I. HISTORICAL PERSPECTIVE
A. Perforator flap era began in 1989—Koshima and Soeda described an inferior epigastric artery skin flap without the rectus abdominis muscle for reconstruction of floor-of-mouth and groin defects.
II. WHAT IS A “PERFORATOR”?
A. In Latin, per means “through” and forare means “to pierce or bore”.
B. Describes a blood vessel that branches off a major named vessel (or source vessel), supplying a particular tissue territory, or angiosome.
C. *Mathes and Nahai tripartite system of fasciocutaneous flaps: Based on three major types of perforators (see Chapter 4—Fig. 4-4)
1. Type A (direct cutaneous vessel)
2. Type B (septocutaneous vessel)
3. Type C (musculocutaneous vessel)
D. “Direct” versus “indirect” perforators
1. Direct perforators course from the source vessel to the skin without first supplying any other deep structure. Examples: An axial vessel, a direct cutaneous vessel (Mathes and Nahai Type A), or a septocutaneous vessel (Mathes and Nahai Type B).
2. Indirect perforators first pass through an intermediary structure before ultimately reaching the subdermal plexus. Example: A muscle or musculocutaneous perforator (Mathes and Nahai Type C), in which the source vessel to the skin passes through and arises from the underlying muscle.
E. Branching patterns of musculocutaneous perforators
1. Type 1 perforators pass almost directly from deep fascia to subdermal plexus without branching.
2. Type 2 perforators branch in the adipose tissue just before reaching the subdermal plexus, with branches then running parallel to the flap surface (e.g., lateral femoral circumflex artery (LCFA)-tfl, tensor fascia lata, deep inferior epigastric artery (DIEP)).
3. Type 3 perforators follow deep fascia for an indeterminate distance before eventually proceeding into subcutaneous tissues (e.g., LCFA-vastus lateralis or ALT flap).
III. WHAT IS A “PERFORATOR FLAP”?
A. A perforator flap generally refers to tissue that receives its blood supply via a “perforator”.
B. Not always a cutaneous flap—can eliminate the cutaneous component to create an adiposal or adipofascial flap.
C. Terminology is historically controversial, with multiple terms used.
D. Some surgeons believe that the muscle perforator flap is the only “true” perforator flap because of the additional time and effort required to dissect the perforator out from between muscle fibers, and intramuscular dissections are technically more difficult.
______________
*Denotes common in-service examination topics
IV. CURRENT STANDARDIZED NOMENCLATURE
A. Perforator flaps are described according to the main artery of origin (e.g., LCFAP for lateral circumflex femoral artery perforator).
B. Suffix “AP” (Artery Perforator) signifies a true musculocutaneous perforator flap.
C. Suffix “-s” is added if the flap is harvested based on direct septal or fasciocutaneous vessels.
D. When multiple flaps are based on musculocutaneous perforators from the same source artery, the muscular origin of the vessel is abbreviated and italicized to indicate the anatomical origin of the flap (e.g., LCFAP-vl for vastus lateralis [VL]).
E. When flaps are based on source arteries that have numbered segmental origins, such as the posterior intercostal arteries, the corresponding vessel number is added after the flap abbreviation (e.g., PIAP-8 for eighth posterior intercostal artery perforator flap).
F. Examples (common name → current nomenclature)
1. Deep inferior epigastric perforator flap → DIEP flap
2. Thoracodorsal artery perforator → TAP
3. Anteriolateral thigh flap → ALT flap
4. Superior gluteal artery perforator flap → SGAP flap
V. *PROPOSED ADVANTAGES OF PERFORATOR FLAPS
A. Reduced donor site morbidity.
B. Reduced postoperative pain.
C. Faster recovery, shorter hospital stay.
D. Less difficult to tailor or thin the flap for covering or filling defects.
E. Longer pedicle than with the parent musculocutaneous flap.
VI. TECHNICAL POINTS
A. Can increase length of pedicle by dissecting perforator back to its origin.
B. Should deliberately preserve a subcutaneous or other large perforator vein during the harvest for supercharging venous outflow in case there is venous congestion.
C. The need for preoperative studies is dependent on the surgeon. Can identify perforators preoperatively by color duplex ultrasound, computerized tomography (CT) angiogram, or handheld audible Doppler.
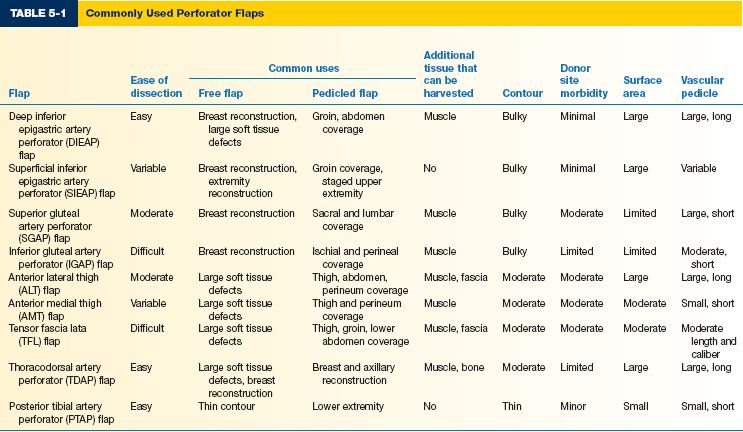
VII. WORKHORSE PERFORATOR FLAPS (TABLE 5-1)
A. Deep inferior epigastric artery perforator (DIEAP) flap—known more commonly as DIEP flap.
1. Indications: Primarily breast reconstruction
2. Anatomy
a. Pedicle length 7.5 to 20.5 cm, diameter 3.3 ± 0.4 mm.
b. Deep inferior epigastric artery (DIEA).
i. Typically divides into two main branches
a) Lateral branch gives rise to lateral row of perforators
1) Usually dominant over medial branch.
2) Has shorter intramuscular course.
3) Gives off more perforators.
b) Medial branch gives rise to medial row of perforators and an umbilical branch.
1) Usually 5 ± 2 perforators can be found concentrated in periumbilical region, which is necessary if zone IV is used.
ii. Usually accompanied by two venae comitantes.
c. Superficial inferior epigastric venous system
i. Responsible for most of the flap’s venous drainage.
ii. Superficial inferior epigastric vein (SIEV) is larger than the deep inferior epigastric vein (DIEV).
3. Surgical technique
a. Flap harvesting
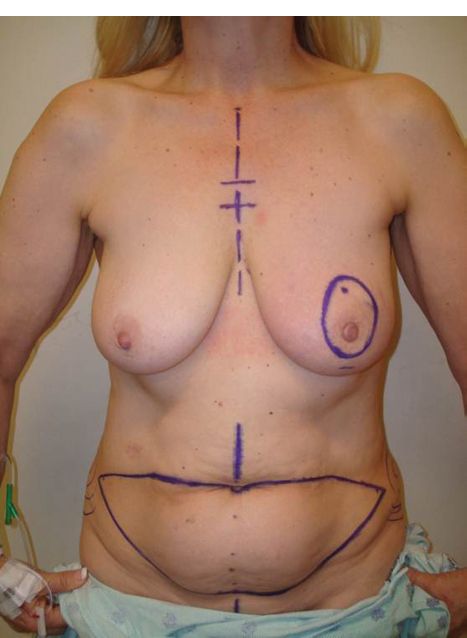
i. Use standard abdominoplasty markings (Fig. 5-1), extending laterally to anterior superior iliac spines (ASIS).
Figure 5-1. Standard markings for the transverse rectus abdominis musculocutaneous flap or DIEP flap markings at our institution.
ii. Search for superficial inferior epigastric artery (SIEA) and SIEV first
a) If SIEA is of sufficient caliber, dissection is carried down to origin at common femoral artery (CFA) to harvest the SIEA flap.
1) Decreased donor site morbidity.
2) Only zones I and II are reliably perfused.
b) If only SIEV is present, this can be used as a backup for additional venous drainage if congestion occurs after DIEV anastomosis.
iii. Can raise the flap on more than one perforator from the same perforator row by performing atraumatic longitudinal separation of rectus muscle fibers.
iv. Take care to preserve segmental intercostal nerves, which run medially and superficially to the pedicle.
b. Recipient vessels in breast reconstruction
i. Can harvest internal mammary artery (IMA) and internal mammary vein (IMV) through the third interspace or by partial resection of the third intercostal cartilage.
a) Start lateral to avoid coming down into the IMA.
b) Remove cartilage to the sternocostal articulation.
ii. Can use large perforators from IMA and IMV if available.
iii. Alternative recipient: Thoracodorsal vessels.
c. Other technical points
i. If possible, should orient flap such that the thicker central adipose tissue forms the medial and inferior portions of the reconstructed breast.
ii. If preserved, can attach sensory nerves from the flap to an intercostal nerve.
iii. Flap is partially deepithelialized or deskinned depending on the amount of breast skin preserved.
iv. Zone IV is routinely discarded.
B. Anterolateral thigh flap (ALT or LCFAP-vl)
1. Indications: Often used in head and neck, upper and lower extremity reconstruction.
2. General features
a. Chimeric principle: Can raise multiple tissue components on different perforators from the lateral circumflex femoral axis.
i. Vastus lateralis muscle
ii. Tensor fascia lata
iii. Rectus femoris (RF) muscle
iv. Iliac crest
b. Mosaic flap principle: Can harvest an adjacent flap and anastomose it to a branch of the LCFA (e.g., groin flap, medial thigh flap).
c. Variations
i. Can raise flap with or without fascia.
ii. Can thin flap with one- or two-stage procedure to resurface shallow defects.
iii. Can use as a flow-through flap.
iv. Can use as an adipofascial flap.
v. Can be pedicled proximally for defects of perineum, lower abdominal wall, and greater trochanter.
vi. Can be pedicled distally for coverage around the knee.
d. Nerves: Can include anterior or lateral branch of lateral cutaneous nerve of the thigh to provide sensation.
e. Donor site
i. Can close primarily if flap width <8 cm.
ii. Alternatively, may repair with skin graft or V–Y local advancement flap.
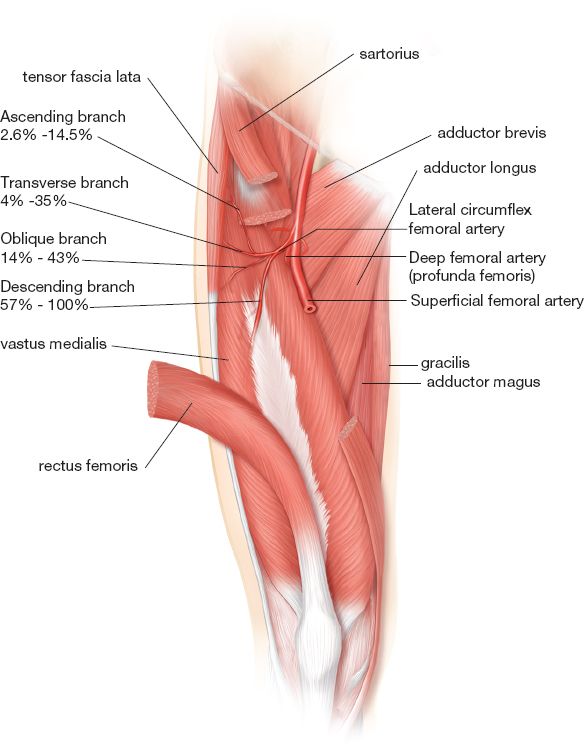
3. Anatomy (Fig. 5-2)
a. Perforators originate from descending branch of LCFA.
b. LCFA lies in the intermuscular septum between RF and VL muscles.
c. Pedicle length typically 8 to 16 cm, diameter >2 mm.
d. Can often find 1 to 3 perforators approximately 5 cm apart and 1.5 cm lateral to a line drawn connecting ASIS to superolateral patella. “Perforator B” is the perforator that is most consistently present, located around the midpoint.
4. Surgical technique
a. Can use Doppler to identify perforators preoperatively.
b. Design flap around perforator B with A and C perforators 5 cm proximal and distal to B perforator.
c. Make a longitudinal skin incision on medial side of flap, carrying on the dissection at the suprafascial level.
d. Enter the intermuscular septum distally between RF and VL to allow direct visualization of the descending branch and location of perforators.
e. May leave a cuff of muscle to minimize damage and spasm of the vessel.
f. Take care to preserve the motor branch.
g. Can incorporate the lateral femoral cutaneous nerve if a sensate flap is desired.
C. Thoracodorsal artery perforator flap (TAP)
1. General
a. Can use as a perforator flap, muscle flap, chimeric flap pedicled on thoracodorsal vessels, flow-through flap, or osteocutaneous flap with a segment of vascularized scapula.
b. Donor site can be closed for a flap width up to 10 cm.
c. If sensate flap is desired, can include lateral branch of intercostal nerve.
Figure 5-2. Vascular anatomy of the anterolateral thigh (ALT) and anterior thigh musculature. The descending branch of the lateral circumflex femoral artery (LCFA) is the dominant vascular supply to the ALT flap in 57% to 100% of cases.
2. Anatomy: Descending branch of the thoracodorsal artery has the largest and most reliable perforating vessels.
a. Found along a line about 2 cm behind anterior border of latissimus dorsi muscle edge.
b. Perforators are located within 8 cm of neurovascular hilum and 4 cm inferior to tip of scapula.
3. Surgical technique: With patient in lateral decubitus position, make incision just anterior to the anterior border of latissimus, which enables incorporation of a septocutaneous or musculocutaneous perforator.
D. SGAP flap
1. General
a. Advantages: Low donor site morbidity, longer vascular pedicle than the musculocutaneous flap, avoids need for vein grafts, abundance of adipose tissue even in thin patients, hidden scar, and good projection of the reconstructed breast.
b. Donor site can be closed for flap widths up to 12 cm
c. Flap length usually 24 to 26 cm.
d. Potential for sensory reinnervation with nervi clunium superioris
2. Anatomy
a. Usually three perforators supply the SGA cutaneous territory
b. Pedicle length 3 to 8 cm.
c. SGA usually emerges from edge of sacrum approximately one-third of distance along a line drawn from the posterior superior iliac spine (PSIS) to the greater trochanter.
3. Surgical technique
a. Identify perforators from SGA along a line drawn connecting PSIS and greater trochanter using Doppler.
b. Horizontal flaps produce a more favorable scar.
c. Flap is elevated from the muscle in the subfascial plane.
d. Perforators are approached from lateral to medial.
e. Usually a single large perforator is used.
f. When dissecting the pedicle, must eventually open the sacral fascia and ligate multiple communicating arterial and venous branches.
E. Inferior gluteal artery perforator flap
1. Indications: Similar to SGAP flap
2. Anatomy
a. Usually has two to four perforators originating from inferior gluteal artery (IGA) supplying the cutaneous territory.
b. Pedicle 7 to 10 cm.
3. Surgical technique
a. Inferior limit of the flap is 1 cm inferior and parallel to the gluteal fold with the patient in standing position.
b. With the patient in lateral decubitus position, perforators are identified with Doppler.
c. Flap is elevated from muscle in subfascial plane.
d. Approach perforators from lateral to medial.
e. No need to expose sciatic nerve.
f. Should preserve the posterior femoral cutaneous nerve and the fat overlying the ischium medially.
g. When dissecting the pedicle, one must eventually open the sacral fascia and ligate multiple communicating arterial and venous branches.
PEARLS
1. Perforator flaps are useful reconstructive tools as pedicled flaps, pedicled flaps in staged reconstruction, and as free tissue transfer.
2. Donor site morbidity should be considered when planning reconstructive options, and closure may require local tissue rearrangement or grafting.
3. A dogmatic, “cook-book” approach to perforator flaps should be avoided, and a detailed understanding of vascular anatomy allows the surgeon to modify these flaps to fit a multitude of reconstructive needs.
QUESTIONS YOU WILL BE ASKED
1. What are the advantages of perforator flaps?
Reduced donor site morbidity, decreased postoperative pain, faster recovery, easier to tailor or thin for covering or filling defects, and has longer pedicle than the parent musculocutaneous flap.
2. What is the difference between a direct and an indirect perforator?
Direct cutaneous perforators pierce the deep fascia to supply the skin without traversing any other structural tissues, whereas indirect perforators traverse an intermediate structure (i.e. muscle) prior to piercing the deep fascia and supplying the skin.
3. What perforator flap options are available for breast reconstruction?
Options include the DIEP (deep inferior epigastric perforator), SIEA (superficial interior epigastric artery), TUG (transverse upper gracilis), TAP/TDAP (thoracodorsal artery perforator), SGAP (superior gluteal artery perforator), IGAP (inferior gluteal artery perforator), and LAP (lumbar artery perforator) flaps.
THINGS TO DRAW
1. Blood supply to the rectus abdominis muscle
2. Blood supply to SGAP flap
Recommended Readings
Saint-Cyr M, Schaverien MV, Rohrich RJ. Perforator flaps: history, controversies, physiology, anatomy, and use in reconstruction. Plast Reconstr Surg. 2009;123(4):132e–145e. PMID: 19337067.
Sinna R, Boloorchi A, Mahajan AL, Qassemyar Q, Robbe M. What should define a perforator flap? Plast Reconstr Surg. 2010;126(6):2258–2263. PMID: 21124168.
Wallace CG, Kao HK, Jeng SF, Wei FC. Free-style flaps: a further step forward for perforator flap surgery. Plast Reconstr Surg. 2009;124(6):e419–426. PMID: 19952709.
< div class='tao-gold-member'>