishmaniasis SE: pancreatitis, hepatitis, renal failure, prolong QT interval |
Pentamidine | Inhibits protozoal DNA/RNA/phospholipid/protein synthesis | Used for trypanosomiasis and leishmaniasis |
Diethylcarbamazine (DEC) | Piperazine derivative, unknown mechanism Mazzotti reaction pt with onchocerciasis treated with DEC → fever, hypotension, tachycardia | Used for filariasis, onchocerciasis |
7.2 Immunosuppressant Drugs
A. Topical Immunosuppressants
Topical Glucocorticoids
Topical form: inhibits epidermal mitosis and DNA synthesis, ↓ collagen cross-linking
Vasoconstriction directly proportional to anti-inflammatory potency of agent
SE: atrophy, striae, acneiform eruption, hypertrichosis, hypopigmentation
Tachyphylaxis: efficacy of topical lost over time, and structurally different steroid required
Pregnancy category C
Topical Calcineurin Inhibitors
Includes pimecrolimus (Elidel®) and tacrolimus (Protopic®)
Binds FK506-binding protein, which then inhibits calcineurin (phosphatase) and subsequently blocks T cell activation; calcineurin typically activated by calcium and calmodulin (bound together), which subsequently causes dephosphorylation of nuclear factor of activated T cells (NFAT) and T cell activation
B. Oral Immunosuppressants
Oral Glucocorticoids
Anti-inflammatory, anti-mitotic, immunosuppressive and vasoconstrictive properties; forms complex with intracellular receptors and modulates transcription of certain genes
Effects:
↓ Circulating lymphocytes/eosinophils/monocytes, ↓ macrophage response to lymphokines, ↓ Ab production, ↓ synthesis of proinflammatory molecules, ↓ fibroblast production of collagen
↑ Neutrophils, ↑ blood glucose (stimulates gluconeogenesis), ↑ protein catabolism, ↑ plasma fatty acids/ketone body formation, ↑ acid/pepsin secretion in stomach
Side effects
Cutaneous: atrophy, telangiectasias, striae, poor wound healing
Musculoskeletal: osteoporosis (decrease intestinal calcium absorption, inhibit osteoblasts, increase bone resorption by osteoclasts and increase calcium excretion by kidneys)
Other: ↑ appetite, peptic ulcers, pancreatitis, Cushing’s syndrome, hyperglycemia, hypertriglyceridemia, sodium retention, cataracts, glaucoma, ↑ risk of infection, hypertension, hirsutism, HPA axis suppression, failure to thrive, aseptic necrosis of femoral head (MRI best modality to evaluate), muscle weakness, psychosis, pseudotumor cerebri
Short-acting glucocorticoids → cortisone and hydrocortisone
Greatest mineralocorticoid activity; lowest glucocorticoid activity
Intermediate and long-acting glucocorticoids → methylprednisolone, triamcinolone, dexamethasone, betamethasone
Virtually no mineralocorticoid activity; dexamethasone/betamethasone with highest glucocorticoid activity
Dosing
Single morning dose ↓ risk of HPA suppression
Divided daily dosing may ↑ anti-inflammatory efficacy but also ↑ systemic toxicity
Alternate day dosing reduces all complications except osteoporosis and cataracts
Purine analog which blocks purine synthesis (S phase specific); active metabolite is 6-mercaptopurine (6-MP) which is converted to either inactive or active metabolite (6-thioguanine) via one of three enzymatic pathways (TPMT, HPRT, XO):

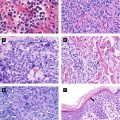
Figure 7.1:
Metabolic pathway for azathioprine
TPMT: thiopurine methyltransferaseHPRT: hypoxanthine phosphoribosyltransferaseXO: xanthine oxidase
If XO or TPMT activity inhibited, HPRT becomes primary pathway causing excess toxic purine analogs, which can cause bone marrow suppression; can occur if azathioprine used with allopurinol (which blocks XO) or in patients with genetically low TPMT levels
Excreted by kidneysCheck TPMT levels before starting medication
SE: bone marrow suppression, hypersensitivity syndrome, teratogenicity, lymphoproliferative malignancies (latter only documented in rheumatoid arthritis)
Pregnancy category D
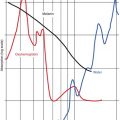
Antimetabolite and antifolate drug; inhibits dihydrofolate reductase (DHFR) involved in folic acid pathway, which is necessary for DNA/RNA synthesis (via purine and thymidylate synthesis); S phase specific
DHF: dihydrofolateTHF: tetrahydrofolate

Figure 7.2:
Metabolic pathway inhibited by methotrexate
Renal excretion; liver biopsy at cumulative dose of 3.5 grams unless high risk; treat acute toxicity with leucovorin; caution in patients with ↑ alcohol intake, diabetes, or renal failure
SE: hepatotoxicity, pancytopenia, teratogenicity (egg and sperm), acute pneumonitis (idiosyncratic), pulmonary fibrosis, ± lymphoma
↑ Pancytopenia risk with concomitant use of: NSAID, dapsone, TMP/SMX, or no folate supplementation; ↑ MTX levels with concomitant use of TCN, phenytoin, phenothiazine, barbiturate, NSAID, salicylate, sulfonamide
Pregnancy category C
Mycophenolate Mofetil (Cellcept)
Inhibits de novo purine synthesis by inhibiting inosine monophosphate dehydrogenase (IMPDH); T and B cells particularly affected; excreted by kidneys
After ingestion, active metabolite is mycophenolic acid; deactivated by liver but ‘reactivated’ by both epidermis and GI tract
SE: nausea, vomiting, reversible dose-related bone marrow toxicity, progressive multifocal leukoencephalopathy, pure red cell aplasia
Caution in peptic ulcer disease; of note, not hepatotoxic or nephrotoxic
Pregnancy category D
Cyclophosphamide (Cytoxan)
Nitrogen mustard derivative; cell cycle DNA cross-linkages at any point in cycle
SE: teratogenicity, ↑ lymphoma, ↑ leukemia, ↑ bladder cancer, ↑ SCC, bone marrow suppression, hemorrhagic cystitis (mesna decreases toxicity), azoospermia, pulmonary fibrosis, alopecia, hyperpigmentation of skin/nails
Treatment of choice for Wegener’s granulomatosis
Pregnancy category D
Apremilast (Otezla)
Selective immunosuppressant: phosphodiesterase-4 (PDE4) inhibitor which causes increased cyclic adenosine monophosphate (cAMP), which in turn activates protein kinase A (PKA) and other downstream effectors, resulting in inhibition of proinflammatory cytokine transcription, neutrophil degranulation, chemotaxis and adhesion to endothelial cells; used for both psoriasis and psoriatic arthritis
SE: nausea, diarrhea, depression, weight loss
Calcineurin: a phosphatase activated in presence of calmodulin and calcium by cyclophilin
Cyclosporine (CsA)
Inhibits T cell activity by binding to cyclophilin, which subsequently blocks cyclophilin’s ability to activate calcineurin; calcineurin regulates NFAT and IL-12, which results in overall inability to produce/release IL-12
Treatment for psoriasis, pyoderma gangrenosum, severe atopic dermatitis, autoimmune bullous disorders
SE: nephrotoxicity, reversible HTN, gingival hyperplasia, hyperlipidemia, ↑ K and ↓ Mg, ↑ uric acid, paresthesias, hypertrichosis, lymphoma
Metabolized by cytochrome p450 3A4: inhibitors of cytochrome cause ↑ CsA levels (ie. diltiazem, nicardipine, verapamil, ketoconazole, fluconazole, itraconazole, erythromycin); inducers of p450 enzymes result in ↓ CsA levels (rifampin, phenobarbital, phenytoin, carbamazepine)
Check BP regularly; if renal creatinine above 30% of baseline, dose should be reduced
↑ Risk for renal toxicity: aminoglycosides, NSAIDs, amphotericin B and vancomycin
Pregnancy category C
Hydroxyurea
Inhibits ribonucleotidase reductase (inhibits DNA synthesis); S-phase specific
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree