8 Patient safety in plastic surgery
Synopsis
 Modern medicine has greatly reduced the risk of surgery.
Modern medicine has greatly reduced the risk of surgery.
 Identifying which patients are at greatest risk for surgery starts the risk reduction process.
Identifying which patients are at greatest risk for surgery starts the risk reduction process.
 Identification of medical factors leading to complications helps prevent untoward outcomes.
Identification of medical factors leading to complications helps prevent untoward outcomes.
 Specialized care for the liposuction patient.
Specialized care for the liposuction patient.
 Specialized care for the patient having facial aesthetic surgery.
Specialized care for the patient having facial aesthetic surgery.
 Avoiding fire in the operating room.
Avoiding fire in the operating room.
 Protocol-based systems for risk reduction.
Protocol-based systems for risk reduction.
 Reducing patient risk through optimal patient care.
Reducing patient risk through optimal patient care.
The risk of having surgery
Prior to the introduction of anesthesia the surgical experience was a decidedly unpleasant one for the patient. The success of a surgical procedure (read: survival) was often based on the speed at which the procedure was accomplished. If nothing else, the introduction of anesthetic techniques brought the ability of the surgical team to take more time in accomplishing the procedure. The introduction of an additional medical intervention (anesthesia) on the patient brought additional undesired effects and perioperative death.1,2 Since the introduction of general and regional anesthesia as part of normal surgical practice, surgical and anesthetic complication rates have been analyzed using a variety of clinical criteria. It is this wide variety of criteria that has led to confusion in the medical literature and in the mind of practicing clinicians of the actual risk attributable to anesthesia care during a surgical intervention. Do we consider in our complication rate only events that happened during the actual surgical procedure? Do we only consider events attributed solely to providing anesthesia or do we consider the contribution of surgery to the untoward outcome?3 The time course for evaluation of surgical and anesthetic complications remains controversial and almost certainly is related to the nature of the surgical procedure and type of anesthesia, if any, that was used during surgery. The wide variety of time indices that are used in the medical literature for the study of perioperative complications makes comparison of studies very difficult. Definitions of the time period for study of perioperative mortality range from 48 hours, as defined by the Joint Commission on Accreditation of Healthcare Organizations, to 30 days, as defined by the American College of Surgeons. Similarly, the inability to compare clinical studies adds to the confusion in defining clinical risk to the patient from a given surgical or anesthetic technique. For anesthetic risk we need to consider not only cases where anesthesia is deemed the sole cause of complication and mortality but also cases where anesthesia is a significant contributing factor of complications and mortality.
It remains extremely difficult, even with review of the extensive body of medical literature, to predict accurately the risk for any given patient who is about to undergo any given surgical procedure. We can safely claim that complications from anesthesia have been greatly reduced since the widespread acceptance of anesthesia techniques. Beecher and Todd published in 1954 that, where anesthesia was a very important contributing factor, death occurred in 1 : 1560 surgeries.4 Today, patients want to know the current state of the art of medical science in regard to perioperative risk and complication. One of the most useful and popular ways to assess risk in the surgical patient population is by the American Society of Anesthesiologists (ASA) physical status. This classification system was originally designed in the early 1940s and updated in 1961 (Table 8.1).
| ASA I | Normal healthy patient without active disease |
| ASA II | Patient with mild systemic disease (e.g., hypertension under medical control) |
| ASA III | Patient with severe systemic disease |
| ASA IV | Patient with severe systemic disease that is a constant threat to life |
| ASA V | Patient who is moribund and is not expected to survive without surgery |
| ASA VI | Patient who has been declared brain-dead for organ donation |
ASA, American Society of Anesthesiologists.
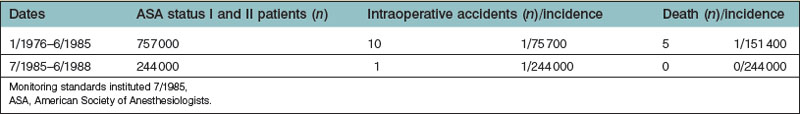
The ASA classification system has been shown to correlate with surgical and anesthetic outcome.5 Lagasse’s study5 concluded that the incidence of anesthesia-related mortality within 48 hours of surgery was 1 : 13 000 procedures, when evaluating all patients coming for a surgical procedure. Of great interest, but of little surprise to the practicing anesthesiologist, was that anesthesia-related deaths increased with increasing ASA classification. Other reports dating as far back as 1987 report anesthesia-related mortality rates at 1 : 185 000.6 The study by Buck et al.6 was performed before the widespread acceptance of new technology monitoring systems (pulse oximetry and capnography) that serve as early-warning systems for respiratory compromise. More recent studies have shown even better safety outcome results for patients having surgery. A 2004 study performed in France again showed that mortality rates increased with increasing patient ASA status, at a rate of 4 deaths per million surgeries for ASA category I patients and with 554 deaths per million in ASA category IV patients.7 The effect of medical progress on improved clinical outcome is often difficult to detect when the incidence of maloccurrence is infrequent. Significant changes in daily anesthesia practice began in the mid-1980s with the introduction of the Harvard Standards of Practice I – minimal monitoring. These anesthesia standards required the use of monitoring devices to detect and prevent impending disaster during surgery.8 The 1986 ASA standards for basic intraoperative monitoring encourage both capnography and pulse oximetry during conduct of anesthesia and surgery. The incidence of accident and death rate in ASA status I and II patients was studied before and after the adoption of the new monitoring standards at Harvard hospitals (Table 8.2). The implementation of these standards, along with the introduction of new monitoring techniques, has greatly reduced the incidence of unrecognized hypoventilation and hypoxemia leading to intraoperative complication and death.9–11
It is the experience gained from in-hospital surgery and advances in medical care that have allowed the development of outpatient surgery. Recent data show that upwards of 60% of surgery at community hospitals in 2005 was performed in an outpatient setting.12 It is almost certain the percentage of patients undergoing cosmetic and reconstructive surgery on an outpatient basis is even higher. In the mid-1970s there were two free-standing outpatient surgery centers in the US. There are now over 5000. The success of outpatient surgery done outside a hospital operating room is based on the cost-efficient ability of these centers to meet the medical needs of the patient and the medical staff safely. It has been shown repeatedly that outpatient surgery can be performed with a safety standard equal to or exceeding that available in an inpatient hospital-based environment. The spectrum of settings for performance of surgery continues to expand with the development of office-based surgical facilities.13 The American Society of Plastic Surgery through the Patient Safety committee has published an outstanding series of articles outlining advisory principles for safety in ambulatory surgery.14 These reports, based on the medical literature combined with the general principles described above, set an educated guideline for conduct of outpatient plastic surgery. A primary area of concern for the plastic surgeon is patient selection for surgery and whether or not to perform the surgery on an outpatient basis. We have previously described the data that demonstrate that complications increase with an increase in a patient’s ASA status. Prospective stratification of 17 638 patients by age found that patients over the age of 65 years were 1.4 times as likely to have an untoward intraoperative event and twice as likely to experience an intraoperative cardiovascular event as patients under 65.15
Obese patients/sleep apnea patients having plastic surgery
Multiple studies have demonstrated an increase in perioperative risk associated with obesity. Complications during surgery associated with patient obesity include increased rates of failed regional anesthesia, unplanned hospital admissions, and an increased incidence of deep venous thrombosis.16 It is also unreasonable to expect medical care providers to be able to manage the obese patient physically without assistance from other healthcare assistants. Unless an ambulatory center is prepared to have the help the obese patient will require, the patient should have surgery in a facility with the necessary staff available. Setting a weight limit for patients, based on the ability of the staff of the center to manage the patient, avoids uncomfortable situations when the patient arrives for surgery and the facility is unable to take care of him or her. Proper planning at the surgical facility reduces surgical cancelations. Obese patients have a higher incidence of sleep apnea than patients of normal body habitus. Physical characteristics that predispose patients to having obstructive sleep apnea include body mass index over 35, neck circumference of 17 inches (43 cm) in men or 16 inches (41 cm) in women, craniofacial abnormalities affecting the airway, nasal obstruction, and tonsil hypertrophy.17
The 2006 report by the ASA taskforce on perioperative management of patients with obstructive sleep apnea is a valuable reference for conduct of care of this classification of patients.17 The severity of sleep apnea, as determined by a formal sleep study, is seen in Table 8.3. The severity of oxygen saturation depression during apnea events and the number of apneic events per hour should be considered in evaluating the patient for surgery.
Table 8.3 Criteria for determining the severity of sleep apnea after sleep study
| Severity of obstructive sleep apnea | Adult apnea–hypopnea index | Pediatric apnea–hypopnea index |
|---|---|---|
| None | 0–5 | 0 |
| Mild | 6–20 | 1–5 |
| Moderate | 21–40 | 6–10 |
| Severe | >40 | >10 |
Proper perioperative clinical management of patients with sleep apnea is of critical importance. Airway management of the obese patient, with or without sleep apnea, may be difficult. Careful airway evaluation preoperatively with notation of mouth opening, mental–hyoid distance, submandibular compliance, range of motion of the cervical spine, and Mallampati score may indicate potential difficulties in airway maintenance and intubation.18 Conduct of the actual anesthetic for patients having sleep apnea and having plastic surgery depends on many factors. Certainly the type of surgery, the severity of airway disease, and the desires of the patient are major components in the decision-making process. The need for intubation or airway manipulation during surgery should not be an automatic exclusionary criterion for outpatient surgery in a patient with a history of sleep apnea. Appropriately selected patients with a history of sleep apnea who are observed and monitored for extended periods of time after surgery may do well on an outpatient basis. Patients with sleep apnea requiring large amounts of postoperative narcotics or sedatives and those who are noted to have decreased oxygen saturation levels on room air or inadequate ventilation will require admission and continued monitoring in an acute care setting. Monitoring of the sleep apnea patient after surgery and after hospital admission includes continuous oxygen saturation. Monitoring of oxygen saturation levels on an every 4–6-hour basis makes no sense given the fact that obstructive apneic events are more likely after surgery and hypoxic brain injury may occur in a matter of minutes.
In addition, it may be unwise to attempt to complete a surgical procedure on a patient with sleep apnea using local anesthesia with deep levels of sedation. Commonly used medications for sedation during surgery, including narcotics and benzodiazepines, may exacerbate apneic episodes leading to hypoxia and hypoventilation. Performing procedures on a patient with sleep apnea with the patient in the prone position and limited airway access without first securing the airway may be particularly hazardous. It is often difficult to monitor ventilation accurately in a nonintubated patient. New technologies to detect hypoventilation will need to be developed to monitor ventilation accurately in nonairway-controlled patients. Development of continuous arterial CO2 using a noninvasive format will further improve patient safety during surgery.19 Patients using continuous positive airway pressure (CPAP) as a therapeutic modality for sleep apnea should be instructed to bring the CPAP equipment to the surgical center. The center should have personnel knowledgeable in the application of CPAP devices available to assist in the respiratory care of the patient. Similarly, patients who use CPAP at home should use their CPAP while resting or asleep at the hospital.
Review of large databases evaluating the safety of surgery has shown that surgery and anesthesia are very safe. The risk of anesthesia as the cause of death in ASA I and ASA II category patients is in the range of 1 : 150 000–1 : 300 000 patients.20,21 Therefore, it should be no surprise when medical publications are presented with a small series of patients undergoing outpatient surgery in an office-based surgery center that the reported complication and death rates are very low.22 In a study on office-based surgery, 84.3% of patients were ASA class I, 15.6% ASA II, and only 0.1% ASA class III. It would require a very large data collection of ASA I and II patients to provide evidence of increased risk or an improved outcome in a particular surgical setting or using a specific anesthesia technique in this subset of patients.
Similar publications have documented the highest levels of safety in the office surgery environment using general anesthesia. Hoefflin et al. published a series of 23 000 consecutive surgical patients over an 18-year period. The advantages of general anesthesia with airway control during surgery are also presented.23 Again, given the relatively low incidence of complications in this patient population and the small number of patients studied, it will be difficult to show statistically significant change in clinical complication rates. The American Association for Accreditation of Ambulatory Surgery Facilities study of 400 675 patients concluded that patient safety in accredited office-based surgical facilities was equal to or exceeded the safety level of surgery in a hospital.24 As these articles propose, there are tangible benefits to office-based surgery, including cost containment, convenience, and ease of scheduling. There is little doubt that patients prefer the quieter, gentler ambience of the office/outpatient surgery center than a busy hospital environment. The office-based surgery/outpatient surgical environment can provide a superb surgical environment for patient, physician, and staff as long as the quality of care equals or exceeds that of the full service hospital in all regards.
Intraoperative management of the plastic surgery patient
Both the medical literature and nonpeer-reviewed publications extol the virtues of a variety of anesthesia techniques for plastic surgery, particular aesthetic surgery. The general public would like to believe that a less invasive and seemingly simpler anesthesia technique will be safer. Physicians who are not knowledgeable of the medical literature may contribute to this misconception. As we have seen in the case of patients with sleep apnea, local anesthesia with deep levels of sedation may not be an appropriate anesthetic choice and may put the patient at substantial risk of airway compromise. Both local anesthesia and general anesthesia produce a similar incidence of complications in patients having oral surgery on an outpatient basis.25,26 The 2006 closed claims analysis from the ASA Closed Claims database demonstrated that, relative to the incidence of the anesthesia technique, death during monitored anesthesia care and general anesthesia was twice as common as in patients undergoing a regional anesthetic.27 The primary complication leading to death in this study was inadequate oxygenation and ventilation. In this closed claim study, respiratory insufficiency was found to have occurred in 15% of patients who had monitored anesthesia care versus 7% of patient who had general anesthesia. Other factors in this group, such as patient age and ASA classification, may have contributed to the findings. Randomized studies comparing anesthesia technique for a given surgical procedure must be performed before declaring a winner in the category of anesthesia technique for patient safety. Very large patient populations will need to be evaluated so that appropriate conclusions can be drawn.
Advances in medical technology and medical practice have allowed the development of outpatient surgery to be performed in both a free-standing surgical center and in the medical office-based surgery setting. The American Society of Plastic Surgery commissioned a taskforce on patient safety in office-based surgical facilities and published a taskforce statement.28 This taskforce statement provides conservative judgments on the nature of surgical procedures appropriate for the office-based setting and the appropriate magnitude of these same surgeries. Of particular interest to the practicing physician was the recommendation for limiting the volume of liposuction to a total of 5000 cc of total aspirate volume (fat and fluid). A large study looking at the clinical outcome of 631 large-volume liposuction patients showed a high degree of safety and extremely low complication rates with much larger total aspirate volume.29
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree