■ Deep to the muscles is the posterior rectus fascia made up of the transversus fascia and internal oblique muscle fascia above the arcuate line and the transversus fascia below the arcuate line.
■ The paired rectus muscles originate from the pubic bone and extend to the cartilage of the 6th, 7th and 8th ribs. The blood supply comes from the dominant deep inferior epigastric artery and the superior epigastric artery (FIG 2). Additional blood supply comes from the posterior perforating vessels accompanying the 8th through 12th intercostal neurovascular bundles.
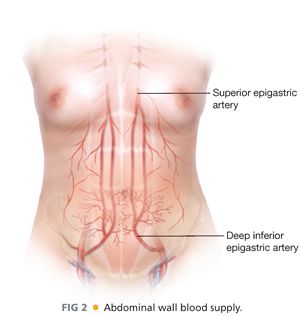
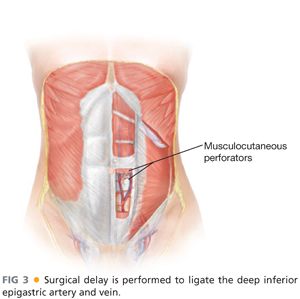
■ Within the muscle, the superior and inferior epigastric arteries may not have direct anastomoses under normal conditions. These connections are made or increased with surgical delay of the deep inferior epigastric artery.
■ Musculocutaneous perforators pass through the muscle and anterior rectus fascia (FIG 3). They are often gathered in the periumbilical area and in mirrored medial and lateral rows of perforators. The medial and lateral row of perforators on a given side is separated by approximately 1.5 to 2 cm. In the case of the pedicled TRAM flap, the flap is based on the superior epigastric vessels.
SURGICAL MANAGEMENT
Preoperative Planning
■ For high-risk patients, ligation of the inferior epigastric artery (surgical delay) should be considered. Surgical delay of the inferior epigastric artery is performed 10 to 14 days prior to the mastectomy. This is often performed at the time of sentinel lymph node biopsy in order to limit events requiring anesthesia.
■ On the day of reconstruction, the patient is marked first in the standing position. At the breast, the inframammary fold (IMF), midline and a line 1 cm off the midline on either side, the lateral breast extension, and proposed or prior mastectomy skin incision approach are marked. The width of the proposed breast reconstruction is measured as this will guide the ideal width of the abdominal flap, which is particularly important in delayed breast reconstruction where there is often a paucity of breast skin (FIG 4).
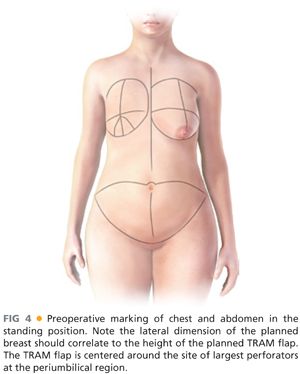
■ On the abdomen, the midline is marked and an ellipse of skin including the umbilicus is marked. In our experience, all patients offer at least 13 cm in width of the ellipse and this can be assessed with a pinch test (FIG 4).
■ The patient is then seated and any further extensions of the incisions are laterally marked to remove any “dog ear.”
TECHNIQUES
■ Perioperative antibiotics are provided and a Foley catheter and sequential compression device (SCD) boots are placed.
■ The flap can be raised while the mastectomy is being performed. No tumescence is used. The superior incision is made first, and the upper abdominal wall is raised to the level of the costochondral cartilages. On the side of the planned reconstruction, a tunnel is made through the IMF into the mastectomy pocket that fits a fist and the planned flap.
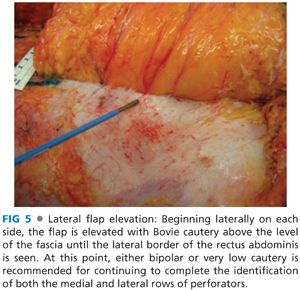
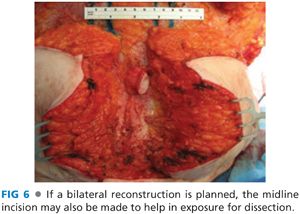
■ The patient is then flexed and the superior abdominal flap brought down to verify its pending closure and the possible height of the flap to be created. The inferior incision is then made. Beginning laterally on each side, the flap is then elevated with electrocautery above the level of the fascia until the lateral border of the rectus abdominis is seen. At this point, either bipolar or very low cautery is recommended for continuing to complete the identification of both the medial and lateral rows of perforators (FIG 5). If a bilateral reconstruction is planned, the midline incision may also be made to help in exposure for dissection (FIG 6). No perforators should be sacrificed at this time.
■ Once all perforators have been identified, the flap vascularity is assessed. In unilateral reconstruction cases, if one flap has a heartier blood supply, this flap is chosen.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree