8.6 Periareolar technique with mesh support
Synopsis
 The chapter describes a technique based on reshaping the breast parenchyma and treating the glandular mound separately from the skin.
The chapter describes a technique based on reshaping the breast parenchyma and treating the glandular mound separately from the skin.
 The skin is redraped over the new breast architecture, though the periareolar approach, and the new breast is assembled through glandular flap rotation and fixation to the anterior pectoral fascia.
The skin is redraped over the new breast architecture, though the periareolar approach, and the new breast is assembled through glandular flap rotation and fixation to the anterior pectoral fascia.
 The cutaneous lining is duplicated using a circular dermal flap with the central pedicle in the areolar region.
The cutaneous lining is duplicated using a circular dermal flap with the central pedicle in the areolar region.
 The addition of the mixed mesh to the original technique, applied as a sandwich between the two layers of cutaneous lining, was performed to obtain a longer-lasting aesthetic result based on a resistant supporting system.
The addition of the mixed mesh to the original technique, applied as a sandwich between the two layers of cutaneous lining, was performed to obtain a longer-lasting aesthetic result based on a resistant supporting system.
 This would maintain the ideal position of the gland after surgery and permit adequate fixation of the tissues into place.
This would maintain the ideal position of the gland after surgery and permit adequate fixation of the tissues into place.
Evolution of the technique
The areolar surgical approach has always been of great interest to the authors, as it enables surgical access to the whole breast; the glandular mound can be treated separately from the skin coverage, and the surgery results in minimal scars, avoiding the unpleasant ‘surgical’ appearance. In 1976, the authors described the areolar mammary quadrant resection, with plastic repair using two internally rotated glandular flaps detached from the skin.1
This technique, which is currently used in oncological quadrantectomies, was the basis for the development of Góes’ periareolar technique, first published in 1989.2–9 Periareolar mammoplasty was initially intended to reposition the glandular mound and provide a new positioning in relation to the thorax and a new aesthetic format.10–16 The skin cover, initially detached from the gland, only covers the repositioned gland, leaving one scar in the periareolar region. Excessive periareolar skin is de-epithelialized and used as an internal flap, working as an internal bra to support the new breast.
Different kinds of materials have been used for the support system. A polyglactin 910 mesh was initially used in 55 cases. Because it is an absorbable material, there was a partial loss of the aesthetic result after 2 years of follow-up.4,5
To obtain a long-lasting result, a mixed-mesh of polyglactin 910 and polyester was used in 172 cases, providing excellent results which were maintained in the late follow-up for several years. Other partially absorbable materials were also used and with delicate permanent components, which we consider important to maintain the ideal format of the breast, such as Vypro made of polypropylene and polyglactin and presently, we are using ULTRAPRO made of polypropylene and monocryl.6,7
Marking
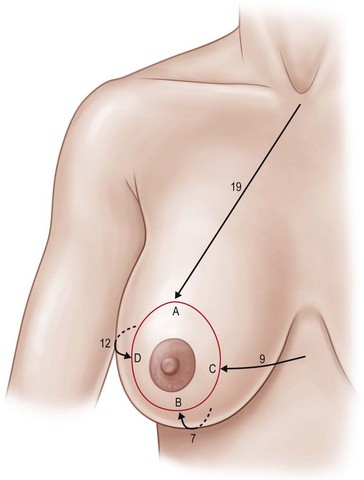
Preoperative planning and marking must be carefully performed so that the correct amount of skin is present to cover the reassembled gland without tension (Fig. 8.6.1). Insufficient skin at any point tends to pull the areola, leading to loss of anterior projection and compromising the final result.
Surgical technique
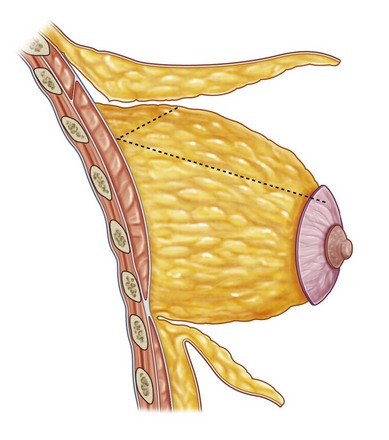
The region between the areola and the teardrop markings is de-epithelialized. Dissection of the upper skin flap is beveled, so that the thickness of adipose tissue attached to the skin increases progressively. This maneuver enhances the upper pole fullness since the thickened flap overlaps the newly assembled gland at the end of the operation. The first 4–5 cm are dissected, leaving a 0.5 cm layer of subcutaneous adipose tissue attached to the dermis, which preserves the subdermal vascular plexus responsible for flap viability. From then on, flap thickness increases until the anterior pectoral fascia appears. Dissection continues superiorly for approximately 4 cm or until the ideal position of the future upper breast pole is reached (Fig. 8.6.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree