■ The artery then divides into the medial (also known as transverse) and the lateral (also known as vertical or descending) branches. The medial branch is located approximately 3.5 cm below and parallel to the superior border. The lateral branch is located approximately 2.6 cm medial and parallel to the lateral border. The serratus branch (artery to the serratus anterior), which joins the thoracodorsal artery just before its entrance to the latissimus muscle, is a useful landmark as it guides one directly to the thoracodorsal pedicle. There is usually a single vena comitans of the thoracodorsal artery.8,9
■ The thoracodorsal motor nerve enters the muscle with the vascular pedicle. Cutaneous sensory nerves arise from the intercostal nerves at the midaxillary line and also in the paraspinal region.
PATIENT HISTORY AND PHYSICAL FINDINGS
■ A thorough history and physical examination are critical in preparing for reconstruction.
■ Pertinent aspects of the history include previous axillary operations (e.g., lymph node dissections or biopsies) and medical conditions that would preclude patients from an operation of moderate length under general anesthesia.
■ Certain patients (e.g., paraplegic or wheelchair-dependent individuals who cannot afford even a minimal weakening of shoulder strength) probably should not undergo latissimus dorsi breast reconstruction. The average patient, however, will likely not notice a difference in shoulder function after a period of full recovery.
■ A focused exam of the axilla and back for scars that may preclude use of the muscle flap or affect placement of the skin paddle is necessary.
■ The presence of a viable and innervated muscle may be confirmed by having the patient activate the muscle by placing the hands on the hips and pushing firmly. However, a vigorous muscle contraction does not necessarily indicate an intact thoracodorsal arterial pedicle, as the nerve is quite separated from the thoracodorsal artery proximal to the branch point from the subscapular artery and could be potentially preserved despite ligation of the thoracodorsal artery.
■ A team-based approach involving surgeons, anesthesiologists, primary care physicians, and other specialists such as cardiologists when needed ensures that patients are evaluated as a whole and all key concerns are addressed.
IMAGING AND OTHER DIAGNOSTIC STUDIES
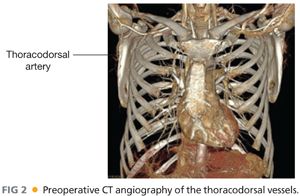
■ Preoperative computed tomography (CT) angiography of the donor site (FIG 2) is recommended in patients with previous surgical procedures during which the thoracodorsal arterial pedicle may have been sacrificed (e.g., axillary lymph node dissection or modified radical mastectomy).
SURGICAL MANAGEMENT
■ In consulting with patients, decisions about the timing of reconstruction (immediately after mastectomy or delayed) and the type of reconstruction are made taking patient factors and tumor characteristics into consideration.
■ Patient factors of significance include the following:
■ Patient preference
■ Smoking history
■ History of previous axillary operations that compromise the vascular pedicle of the donor site
■ Medical comorbidities that would preclude patients from undergoing an operation of moderate length.
■ Tumor characteristics as they relate to the following:
■ The need for postmastectomy radiation therapy
■ The need for close postmastectomy surveillance prior to reconstruction
■ In general, patients known to require postmastectomy radiation therapy are reconstructed in a delayed fashion to avoid the detrimental effects of radiation on flaps. A history of radiation therapy also serves as a relative indication for use of an autologous form of reconstruction, as implant-only reconstructions in the setting of radiation are prone to higher rates of complications and failure.
Preoperative Planning
■ Basic labs (chemistry and blood counts)
■ All anticoagulant and antiplatelet medications should be stopped a week prior to the operation. Warfarin can be bridged with enoxaparin a week prior.
■ Smokers are required to quit for a minimum of 4 weeks prior.
■ Patients receive preoperative antibiotics with intraoperative redosing.
■ Patients receive deep vein thrombosis (DVT) prophylaxis with use of a pneumatic compression device at the beginning of the case; preoperative subcutaneous heparin is not typically used in our practice.
■ A Foley catheter will be needed, given the length of the case.
■ A headlight may be helpful in the harvest of the latissimus dorsi muscle.
■ A beanbag is needed for lateral decubitus positioning.
■ A sterile Doppler probe is helpful to have available in case there is any concern for the location or integrity of the thoracodorsal pedicle during the case.
Positioning
Marking/positioning
■ The inframammary fold (IMF), medial limit, and lateral limit of the breast should be marked with the patient upright.
■ With the patient in the sitting position, have the patient activate the latissimus muscle (by placing hands on the hips and coughing) and mark anterolateral margin of the muscle.
■ Other key landmarks for the limits of the latissimus muscle are the tip of scapula, vertebral column, and posterior iliac crest. They should be marked for additional orientation.
■ The pivot point for the flap is the approximate pedicle location: It should be marked 2 to 3 cm medial to lateral border and 9 cm below the apex of the axilla.
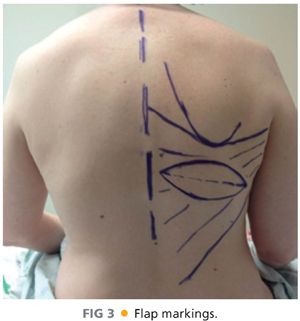
■ Eight to 10-cm–wide skin paddles can generally be closed primarily (verify adequate skin laxity by pinching). The skin paddle must be placed over the muscular portion of the latissimus, as the vascularity of the skin over the thoracolumbar fascia is notoriously poor. In most patients, it is necessary to stay at least 8 cm superior to the posterior iliac crest to avoid the thoracolumbar fascia (FIG 3).
■ Verify that the skin paddle has been designed correctly for rotating to the planned anterior position by measuring from the estimated pedicle pivot point to the inferolateral tip of the skin paddle. This distance must equal the distance from the pivot point to the medial limit of your planned mastectomy incision.
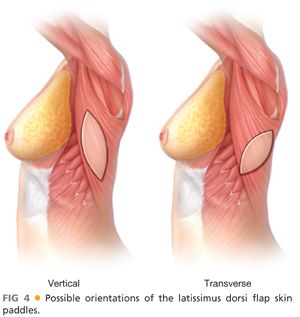
■ The orientation of the axis of the skin paddle can be varied (FIG 4). A horizontally oriented skin paddle allows the scar to be hidden by a bra strap but may limit the size of the paddle harvested.
■ Measure the breast base width to guide your choice of tissue expander size.
■ Patient positioning varies by surgeon. Harvesting a full latissimus dorsi flap requires a lateral decubitus position with a special arm support for the ipsilateral arm and an axillary roll under the contralateral axilla to prevent brachial plexopathy. The lower extremities will also require adequate padding.
■ Placing patients in the supine position during the earlier or latter parts of the case is based on surgeon preference and laterality of reconstruction (unilateral vs. bilateral). Bilateral procedures absolutely require position changes.
■ The description in the following text will include multiple position changes to make clear the sequence of events for the procedure. This sequence can then be modified.
TECHNIQUES
RECIPIENT SITE PREPARATION (IN EITHER SUPINE OR LATERAL POSITION)
■ Develop the recipient site with the patient in supine position: Elevate the skin and subcutaneous flaps off the pectoralis major to recreate the mastectomy defect in cases of delayed reconstruction; for immediate reconstruction, the mastectomy skin flaps are already developed by the breast surgeon.
■ Natural borders of the breast should be preserved, including the IMF and skin adherence to the sternum along the midline. A possible exception would be in delayed reconstruction where the inferior dissection can extend approximately 0.5 to 1.0 cm inferior to the IMF to allow the expander to sit at the IMF after the latissimus is inset.
■ Limit the lateral dissection, when possible, to the anterior axillary line with the exception of a three to four fingerbreadths tunnel created to allow for transfer of the flap. This tunnel should not violate the IMF.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree