CHAPTER 51 Periareolar Benelli mastopexy and reduction: The “Round Block”
History
However, the indications for the various periareolar plasty techniques have been limited.1–6 Only moderate cases of small breast ptosis have been treated using periareolar mastopexy, owing to the risk of enlargement and distortion caused by tension on the areola. The round block technique helps to eliminate this complication, and makes it possible to treat many cases of breast ptosis and hypertrophy by periareolar mastopexy.7,8
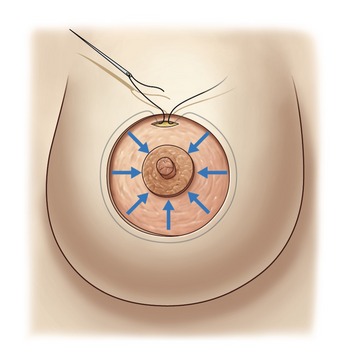
One of the principal elements of our technique is to treat ptosis and hypertrophy by using a blocked circular dermal suture passed in a purse-string fashion. The round block constitutes a cerclage, fixing a solid circular dermodermal scar block around the areola (Figs 51.1 and 51.2).
Evolution of personal technique
In 1983, we started performing periareolar mastopexy with dermal cerclage of the areola via a purse-string suture in order to prevent postoperative enlargement of the areola and the scar. In view of this procedure’s effectiveness, we extended its application, calling it the “round block” because of the solidity of the dermodermal circular scar block reinforced by the cerclage, with a non-resorbable suture passed in a purse-string manner through the edge of the periareolar dermis. By using the round block, our efforts initially enabled reduction of the length of the horizontal scar, and subsequently, to totally eliminate the horizontal scar, going from a T-inverted technique to a vertical technique.7,8 Finally, it was possible to eliminate the vertical scar with the periareolar technique.
This procedure has enabled us to treat more serious cases of ptosis and thereby extend the indications of periareolar mastopexy that in the past had been reserved only for moderate ptosis or hypertrophy, essentially because of the postoperative risk of enlargement of the areola and periareolar scar.
The inverted-T techniques that give maximum coning and the best long-term hold are those that are characterized by crossing and overlapping of two flaps (lateral and medial), which ensure a maximum of anterior projection to the areola.9,10
Materials and methods
From 1983 to December 2007, we performed this surgical procedure on over 528 patients in aesthetic, tumoral, and reconstructive surgeries (Table 51.1). We have been progressive in our advancement of this procedure for cases of serious ptosis or hypertrophy. Breast reductions have entailed an average resection of 180 g (maximum 1200 g) on each breast.
Table 51.1 Clinical series (January 1983 to December 2007)
| Breast reductions | 43% | 227 |
| Mastopexies | 22% | 116 |
| Mastopexies and augmentations | 23% | 122 |
| Tumoral and reconstructive surgeries | 12% | 63 |
| Total number of cases | 100% | 528 |
Anatomy
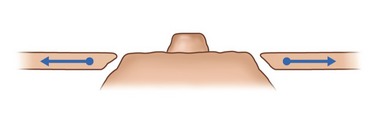
For support of the breast, the periareolar technique is used to remove the thin, elastic stretched skin around the areola, which does not have any supportive value, and to conserve the thick skin at the base of the breast and submammary fold.
Subdermal vascularization is preserved with skin excision done with scissors close to the gland. At the time of the dermal incision within the de-epithelialized ellipse, we conserve a 1 cm strip of dermis in order to protect the vascularity of the ellipse’s skin edge, especially in its lower part (see Fig. 51.5).
Physical evaluation
Technical steps
Step 1: Planning and marking
Marking in the standing position
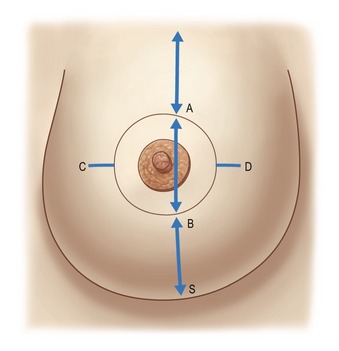
The midline is marked to maintain symmetry. The breast meridian is marked at the beginning on the clavicle, 6 cm from the midline. The meridian is not the meridian of the ptotic breast, but the meridian of the manually reshaped breast. This new meridian will not necessarily cross the ptotic nipple, because the mammary ptosis is generally a lateralization of the breast due to chest wall convexity (Fig. 51.3).
The new areola vertical position
The superior border of the areola (point A) is marked as in a Pitanguy technique on the breast meridian, 2 cm higher than the anterior projection of the submammary crease. Reshaping the breast manually, the surgeon verifies that point A is marked in the correct position. Contralateral point A is marked by measuring the distance to the sternal notch.