BLEPHAROPLASTY
I. ANATOMY
A. General anatomy
1. Levator palpebrae
a. Origin: Lesser wing of sphenoid
b. Insertion: Dermis and superior edge of tarsus
c. Innervation: CN III
d. Action: 10 to 15 mm upper lid excursion
e. Whitnall ligament: Fascial condensation 16 mm from superior edge of tarsus
2. Müller’s muscle
a. Origin: Levator
b. Insertion: Superior edge of tarsus
c. Innervation: Sympathetic nerves
d. Action: 2 to 3 mm upper lid lift
3. Capsulopalpebral fascia (lower levator)
a. Origin: Inferior oblique muscle fascia
b. Insertion: Septum 5 mm below tarsus
c. Action: 1 to 2 mm downward lower lid migration with downward gaze
4. Medial canthal tendon: Formed by deep head of pretarsal orbicularis, medial Lockwood’s ligament, check ligaments of medial rectus, and Whitnall’s ligament
5. Lateral canthal tendon: Formed by Lockwood ligament, lateral horn of levator, check ligament of lateral rectus, and deep preseptal and pretarsal orbicularis
6. Upper tarsus
a. 7 to 11 mm wide
b. Sup border: Site of Müller’s muscle insertion and levator insertion
7. Orbicularis oculi muscle
a. CN III innervation
b. Orbital portion
i. Outermost, superficial to corrugator and procerus
ii. Voluntary eye closure
c. Preseptal: Overlies septum and allows for voluntary and involuntary blink
d. Pretarsal: Adheres to tarsus and involved in involuntary blink
8. Orbital fat
a. Upper lid: Medial and middle compartments separated by trochlea of superior oblique
b. Lower lid: Lateral, central, and medial compartments with central and medial compartments divided by inferior oblique
9. Lacrimal drainage system: Punctum→canaliculus→lacrimal sac→nasolacrimal duct→inferior meatus
______________
*Denotes common in-service examination topics
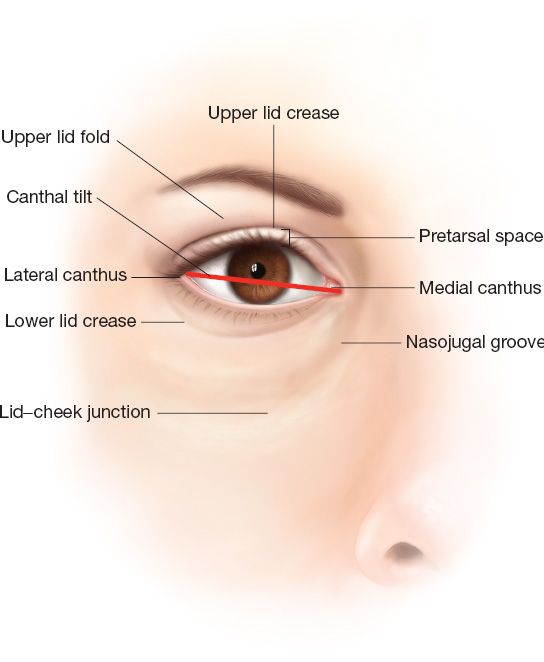
Figure 34-1. Surface anatomy of the eyelids.
B. Surface anatomy (Fig. 34-1)
1. Palpebral fissure: Measures 12 to 14 mm vertically, 28 to 30 mm horizontally
2. The upper lids rest 2 mm below the superior limbus, the lower lid rests at the inferior limbus
3. Anterior hairline to brow distance: Approximately 5 to 6 cm at the midpupillary line
4. Brow to supratarsal crease distance: Approximately 10 to 12 mm
5. Supratarsal crease: Ideally 8 to 10 mm above the upper lid margin
6. *The minimum distance from upper eyelid margin to brow which precludes lagophthalmos is around 20 mm (18 to 24 mm)
7. Lateral canthus position: About the level of the midpupil and 1 to 2 mm superior to medial canthus.
8. In women, the eyebrow should peak above the superior orbital rim margin at the level of the lateral limbus, corresponding to the junction of the middle third with the lateral third of the brow.
9. 2-5mm of pre tarsal lid show.
10. In men, the eyebrow should be more transverse and along the superior orbital rim margin.
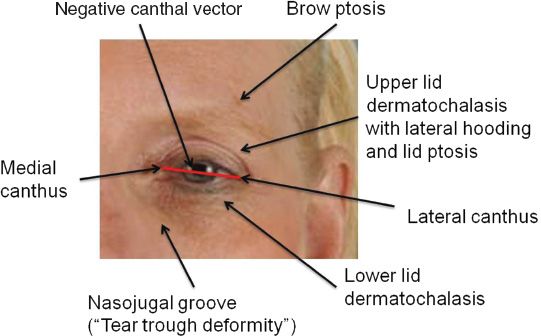
11. Many of these periocular relationships change with facial aging (Fig. 34-2).
Figure 34-2. Features of periocular aging.
C. Layers of the eyelid
1. Anterior lamella
a. Skin (0.5 to 0.7 mm thick), subcutaneous fat
b. Orbicularis oculi muscle (divided into pretarsal and preseptal components)
i. Sphincter muscle innervated by buccal, zygomatic, and frontal branches. Persistent tone during sleep.
a) Peripheral orbital—contracts for tight closure
b) Palpebral—contracts for light closure
c) Lacrimal
ii. OO has direct muscle attachment to inferior orbital rim from anterior lacrimal crest out to level of medial corneoscleral limbus. Lateral to this point, the attachment of the OO to the rim is indirect through the orbicularis retaining ligament (ORL). Pretarsal segment of OO is relatively fixed, while the preseptal segment undergoes elongation with downward displacement of the lid–cheek junction with age.
iii. Above the levator labii superioris, the OO is closely attached to orbital rim. The length of this attachment increases to a maximum centrally 10 to 14 mm (distance from orbital rim to OO) and 1.5 to 5 mm in thickness.
c. ORL—bilaminar membrane derived from reflection of orbital septum on orbital side and from continuation of membrane covering the preperiosteal fat over the zygoma on the caudal side
i. Spans from periosteum just outside orbital rim to fascia on undersurface of OO separating it into preseptal and peripheral parts
ii. Periosteal attachments continue around inferior orbital rim to the lateral canthal region
iii. The length of the ORL diminishes laterally until it becomes negligible at the lateral orbital thickening (LOT). ORL lies directly cephalad and on the orbital side of the zygomaticofacial nerve and foramen.
iv. Laxity of ORL centrally creates a V-shaped deformity that contributes to the development of nasojugal grooves. The descent of the lid–cheek junction produces a redundancy of the prezygomatic space that contributes to the appearance of malar mounds. Lengthening allows descent of bulging orbital fat behind the attenuated septum orbitale.
v. It is the ORL, and not the septum orbitale, that defines the lower limit of descent and shape of lower lid fat bulges
vi. Fat bulges most prone centrally where the ligament is weakest and becomes most distended. Lateral compartment fat bulges are initially situated higher near the lateral canthus because the septum orbitale is least distensible near the inferolateral orbital rim.
vii. Access to ORL may be gained through pre-zygomatic space
2. Middle lamella
a. The orbital septum originates from the arcus marginalis and is contiguous with the orbital periosteum.
b. In upper lid septum fuses with levator several mm above tarsal plate. IN lower lid, the septum fuses with the capsulopalbral fascia below the tarsal plate.
3. Posterior lamella
a. Tarsoligamentous sling.
b. Upper lid: Tarsus, levator, Muller’s muscle and conjunctiva.
c. Lower Lid: Tarsus, capsulopalpebral fascia and conjunctiva.
4. Fat
a. Preseptal fat: sub-orbicularis oculi fat (SOOF in lower lid), retro-orbicularis oculus fat (ROOF in upper lid)
b. Postseptal fat: Intraorbital fat pads
c. The upper lid has central and nasal fat pads, separated by the superior oblique tendon. Laterally, the lacrimal gland takes the space of what would be the lateral fat pad.
d. The lower lid has lateral, central, and nasal fat pads. *The nasal and central pads are separated by the inferior oblique tendon, which is the most commonly injured structure in a blepharoplasty.
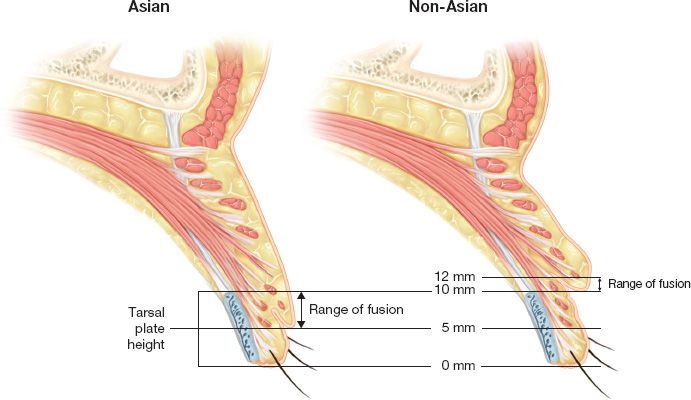
D. The Asian eyelid (Fig. 34-3)
1. The Asian eyelid differs from the Caucasian eyelid in the lack of the supratarsal fold, a narrower palpebral aperture, and a slightly higher lateral canthus
Figure 34-3. Asian versus non-Asian upper lid anatomy.
2. The lack of supratarsal fold is due to the absence of fibrous extensions of the levator piercing the orbital septum and attaching to the orbicularis and skin
3. Various Asian blepharoplasty techniques exist to surgically create a tarsal fold by making an attachment between the levator aponeurosis, dermis, and tarsal plate
II. INDICATIONS AND PATIENT ASSESSMENT
A. The goal of blepharoplasty is to recreate a more youthful periocular appearance by creating a well-defined tarsal fold with pretarsal show on the upper lid and a smooth lid-cheek junction in the lower lid
B. Particular attention is paid to a history of smoking, diabetes, myasthenia gravis, Graves disease, bleeding disorders, abnormal scarring, dry eyes (xerophthalmia), allergies, glaucoma, cataracts, and visual impairment
C. Ask “Can you wear contacts?”, “How long can you keep your eye open before needing to blink?”, “Do you use eye drops routinely?” Intolerance of contact lenses may be an important indicator of dry eyes.
D. Aesthetic measurements
1. Palpebral fissure: 12 to 14 mm vertically, 28 to 30 mm horizontally
2. Upper lid: At level of upper limbus with highest point just medial to pupil
3. Lower lid: At lower limbus with lowest point slightly lateral
4. Visible pretarsal skin: 3 to 6 mm
5. Lash line to supratarsal crease: 8 to 10 mm
6. Anterior hairline to brow: 5 to 6 mm
7. Brow to orbital rim: 10 mm
8. Brow to midpupil: 25 mm
9. Lateral canthus: 1 to 2 mm superior to medial canthus
E. Specific examinations to document prior to blepharoplasty
1. Schirmer’s test
a. Quantitative assessment of tear production, used to judge the postoperative protection of the eye.
b. It consists of placing a piece of filter paper in the inferior fornix and measuring the length of wetting of the paper over 5 minutes.
c. Normal tear production is >15 mm
2. Evaluate the relationship between the cornea and infra-orbital rim. *A negative vector (cornea anteriorly positioned relative to the rim) is prone to lid malposition after blepharoplasty and requires a canthopexy at time of lower lid rejuvenation.
3. Look for tear trough deformity—the concavity at the border of the eyelid and the cheek medially—which is created by protrusion of orbital fat juxtaposed to the tight attachment of the orbital spetum via the arcus marginalis. The tear trough is alternatively called the nasojugal groove and can be addressed with arcus marginalis release, fat repositioning, and septal reset, with fat grafting, or with use of fillers.
4. Examine for lid symmetry, lid ptosis, degree of dermatochalasis, prominence of fat pads, sclera show, lower lid tone (snap test)
5. Presence of edema and pigmentation, which may be indicators of increased risk of excessive postoperative swelling.
6. Examine the brow position. The brow should be manually elevated to determine the effect of brow ptosis on the eyes.
7. Documentation of Bell’s phenomenon: Upward rolling of the globe with eye closing, which serves to protect the cornea in the event of lagophthalmos
8. Visual acuity, field cuts, facial nerves, extraocular movements, and fundoscopic examination
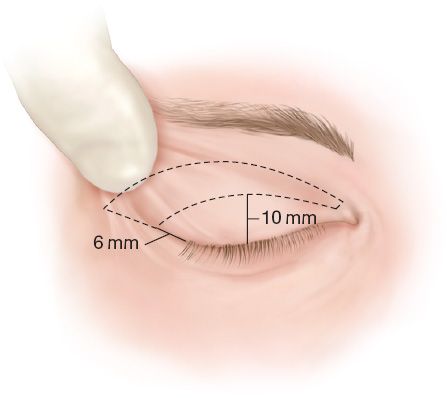
Figure 34-4. Upper lid blepharoplasty markings.
III. OPERATIONS/APPROACHES
A. Upper lid blepharoplasty (Fig. 34-4)
1. Preoperative markings
a. Made prior to injection of local anesthetic with the patient awake
b. The lower incision is usually made anywhere from 6 to 10 mm above the ciliary margin at the level of the superior edge of the tarsal plate. Usually this is at the existing supratarsal crease.
c. The level of the upper incision is determined by gathering the excess lid skin with broad-tipped forceps until lagophthalmos occurs
d. Can also calculate by measuring distance from upper lid to brow and making ellipse big enough that when you subtract this distance from the brow to lid distance, you get between 20 and 24 mm left.
2. The minimal distance from the brow to the upper incision line is usually 10 to 12 mm.
3. The medial and lateral ends of the incisions can be altered with Z-plasties, W-plasties, or Y–V plasties
4. A thin strip of orbicularis oculi muscle excision is variably recommended.
5. Gently depress the globe to aid in the identification of postseptal fat. The septum is incised high to avoid injury to the levator mechanism.
6. *Judicious fat removal is essential, as overresection leads to a “hollowed-out” or cadaveric look
7. The superior oblique muscle may be identified between the nasal and central fat pads and should be protected
8. The dermis and orbicularis may be sutured to the levator in order to recreate a distinct supratarsal fold.
9. Lateral hooding and ptosis may be corrected by a concomitant browlift. In these cases, the browlift should be performed first to allow accurate judgment of how much upper eyelid skin to remove.
10. Lateral fullness may be addressed with suspension of the lacrimal gland
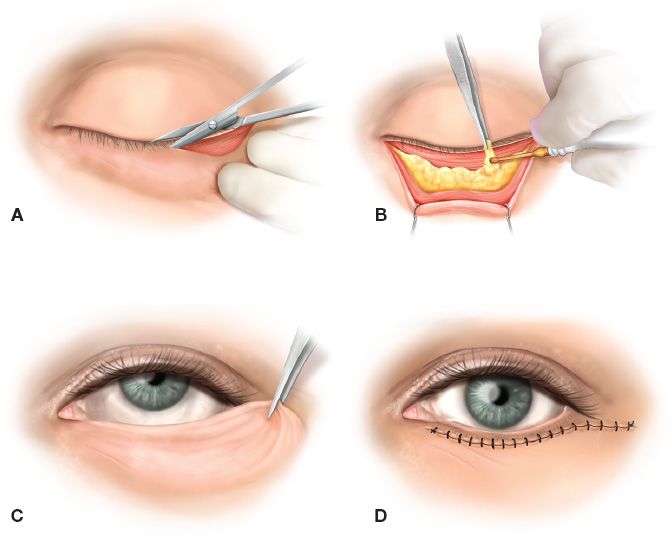
Figure 34-5. Transcutaneous lower lid blepharoplasty. A: Lower lid incision placed in the infraciliary groove. B: Excision of fat, after orbital septum and fat capsule have been incised. C: Determination of the amount of excess skin and muscle for excision by draping skin in a superior and lateral direction while the patient is looking up with the mouth open. D: Closure with running infraciliary 6-0 Prolene suture.
B. Lower lid blepharoplasty
1. Transcutaneous (Fig. 34-5)
a. A conservative, skin-only resection via a subciliary incision may be coupled with retro-orbital (postseptal) fat resection. This is recommended for patients with excess skin and good orbicularis tone.
b. Skin and muscle may be resected together via a subciliary incision if poor orbicularis tone is present. Postseptal fat is excised similarly to upper lid blepharoplasty, with care not to injure the inferior oblique muscle.
c. After the orbital septum is incised along the arcus marginalis to access orbital fat, it may be redraped to a more anterior and inferior position in an effort to diminish a prominent tear trough.
d. A strip of orbicularis may be repositioned laterally and superiorly to support the lateral canthus.
2. Transconjunctival approach:
a. The orbital septum is left intact and fat is removed via an incision through the conjunctiva.
b. This technique can be combined with a separate skin excision or with a chemical or TCA peel.
c. Disadvantages include a more limited exposure and the potential for inadequate fat removal.
C. Ancillary procedures for lower lid laxity
1. Suspension or tightening of the lower lid orbicularis muscle
2. Tarsal suspension with a lateral tarsal strip
3. Lateral canthopexy (to periosteum or drill hole through bone)
4. Temporary external support of the lower lid margin with tape or a tarsorraphy
5. Wedge resection to shorten the lid (Kuhnt–Szymanowski procedure)
IV. POST-OP CARE
A. Chilled gel compress or iced gauze × 48 hours
B. Saline eye drops while awake
C. Lubricating ointment for night use
D. Head elevation to reduce edema and ophthalmic pressure
E. Evaluate and document vision before discharge and 4 to 5 days post-op when sutures removed
F. Lagophthalmos usually secondary to periorbital edema and resolves 1 to 2 weeks
G. Pre- and post-op patient education on eye drop and ointment use is essential to prevent corneal abrasions and exposure problems
V. COMPLICATIONS OF BLEPHAROPLASTY
A. Blindness: Rare—0.0045%, primarily from retrobulbar hematoma (0.05%)
1. A surgical emergency requiring immediate decompression with a lateral canthotomy and cantholysis. *Associated with SEVERE UNILATERAL PAIN.
2. Mannitol and/or acetazolimide administration
3. Emergent ophthalmologic consultation
B. Dry eyes are common postoperatively and are managed with use of artificial tears. Patients with dry eyes preoperatively may have exacerbated symptoms after surgery.
C. Ectropion: Some surgeons recommend a canthopexy in almost every case.
D. Entropion: Significantly less common than ectropion; when occurring after blepharoplasty is usually due to cicatrix of the posterior lamellae.
E. Scarring at the lateral canthus can cause a rounding out of the normal almond shape
F. Corneal injury: Some recommend routine use of corneal shields, but meticulous attention is still necessary to prevent this
G. Ptosis: Usually from damage to levator mechanism. In many cases, ptosis is present preoperatively but not noticed
H. Diplopia: Usually from injury to the inferior oblique or superior oblique muscle
I. Enophthalmos: From excess fat removal
J. Lagophthalmos: A minute amount of lagophthalmos is expected at the end of the case, and most resolves with scar massage and time, but in severe cases of skin overresection may require skin grafting
K. Infection: Rare but may constitute an emergency if develops into orbital cellulitis
L. Lash atrophy
M. Epiphora: Can result from dry eye, exposure, or dysfunction of the lacrimal pump, but is usually a transient problem
BROWLIFT
I. ANATOMY
A. Scalp
1. S—skin
2. C—subcutaneous tissue
3. A—aponeurotica galea, in the forehead it is the frontalis
4. L—loose connective tissue
5. P—pericranium
B. Frontalis
1. Elevates the medial two-thirds of brow and causes transverse rhytides of the forehead skin
2. No bony origins. It traverses subcutaneously from the eyebrows and the root of the nose and is invested by the galea aponeurotica.
3. Innervation: Frontal branch of facial nerve
C. Galea aponeurotica spans from the frontalis muscle anteriorly to the occipitalis muscle posteriorly
D. Corrugator supercilii muscle
1. Triangular muscle located at the medial aspect of the eyebrow deep to the frontalis and orbicularis oculi muscles
2. It causes vertical creases called “glabellar frown lines”
3. Brow depressor
4. Innervation: Frontal and zygomatic branches of CN VII
E. Procerus muscle
1. Originates from the nasal bones and inserts superiorly into the skin between the eyebrows.
2. Causing transverse creases at the radix
3. Brow depressor
4. Innervation: Frontal and zygomatic branches of CN VII
F. The temporal fusion line is a plane of fusion between the galea, temporalis, and the periosteum at the temporal crest.
G. The temporal (frontal) branch of the facial nerve runs on the undersurface of the superficial temporal fascia along a course 0.5 cm below the tragus to a point 1.5 cm above the lateral brow
H. Sensation
1. Supraorbital nerve: Enters corrugator and frontalis supplying forehead: 1.7 to 2.2 cm from midline.
2. Supraorbital
a. Exits foramen/notch lateral to supratrochlear nerve
b. Splits into superficial and deep branches
c. Superficial branch: Enters frontalis 2 to 3 cm above rim supplying forehead
d. Deep branch: Supplies scalp posterior to hairline and is divided during coronal incision causing scalp paresthesias.
I. Physiology
1. Frontalis: Elevates eyebrow causing transverse wrinkling of forehead
2. Corrugator supercilii: Draws eyebrows inferomedially causing vertical furrows
3. Procerus: Pulls glabella caudally resulting in transverse creases at the root of the nose
II. PATIENT ASSESSMENT
A. Measure the height of the forehead (see periorbital rejuvenation)
B. Note the presence of glabellar, forehead rhytides, and brow position in relation to the orbital rim.
C. Distinguish upper lid ptosis from brow ptosis by manually elevating the patient’s lateral brow, noting the true degree of dermatochalasis with the brow held at the appropriate level (depends on gender: men at the orbital rim, women about 1 cm above orbital rim).
A. Botulinum toxin
1. Used to attenuate glabellar grown lines
2. Injected into corrugator supercilii at point medial to end of eyebrow and above the supraorbital rim.
3. Onset of paralysis may take 24 to 48 hours and its effects persist for 4 to 6 months.
B. Suprabrow excision
1. Direct resection of forehead skin above the eyebrow.
2. Can be performed under local anesthesia so considered a good option for older patients with more medical problems.
3. Relies on skin tension to reposition brow, which can lead to scar spreading and early relapse and therefore has been replaced by other techniques.
C. Transpalpebral corrugator resection
1. Indicated in patients who exhibit significant glabellar frown lines and corrugator hyperactivity, but minimal brow ptosis and do not want continued botulinum toxin injection.
2. Used as adjunct to blepharoplasty or alone in patients who do not need or desire full forehead rejuvenation.
3. The procerus and corrugator supercilii are resected with care to preserve the supraorbital and supratrochlear nerve fibers. A fat graft can be placed to fill in the resultant depression.
D. Endoscopic brow lift
1. *Most useful in patients with an optimal forehead height of <6 cm.
2. Preoperative markings consist of placing reference marks on the eyebrows directly above the medial canthus, midpupil, and lateral canthus, as well as the anterior hairline directly above the medial canthus and midpupil.
3. If brow to hairline is >6 cm, and you perform endobrow, you will get an overly long forehead and endotines will be hard to put in behind the hairline.
4. Brow height from the midpupil should be approximately 22 to 25 mm.
5. Tissue fixation techniques (endotine, anchors, K-wires) are required
6. Technique
a. Mark out course of temporal branch of facial nerve: triangle from line 0.5 cm below tragus to 2 cm above lateral eyebrow. Draw second line along zygoma to lateral orbital rim and then connect these lines.
b. Mark out course of supraorbital and supratrochlear nerves 1.7 to 2.2 cm lateral to midline or at supraorbital notch (or midpupillary line).
c. Mark out area where you will resect procerus (radix of nose)
d. Mark where you will resect corrugator (just medial to medial brow angle slightly inferior).
e. Mark area of brow directly above medial canthus, midpupil, and lateral canthus and lateral brow along line from ala
f. Port placement
i. Medial port at midpupil line 1.5 cm long, 1 cm behind the hairline (vertical).
ii. Lateral port mark axis of ala to lateral canthus 2 cm behind the hairline and make this 3 cm long (horizontal).
iii. Central port optional
g. Inject lido with epi in subperiosteum all the way along forehead and the entire scalp.
h. Place two medial ports at midpupil line 1.5 cm long and 1 cm posterior to hairline as previously marked.
i. Once get down to subperiosteal level, mark inferior part of incision on bone so you know where you started.
j. Once you are done with entire subperiosteal dissection, you can put in scope and then get down over orbital rim and identify supraorbital nerves and corrugator.
k. Make incision for lateral ports: as above 2 cm behind hairline, 3 cm long in line with a line from ala to lateral canthus.
l. Cut through temporoparietal fascia (superficial temporal fascia) to deep layer or deep temporal fascia but not through the deep temporal fascia.
m. Dissect in the plane superficial to the deep layer of the deep temporal (temporalis muscle is below the deep layer of deep temporal fascia). The surgeon can verify the identity of the deep layer of the deep temporal fascia by making one small incision through this fascia and observing the temporal muscle in the next deeper plane.
n. Also make registry in fascia so you know where you started.
o. Dissect above deep layer of DTF toward Zygoma and stop 2 cm short of lateral orbital rim and you will feel superficial temporal crest fusion line.
p. In this lateral dissection, extend down to orbital rim junction where temporal vein is divided and then inferiorly down to level of lateral canthus.
q. Dissection stops 1 cm above zygomatic arch where second temporal vein is encountered.
r. Insert scope into medial port and use #2 elevator performing subperiosteal dissection to the radix midline and laterally to lateral canthus.
s. Make sure to lift this over the supraorbital rim.
t. Protect the supraorbtial and supratrochlear nerves.
u. Cut the periosteum above the supraorbital rim using a reverse elevator and release to radix and make sure to define your nerves.
v. Use grasper and ablate both corrugator and procerus.
w. Slide elevator into lateral port and move it medial to fusion line and then place an endoscope so you can see temporal connection between temporoparietal fascia and periosteum and take down fascial bands. You take down the insertion and should be able to see temporal muscle on one side and periosteum on other.
x. Come across fusion line from lateral to medial and superior to inferior.
y. Place TLS drain for temporal incision.
z. Use endotine drill and drill a point in medial/post part of the medial incision.
a1. Pull scalp posteriorly and engage scalp into endotine.
b1. Check symmetry with eyebrows slightly above supraorbital rim
c1. Take large bite of superficial temporal fascia of the superior flap of the lateral port. Temporal fascia is lifted posteriorly and superiorly and secured to deep temporal fascia with 3-0 PDS. You should be pulling back about 13 mm.
d1. Skin closed with 4-0 prolene or staples
E. Open brow lift: An open browlift is indicated if the patient has a superiorly displaced (high) frontal hairline (>6 cm in men, >5 cm in women.) Several incisions are available
1. Coronal: Removes tissue from behind the hairline, but lengthens the forehead. Therefore, the coronal incision is indicated in patients with a short forehead.
2. Pretrichial: Incision is placed at the hairline. *This incision shortens the forehead and is indicated in patients with a long forehead.
3. Midforehead: Excises a strip of skin and subcutaneous tissue from middle of forehead, placing incision along a transverse rhytid. Useful in men with thick skin and alopecia, where the scar will be less obvious here than on scalp. A variation of this is an incision just above each brow.
A. Injury to supraorbital or supratrochlear nerves. *Posterior scalp dysesthesias can result from injury to the deep branch of the supraorbital nerve.
B. Alopecia can result from use of electrocautery or excessive tension at the incision.
C. Injury to the temporal branch of facial nerve during temporal dissection
D. Contour irregularity from overresection of muscle (e.g., corrugators)
E. Asymmetry of brow posture
F. Permanent overcorrection, for example, “surprised look”
PEARLS
1. Leave at least 10 mm between the lateral extent of the upper and lower blepharoplasty incisions.
2. Rule out medical reasons for patients who “look tired” (e.g., myasthenia gravis)
3. Avoid overcorrection! Restore brow position and shape. A low brow can be aesthetically pleasing and brows that look lifted are not aesthetic.
4. Be prepared at all times to draw the cross-section anatomy of the upper and lower eyelids
QUESTIONS YOU WILL BE ASKED
1. To what does a negative vector predispose the patient?
Lower lid malposition.
2. Why do not we take out all this fat around the eye?
It will result in a “hollowed out” or “cadaveric” look. Judicious fat removal is key.
3. What is a normal Schirmer’s test?
Five minutes after placing a piece of filter paper in the inferior fornix there should be ~15 mm of tears.
4. What are the ROOF and the SOOF?
The ROOF stands for retro-orbicularis oculus fat and is the preseptal fat in the upper lid. The SOOF stands for sub-orbicularis oculi fat and is the preseptal far in lower lid.
5. What is the minimal distance you need to leave between the eyebrow and the upper lid incision.
10 to 12 mm. Not leaving enough skin can result in lagophthalmos and potentially corneal exposure.
6. How many fat compartments are in the upper and lower eyelids, respectively?
The upper has two compartments: central and nasal; the lower has three compartments: nasal, central, and lateral.
7. What structure separates the nasal and central fat compartments?
The inferior oblique tendon.
8. When would a pretrichial incision be a good choice for a brow lift?
In a patient with a long forehead, because this incision shortens the forehead.
Recommended Readings
Blepharoplasty
Carraway JH. Surgical anatomy of the eyelids. Clin Plast Surg. 1987;14(4):693–701. PMID: 3308277.
Chen WP. Asian blepharoplasty. Update on anatomy and techniques. Ophthal Plast Reconstr Surg. 1987;3(3):135–140. PMID: 3154592.
Jelks GW, Jelks EB. Preoperative evaluation of the blepharoplasty patient. Bypassing the pitfalls. Clin Plast Surg. 1993;20(2):213–223; discussion 224. PMID: 8485931.
May JW Jr, Fearon J, Zingarelli P. Retro-orbicularis oculus fat (ROOF) resection in aesthetic blepharoplasty: a 6-year study in 63 patients. Plast Reconstr Surg. 1990;86(4):682–689. PMID: 2217582.
Rohrich RJ, Coberly DM, Fagien S, Stuzin JM. Current concepts in aesthetic upper blepharoplasty. Plast Reconstr Surg. 2004;113(3):32e–42e. PMID: 15536308.
Tomlinson FB, Hovey LM. Transconjunctival lower lid blepharoplasty for removal of fat. Plast Reconstr Surg. 1975;56(3):314–318. PMID: 1153547.
Brow Lift
Ellenbogen R. Transcoronal eyebrow lift with concomitant upper blepharoplasty. Plast Reconstr Surg. 1983;71(4):490–499. PMID: 6828583.
Knize DM. Limited-incision forehead lift for eyebrow elevation to enhance upper blepharoplasty. Plast Reconstr Surg. 1996;97(7):1334–1342. PMID: 8643715.
Moss CJ, Mendelson BC, Taylor GI. Surgical anatomy of the ligamentous attachments in the temple and periorbital regions. Plast Reconstr Surg. 2000;105(4):1475–1490; discussion 1491–1498. PMID: 10744245.
Ramirez OM. Endoscopically assisted biplanar forehead lift. Plast Reconstr Surg. 1995;96(2):323–333. PMID: 7624404.
< div class='tao-gold-member'>